Abstract
Objectives
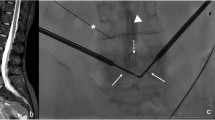
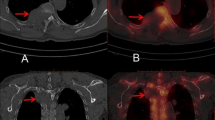
To evaluate post-ablation MRI for the detection of incompletely treated spinal osseous metastases (SOM) after cryoablation and to propose a post-ablation imaging classification.
Methods
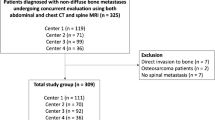
After IRB consent, all patients treated with cryoablation of SOM between 2011 and 2017 having at least 1-year minimum follow-up and a spine MRI within 4 months after cryoablation were retrospectively included. A classification of MRI images into four types was set up. The primary endpoint of our study was to assess the diagnostic performance of the post-ablation MRI. The secondary endpoints were the 1-year complete treatment rate (CTR) and complications.
Results
Fifty-four SOMs in 39 patients were evaluated. Post-ablation MRI was performed with a median delay of 25 days after cryoablation. Images were evaluated by two independent readers according to the pre-established image classification. Sensitivity and specificity for the detection of residual tumor were 77.3% (95%CI = 62.2–88.5) and 85.9% (95%CI = 75.0–93.4), respectively. Types I, II, III, and IV of the classification were associated with a 1-year complete treatment in 100%, 83.3%, 35.7%, and 10% of cases, respectively. The 1-year CTR was 59.3% for all 54 metastases, and 95.8% for metastases measuring less than 25 mm and at least 2 mm or more away from the spinal canal. Two grade 3 and two grade 2 adverse events according to the CTCAE were reported.
Conclusions
MRI after cryoablation is useful for the evaluation of the ablation efficacy. The classification of post-cryoablation MRI provides reliable clues for the prediction of complete treatment at 1 year.
Key Points
• MRI performed 25 days after cryoablation is useful to evaluate the efficacy.
• The proposed classification provides a reliable clue for complete cryoablation.
• Percutaneous cryoablation of spinal metastases is highly effective for lesions less than 25 mm in diameter and of at least 2 mm away from the spinal canal.





Similar content being viewed by others
Abbreviations
- CTR:
-
Complete treatment rate
- PMMA:
-
Polymethylmethacrylate
- SOM:
-
Spinal osseous metastases
- SBRT:
-
Stereotactic body radiotherapy
References
Coleman RE (2006) Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 12:6243s–6249s
Fornasier VL, Horne JG (1975) Metastases to the vertebral column. Cancer 36:590–594
Deschamps F, Farouil G, de Baere T (2014) Percutaneous ablation of bone tumors. Diagn Interv Imaging 95:659–663
Munk PL, Murphy KJ, Gangi A, Liu DM (2011) Fire and ice: percutaneous ablative therapies and cement injection in management of metastatic disease of the spine. Semin Musculoskelet Radiol 15:125–134
Deschamps F, Farouil G, Ternes N et al (2014) Thermal ablation techniques: a curative treatment of bone metastases in selected patients? Eur Radiol 24:1971–1980
Gravel G, Leboulleux S, Tselikas L et al (2018) Prevention of serious skeletal-related events by interventional radiology techniques in patients with malignant paraganglioma and pheochromocytoma. Endocrine 59:547–554
Yang H-L, Liu T, Wang X-M et al (2011) Diagnosis of bone metastases: a meta-analysis comparing 18FDG PET, CT, MRI and bone scintigraphy. Eur Radiol 21:2604–2617
Vanel D, Bittoun J, Tardivon A (1998) MRI of bone metastases. Eur Radiol 8:1345–1351
Lecouvet FE, Larbi A, Pasoglou V et al (2013) MRI for response assessment in metastatic bone disease. Eur Radiol 23:1986–1997
National Cancer Institute (2018) Common Terminology Criteria for Adverse Events (CTCAE). Available via https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm. Accessed 20 Sep 2018
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458
Cohen J (1968) Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 70:213–220
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Buhmann Kirchhoff S, Becker C, Duerr HR et al (2009) Detection of osseous metastases of the spine: comparison of high resolution multi-detector-CT with MRI. Eur J Radiol 69:567–573
Thibault I, Chang EL, Sheehan J et al (2015) Response assessment after stereotactic body radiotherapy for spinal metastasis: a report from the SPIne response assessment in Neuro-Oncology (SPINO) group. Lancet Oncol 16:e595–e603
Constantinidou A, Martin A, Sharma B, Johnston SRD (2011) Positron emission tomography/computed tomography in the management of recurrent/metastatic breast cancer: a large retrospective study from the Royal Marsden Hospital. Ann Oncol 22:307–314
De Giorgi U, Mego M, Rohren EM et al (2010) 18F-FDG PET/CT findings and circulating tumor cell counts in the monitoring of systemic therapies for bone metastases from breast cancer. J Nucl Med 51:1213–1218
Deandreis D, Leboulleux S, Dromain C et al (2011) Role of FDG PET/CT and chest CT in the follow-up of lung lesions treated with radiofrequency ablation. Radiology 258:270–276
Tomasian A, Wallace A, Northrup B et al (2016) Spine cryoablation: pain palliation and local tumor control for vertebral metastases. AJNR Am J Neuroradiol 37:189–195
de Baere T, Elias D, Dromain C et al (2000) Radiofrequency ablation of 100 hepatic metastases with a mean follow-up of more than 1 year. AJR Am J Roentgenol 175:1619–1625
de Baère T, Aupérin A, Deschamps F et al (2015) Radiofrequency ablation is a valid treatment option for lung metastases: experience in 566 patients with 1037 metastases. Ann Oncol 26:987–991
Vidoni A, Grainger M, James S (2018) Experience of neuroprotective air injection during radiofrequency ablation (RFA) of spinal osteoid osteoma. Eur Radiol 10:4146–415023
Wang XS, Rhines LD, Shiu AS et al (2012) Stereotactic body radiation therapy for management of spinal metastases in patients without spinal cord compression: a phase 1-2 trial. Lancet Oncol 13:395–402
Yamada Y, Bilsky MH, Lovelock DM et al (2008) High-dose, single-fraction image-guided intensity-modulated radiotherapy for metastatic spinal lesions. Int J Radiat Oncol Biol Phys 71:484–490
Boehling NS, Grosshans DR, Allen PK et al (2012) Vertebral compression fracture risk after stereotactic body radiotherapy for spinal metastases. J Neurosurg Spine 16:379–386
Rose PS, Laufer I, Boland PJ et al (2009) Risk of fracture after single fraction image-guided intensity-modulated radiation therapy to spinal metastases. J Clin Oncol 27:5075–5079
Myrehaug S, Sahgal A, Hayashi M et al (2017) Reirradiation spine stereotactic body radiation therapy for spinal metastases: systematic review. J Neurosurg Spine 27:428–435
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Frederic Deschamps.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gravel, G., Tselikas, L., Moulin, B. et al. Early detection with MRI of incomplete treatment of spine metastases after percutaneous cryoablation. Eur Radiol 29, 5655–5663 (2019). https://doi.org/10.1007/s00330-019-06040-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06040-y