Abstract
Objectives
To assess the proportion of missed/misinterpreted imaging examinations of pancreatic ductal adenocarcinoma (PDAC), and their association with the diagnostic interval and survival.
Methods
Two hundred fifty-seven patients (mean age, 71.8 years) diagnosed with PDAC in 2014–2015 were identified from the Nova Scotia Cancer Registry. Demographics, stage, tumor location, and dates of initial presentation, diagnosis, and, if applicable, surgery and death were recorded. US, CT, and MRI examinations during the diagnostic interval were independently graded by two radiologists using the RADPEER system; discordance was resolved in consensus. Mean diagnostic interval and survival were compared amongst RADPEER groups (one-way ANOVA). Kaplan-Meier analysis was performed for age (< 65, 65–79, ≥ 80), sex, tumor location (proximal/distal), stage (I–IV), surgery (yes/no), chemotherapy (yes/no), and RADPEER score (1–3). Association between these covariates and survival was assessed (multivariate Cox proportion hazards model).
Results
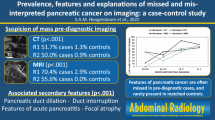
RADPEER 1–3 scores were assigned to 191, 27, and 39 patients, respectively. Mean diagnostic intervals were 53, 86, and 192 days, respectively (p = 0.018). There were only 3/257 (1.2%) survivors. Mean survival was not different between groups (p = 0.43). Kaplan-Meier analysis showed worse survival in RADPEER 1–2 (p = 0.007), older age (p < 0.001), distal PDAC (p = 0.016), stage (p < 0.0001), and no surgery (p < 0.001); survival was not different with sex (p = 0.083). Cox analysis showed better survival in RADPEER 3 (p = 0.005), women (p = 0.002), surgical patients (p < 0.001), and chemotherapy (p < 0.001), and worse survival in stage IV (p = 0.006).
Conclusion
Imaging-related delays occurred in one-fourth of patients and were associated with longer diagnostic intervals but not worse survival, potentially due to overall poor survival in the cohort.
Key Points
• One-fourth of patients (66/257, 25.7%) with pancreatic ductal adenocarcinoma (PDAC) underwent imaging examinations that demonstrated manifestations of the disease, but findings were either missed or misinterpreted; RADPEER 2 and 3 scores were assigned to 10.5% and 15.2% of patients, respectively.
• Patients with imaging examinations assigned RADPEER 3 scores were associated with significantly longer diagnostic intervals (192 ± 323 days) than RADPEER 1 (53 ± 86 days) and RADPEER 2 (86 ± 120 days) (p < 0.001).
• Imaging-related diagnostic delays were not associated with worse survival; however, this may have been confounded by the overall poor survival in our cohort (only 3/257 (1.2%) survivors).





Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- PDAC:
-
Pancreatic ductal adenocarcinoma
- US:
-
Ultrasound
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34
(2019) Canadian Cancer Statistics 2019. Canadian Cancer Society, Statistics Canada, Available at: http://cancer.ca/Canadian-Cancer-Statistics-2019-EN. Accessed 19 Feb 2020. pp 1–95
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM (2014) Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 74:2913–2921
(2017) Canadian Cancer Statistics 2017. Canadian Cancer Society, Statistics Canada, Available at: http://cancer.ca/en/cancer-information/cancer-101/canadian-cancer-statistics-publication/past-editions-canadian-cancer-statistics/?region=on. Accessed 19 Feb 2020. pp 1–142
Kulkarni NM, Soloff EV, Tolat PP et al (2019) White paper on pancreatic ductal adenocarcinoma from society of abdominal radiology’s disease-focused panel for pancreatic ductal adenocarcinoma: part I, AJCC staging system, NCCN guidelines, and borderline resectable disease. Abdom Radiol (NY). https://doi.org/10.1007/s00261-019-02289-5
Hidalgo M (2010) Pancreatic cancer. N Engl J Med 362:1605–1617
Swords DS, Mone MC, Zhang C, Presson AP, Mulvihill SJ, Scaife CL (2015) Initial misdiagnosis of proximal pancreatic adenocarcinoma is associated with delay in diagnosis and advanced stage at presentation. J Gastrointest Surg 19:1813–1821
Gobbi PG, Bergonzi M, Comelli M et al (2013) The prognostic role of time to diagnosis and presenting symptoms in patients with pancreatic cancer. Cancer Epidemiol 37:186–190
Glant JA, Waters JA, House MG et al (2011) Does the interval from imaging to operation affect the rate of unanticipated metastasis encountered during operation for pancreatic adenocarcinoma? Surgery 150:607–616
Weller D, Vedsted P, Rubin G et al (2012) The Aarhus statement: improving design and reporting of studies on early cancer diagnosis. Br J Cancer 106:1262–1267
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Harris PA, Taylor R, Minor BL et al (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208
Goldberg-Stein S, Frigini LA, Long S et al (2017) ACR RADPEER committee white paper with 2016 updates: revised scoring system, new classifications, self-review, and subspecialized reports. J Am Coll Radiol 14:1080–1086
Core Team R (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria
Deshwar AB, Sugar E, Torto D et al (2018) Diagnostic intervals and pancreatic ductal adenocarcinoma (PDAC) resectability: a single-center retrospective analysis. Ann Pancreat Cancer 1:1–8
Walters DM, Lapar DJ, de Lange EE et al (2011) Pancreas-protocol imaging at a high-volume center leads to improved preoperative staging of pancreatic ductal adenocarcinoma. Ann Surg Oncol 18:2764–2771
Gangi S, Fletcher JG, Nathan MA et al (2004) Time interval between abnormalities seen on CT and the clinical diagnosis of pancreatic cancer: retrospective review of CT scans obtained before diagnosis. AJR Am J Roentgenol 182:897–903
Ahn SS, Kim MJ, Choi JY, Hong HS, Chung YE, Lim JS (2009) Indicative findings of pancreatic cancer in prediagnostic CT. Eur Radiol 19:2448–2455
Jang KM, Kim SH, Kim YK, Song KD, Lee SJ, Choi D (2015) Missed pancreatic ductal adenocarcinoma: assessment of early imaging findings on prediagnostic magnetic resonance imaging. Eur J Radiol 84:1473–1479
Gonoi W, Hayashi TY, Okuma H et al (2017) Development of pancreatic cancer is predictable well in advance using contrast-enhanced CT: a case-cohort study. Eur Radiol 27:4941–4950
Kalbhen CL, Yetter EM, Olson MC, Posniak HV, Aranha GV (1998) Assessing the resectability of pancreatic carcinoma: the value of reinterpreting abdominal CT performed at other institutions. AJR Am J Roentgenol 171:1571–1576
Pawlik TM, Laheru D, Hruban RH et al (2008) Evaluating the impact of a single-day multidisciplinary clinic on the management of pancreatic cancer. Ann Surg Oncol 15:2081–2088
Shetty AS, Mittal A, Salter A, Narra VR, Fowler KJ (2018) Journal club: hepatopancreaticobiliary imaging second-opinion consultations: is there value in the second reading? AJR Am J Roentgenol 211:1264–1272
Acknowledgments
The authors thank Candice Crocker, PhD, for assistance with institutional research ethics board submission.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Andreu Costa, MD MSc FRCPC.
Conflict of interest
Jessie Kang, Sharon Clarke, Mohammed Abdolell, Ravi Ramjeesingh, Jennifer Payne, and Andreu Costa declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Statistical analysis was performed by a biostatistician, Mohammed Abdolell.
Informed consent
The need for informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• observational
• Multi-institutional
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kang, J., Clarke, S.E., Abdolell, M. et al. The implications of missed or misinterpreted cases of pancreatic ductal adenocarcinoma on imaging: a multi-centered population-based study. Eur Radiol 31, 212–221 (2021). https://doi.org/10.1007/s00330-020-07120-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-020-07120-0