Abstract
Objectives
To prospectively assess the frequency of severe abdominal pain during and after transarterial chemoembolization (TACE) for hepatocellular carcinoma (HCC) using the visual analog scale (VAS), and to identify predictive factors.
Methods
Ninety-eight TACE performed in 80 patients (mean 65 ± 12 years old, 60 men) were consecutively and prospectively included. Abdominal pain was considered severe if the VAS ≥ 30/100 after treatment administration, or if opioid analgesic (grades 2–3) intake was required during hospitalization. Patient and tumor characteristics as well as technical factors associated with severe pain were identified by binary logistic regression.
Results
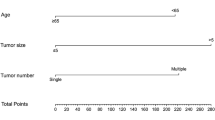
The criterion for severe pain was met in 41/98 (42%) of procedures (peri-procedural pain 30/98 [31%] and opioid consumption during hospitalization 24/98 [25%]). Multivariate analysis identified age (odds ratio [OR] = 0.943 (95% confidence interval 0.895–0.994), p = 0.029), cirrhosis (OR = 0.284 (0.083–0.971), p = 0.045), and alcoholic liver disease (OR = 0.081 (0.010–0.659), p = 0.019) as negative predictive factors of severe abdominal pain. Severe abdominal pain occurred in or after 1/13 (8%), 8/34 (24%), 22/41 (54%), and 10/10 (100%) TACE sessions when none, one, two, and three of the protective factors were absent, respectively (p < 0.001). The area under the ROC curve of the combination of factors for the prediction of severe abdominal pain was 0.779 (CI 0.687–0.871).
Conclusion
Severe abdominal pain was frequent during and after TACE revealing a clinically relevant and underestimated problem. A predictive model based on three readily available clinical variables suggests that young patients without alcoholic liver disease or cirrhosis could benefit from reinforced analgesia.
Key Points
• Severe abdominal pain occurs in 43% of TACE for HCC.
• Younger age, absence of cirrhosis, and absence of alcoholic liver disease were identified as independent predictive factors of severe abdominal pain.
• A simple combination of the three abovementioned features helped predict the occurrence of severe abdominal pain.


Similar content being viewed by others
Change history
27 November 2020
A Correction to this paper has been published: https://doi.org/10.1007/s00330-020-07506-0
Abbreviations
- BCLC:
-
Barcelona Clinics Liver Cancer
- cTACE:
-
Conventional transarterial chemoembolization
- EASL:
-
European Association for the Study of the Liver
- EORTC:
-
European Organization for Research and Treatment of Cancer
- HCC:
-
Hepatocellular carcinoma
- OR:
-
Odds ratio
- PES:
-
Post-embolization syndrome
- TACE:
-
Transarterial chemoembolization
- VAS:
-
Visual analog scale
References
Forner A, Reig M, Bruix J (2018) Hepatocellular carcinoma. Lancet 391:1301–1314
European Association for the Study of the Liver (2018) EASL Clinical Practice guidelines: management of hepatocellular carcinoma. J Hepatol 69:182–236
Otto G, Herber S, Heise M et al (2006) Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl 12:1260–1267
Ravaioli M, Grazi GL, Piscaglia F et al (2008) Liver transplantation for hepatocellular carcinoma: results of down-staging in patients initially outside the Milan selection criteria. Am J Transplant 8:2547–2557
Llovet JM, Real MI, Montana X et al (2002) Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 359:1734–1739
Lo CM, Ngan H, Tso WK et al (2002) Randomized controlled trial of transarterial Lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 35:1164–1171
Llovet JM, Bruix J (2003) Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 37:429–442
Oliveri RS, Wetterslev J, Gluud C (2011) Transarterial (chemo) embolisation for unresectable hepatocellular carcinoma. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004787.pub2CD004787
Pomoni M, Malagari K, Moschouris H et al (2012) Post embolization syndrome in doxorubicin eluting chemoembolization with DC bead. Hepatogastroenterology 59:820–825
Bouvier A, Ozenne V, Aube C et al (2011) Transarterial chemoembolisation: effect of selectivity on tolerance, tumour response and survival. Eur Radiol 21:1719–1726
Golfieri R, Giampalma E, Renzulli M et al (2014) Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolisation for hepatocellular carcinoma. Br J Cancer 111:255–264
Leung DA, Goin JE, Sickles C, Raskay BJ, Soulen MC (2001) Determinants of postembolization syndrome after hepatic chemoembolization. J Vasc Interv Radiol 12:321–326
Benzakoun J, Ronot M, Lagadec M et al (2017) Risks factors for severe pain after selective liver transarterial chemoembolization. Liver Int 37:583–591
Lang EV, Benotsch EG, Fick LJ et al (2000) Adjunctive non-pharmacological analgesia for invasive medical procedures: a randomised trial. Lancet 355:1486–1490
European Association for the Study of the Liver (2018) EASL Clinical Practice guidelines: management of alcohol-related liver disease. J Hepatol 69:154–181
Yang H, Seon J, Sung PS et al (2017) Dexamethasone prophylaxis to alleviate postembolization syndrome after transarterial chemoembolization for hepatocellular carcinoma: a randomized, double-blinded, placebo-controlled study. J Vasc Interv Radiol 28:1503–1511 e1502
Guo JG, Zhao LP, Rao YF et al (2018) Novel multimodal analgesia regimen improves post-TACE pain in patients with hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int 17:510–516
Jensen KJ, Alpini G, Glaser S (2013) Hepatic nervous system and neurobiology of the liver. Compr Physiol 3:655–665
Novak DJ, Victor M (1974) The vagus and sympathetic nerves in alcoholic polyneuropathy. Arch Neurol 30:273–284
Lammer J, Malagari K, Vogl T et al (2009) Prospective randomized study of doxorubicin-eluting-bead embolization in the treatment of hepatocellular carcinoma: results of the PRECISION V study. Cardiovasc Intervent Radiol 33:41–52
Khalaf MH, Shah RP, Green V et al (2020) Comparison of opioid medication use after conventional chemoembolization versus drug-eluting embolic chemoembolization. J Vasc Interv Radiol. https://doi.org/10.1016/j.jvir.2020.04.018
Wang TC, Zhang ZS, Xiao YD (2020) Determination of risk factors for pain after transarterial chemoembolization with drug-eluting beads for hepatocellular carcinoma. J Pain Res 13:649–656
Hatsiopoulou O, Cohen RI, Lang EV (2003) Postprocedure pain management of interventional radiology patients. J Vasc Interv Radiol 14:1373–1385
Schupp CJ, Berbaum K, Berbaum M et al (2005) Pain and anxiety during interventional radiologic procedures: effect of patients’ state anxiety at baseline and modulation by nonpharmacologic analgesia adjuncts. J Vasc Interv Radiol 16:1585–1592
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Maxime Ronot.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The spelling of Lucas Raynaud’s name was incorrect.
Electronic supplementary material
ESM 1
(DOCX 161 kb)
Rights and permissions
About this article
Cite this article
Pachev, A., Raynaud, L., Paulatto, L. et al. Predictive factors of severe abdominal pain during and after transarterial chemoembolization for hepatocellular carcinoma. Eur Radiol 31, 3267–3275 (2021). https://doi.org/10.1007/s00330-020-07404-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07404-5