Abstract
Objective
To develop a deep learning algorithm that can rule out significant rotator cuff tear based on conventional shoulder radiographs in patients suspected of rotator cuff tear.
Methods
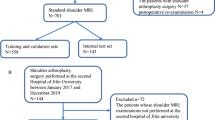
The algorithm was developed using 6793 shoulder radiograph series performed between January 2015 and June 2018, which were labeled based on ultrasound or MRI conducted within 90 days, and clinical information (age, sex, dominant side, history of trauma, degree of pain). The output was the probability of significant rotator cuff tear (supraspinatus/infraspinatus complex tear with > 50% of tendon thickness). An operating point corresponding to sensitivity of 98% was set to achieve high negative predictive value (NPV) and low negative likelihood ratio (LR−). The performance of the algorithm was tested with 1095 radiograph series performed between July and December 2018. Subgroup analysis using Fisher’s exact test was performed to identify factors (clinical information, radiography vendor, advanced imaging modality) associated with negative test results and NPV.
Results
Sensitivity, NPV, and LR− were 97.3%, 96.6%, and 0.06, respectively. The deep learning algorithm could rule out significant rotator cuff tear in about 30% of patients suspected of rotator cuff tear. The subgroup analysis showed that age < 60 years (p < 0.001), non-dominant side (p < 0.001), absence of trauma history (p = 0.001), and ultrasound examination (p < 0.001) were associated with negative test results. NPVs were higher in patients with age < 60 years (p = 0.024) and examined with ultrasound (p < 0.001).
Conclusion
The deep learning algorithm could accurately rule out significant rotator cuff tear based on shoulder radiographs.
Key Points
• The deep learning algorithm can rule out significant rotator cuff tear with a negative likelihood ratio of 0.06 and a negative predictive value of 96.6%.
• The deep learning algorithm can guide patients with significant rotator cuff tear to additional shoulder ultrasound or MRI with a sensitivity of 97.3%.
• The deep learning algorithm could rule out significant rotator cuff tear in about 30% of patients with clinically suspected rotator cuff tear.


Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the receiver operating characteristic curve
- CNN:
-
Convolutional neural network
- Cutoff98% :
-
Cutoff point for an expected sensitivity of 98%
- Cutoffoptimal :
-
Optimal cutoff point determined by Youden’s J statistic
- DICOM:
-
Digital Imaging and Communications in Medicine
- FCN:
-
Fully connected network
- NPV:
-
Negative predictive value
- VAS:
-
Visual analog scale
References
de Jesus JO, Parker L, Frangos AJ, Nazarian LN (2009) Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol 192:1701–1707
Roy JS, Braen C, Leblond J et al (2015) Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: a systematic review and meta-analysis. Br J Sports Med 49:1316–1328
Amini B, Beckmann NM, Beaman FD et al (2018) ACR Appropriateness Criteria® shoulder pain-traumatic. J Am Coll Radiol 15:S171–S188
Small KM, Adler RS, Shah SH et al (2018) ACR Appropriateness Criteria® shoulder pain—atraumatic. J Am Coll Radiol 15:S388–S402
Pearsall AW 4th, Bonsell S, Heitman RJ, Helms CA, Osbahr D, Speer KP (2003) Radiographic findings associated with symptomatic rotator cuff tears. J Shoulder Elbow Surg 12:122–127
Hardy DC, Vogler JB 3rd, White RH (1986) The shoulder impingement syndrome: prevalence of radiographic findings and correlation with response to therapy. AJR Am J Roentgenol 147:557–561
Cone RO 3rd, Resnick D, Danzig L (1984) Shoulder impingement syndrome: radiographic evaluation. Radiology 150:29–33
Peh WC, Farmer TH, Totty WG (1995) Acromial arch shape: assessment with MR imaging. Radiology 195:501–505
Huang LF, Rubin DA, Britton CA (1999) Greater tuberosity changes as revealed by radiography: lack of clinical usefulness in patients with rotator cuff disease. AJR Am J Roentgenol 172:1381–1388
Liotard JP, Cochard P, Walch G (1998) Critical analysis of the supraspinatus outlet view: rationale for a standard scapular Y-view. J Shoulder Elbow Surg 7:134–139
Hyvonen P, Paivansalo M, Lehtiniemi H, Leppilahti J, Jalovaara P (2001) Supraspinatus outlet view in the diagnosis of stages II and III impingement syndrome. Acta Radiol 42:441–446
Hussain A, Muzzammil M, Butt F, Valsamis EM, Dwyer AJ (2018) Effectiveness of plain shoulder radiograph in detecting degenerate rotator cuff tears. J Ayub Med Coll Abbottabad 30:8–11
Chin K, Chowdhury A, Leivadiotou D, Marmery H, Ahrens PM (2017) The accuracy of plain radiographs in diagnosing degenerate rotator cuff disease. Shoulder Elbow. https://doi.org/10.1177/1758573217743942
Simel DL, Samsa GP, Matchar DB (1991) Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol 44:763–770
Jaeschke R, Guyatt GH, Sackett DL (1994) Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA 271:703–707
Narasimhan R, Shamse K, Nash C, Dhingra D, Kennedy S (2016) Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop 40:975–979
Jacobson JA (2011) Shoulder US: anatomy, technique, and scanning pitfalls. Radiology 260:6–16
Okoroha KR, Mehran N, Duncan J et al (2017) Characterization of rotator cuff tears: ultrasound versus magnetic resonance imaging. Orthopedics 40:e124–e130
Ide J, Maeda S, Takagi K (2005) Arthroscopic transtendon repair of partial-thickness articular-side tears of the rotator cuff: anatomical and clinical study. Am J Sports Med 33:1672–1679
Moosmayer S, Lund G, Seljom US et al (2019) At a 10-year follow-up, tendon repair is superior to physiotherapy in the treatment of small and medium-sized rotator cuff tears. J Bone Joint Surg Am 101:1050–1060
McCallister WV, Parsons IM, Titelman RM, Matsen FA 3rd (2005) Open rotator cuff repair without acromioplasty. J Bone Joint Surg Am 87:1278–1283
Harryman DT 2nd, Mack LA, Wang KY, Jackins SE, Richardson ML, Matsen FA 3rd (1991) Repairs of the rotator cuff. Correlation of functional results with integrity of the cuff. J Bone Joint Surg Am 73:982–989
Yamamoto A, Takagishi K, Osawa T et al (2010) Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 19:116–120
Sayampanathan AA, Andrew TH (2017) Systematic review on risk factors of rotator cuff tears. J Orthop Surg (Hong Kong) 25:2309499016684318
Koh KH, Han KY, Yoon YC, Lee SW, Yoo JC (2013) True anteroposterior (Grashey) view as a screening radiograph for further imaging study in rotator cuff tear. J Shoulder Elbow Surg 22:901–907
Ono K, Yamamuro T, Rockwood CA Jr (1992) Use of a thirty-degree caudal tilt radiograph in the shoulder impingement syndrome. J Shoulder Elbow Surg 1:246–252
Mayerhoefer ME, Breitenseher MJ, Roposch A, Treitl C, Wurnig C (2005) Comparison of MRI and conventional radiography for assessment of acromial shape. AJR Am J Roentgenol 184:671–675
Bigliani LU, Ticker JB, Flatow EL, Soslowsky LJ, Mow VC (1991) The relationship of acromial architecture to rotator cuff disease. Clin Sports Med 10:823–838
Hu J, Shen L, Albanie S, Sun G, Wu E (2018) Squeeze-and-excitation networks. Proceedings of the IEEE conference on computer vision and pattern recognition, pp 7132-7141
Glorot X, Bengio Y (2010) Understanding the difficulty of training deep feedforward neural networks. Proceedings of the thirteenth international conference on artificial intelligence and statistics, pp 249-256
Hinton G, Srivastava N, Swersky K (2012) Neural networks for machine learning lecture 6a overview of mini-batch gradient descent. Available via https://www.cs.toronto.edu/~hinton/coursera/lecture6/lec6.pdf
Simonyan K, Vedaldi A, Zisserman A (2014) Deep inside convolutional networks: visualising image classification models and saliency maps. Available via https://arxiv.org/pdf/1312.6034.pdf. Accessed May 30 2019
Philbrick KA, Yoshida K, Inoue D et al (2018) What does deep learning see? Insights from a classifier trained to predict contrast enhancement phase from CT images. AJR Am J Roentgenol 211:1184–1193
Yao L, Prosky J, Poblenz E, Covington B, Lyman K (2018) Weakly supervised medical diagnosis and localization from multiple resolutions. arXiv preprint arXiv:180307703
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Clopper CJ, Pearson ES (1934) The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 26:404–413
Boonstra AM, Schiphorst Preuper HR, Balk GA, Stewart RE (2014) Cut-off points for mild, moderate, and severe pain on the visual analogue scale for pain in patients with chronic musculoskeletal pain. Pain 155:2545–2550
Bachmann LM, Kolb E, Koller MT, Steurer J, ter Riet G (2003) Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ 326:417
Foad A, Wijdicks CA (2012) The accuracy of magnetic resonance imaging and magnetic resonance arthrogram versus arthroscopy in the diagnosis of subscapularis tendon injury. Arthroscopy 28:636–641
Garavaglia G, Ufenast H, Taverna E (2011) The frequency of subscapularis tears in arthroscopic rotator cuff repairs: a retrospective study comparing magnetic resonance imaging and arthroscopic findings. Int J Shoulder Surg 5:90–94
Ono Y, Sakai T, Carroll MJ, Lo IK (2017) Tears of the subscapularis tendon: a critical analysis review. JBJS Rev 5:1–12
Whiting P, Rutjes AW, Reitsma JB, Glas AS, Bossuyt PM, Kleijnen J (2004) Sources of variation and bias in studies of diagnostic accuracy: a systematic review. Ann Intern Med 140:189–202
Lenza M, Buchbinder R, Takwoingi Y, Johnston RV, Hanchard NC, Faloppa F (2013) Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009020.pub2:CD009020
Acknowledgments
The authors sincerely thank Jeongmin Choi for her contribution in the data collection.
Funding
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2019R1F1A1060126), National Research Foundation of Korea (NRF) grant funded by the Ministry of Education (No. 2017R1D1A1B03033610), and grant from the SNUBH Research Fund (No. 13-2019-006).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yusuhn Kang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors (Dongjun Choi) has significant statistical expertise.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained.
Methodology
• retrospective
• experimental
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 196 kb)
Rights and permissions
About this article
Cite this article
Kim, Y., Choi, D., Lee, K.J. et al. Ruling out rotator cuff tear in shoulder radiograph series using deep learning: redefining the role of conventional radiograph. Eur Radiol 30, 2843–2852 (2020). https://doi.org/10.1007/s00330-019-06639-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06639-1