Abstract
Objectives
To determine whether extracellular volume fraction (ECV) quantification by cardiac magnetic resonance (CMR) can demonstrate left ventricle (LV) abnormalities and relationship between ECV and LV remodeling in hypertension (HTN) patients
Methods
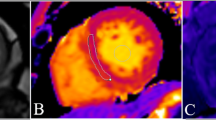
ECV quantification was prospectively performed in 134 consecutive HTN patients and 97 healthy subjects. Individual and regional ECV were compared to the regions on late gadolinium enhancement (LGE) images. Statistical analysis of the relationship between LV global functional parameters and ECV was carried out using Pearson’s correlation, Student’s t test and multiple regressions.
Results
In the HTN group, 70.1% (94/134) were LGE negative and 29.9% (40/134) LGE positive. The mean ECV after adjusting for age, sex, BMI, diabetes, smoking and dyslipidaemia in healthy controls and LGE-negative patients were 26.9 ± 2.67% and 28.5 ± 2.9% (p < 0.001), respectively. The differences in ECV reached statistical significance among the regions of LGE, LGE-Peri, LGE remote and the normal area between the control and LGE-positive subgroup (all p < 0.05). Global ECV significantly correlated with LVEF (r = −0.466, p < 0 .001) and LV hypertrophy (r = 0.667, p < 0.001).
Conclusions
ECV can identify LV abnormalities at an early stage in HTN patients without LGE. These abnormalities may reflect an increase in diffuse myocardial fibrosis and are associated with LV remodeling.
Key points
• Diffuse myocardial fibrosis may develop in hypertensive cardiomyopathy before conventional MRI detectable LGE.
• ECV can identify myocardial fibrosis at an early stage in hypertensive patients.
• Elevated ECV is associated with decreased LV global function and LV remodeling in hypertension.








Similar content being viewed by others
Abbreviations
- BP:
-
Blood pressure
- CI:
-
Cardiac index
- CMR:
-
Cardiac magnetic resonance
- ECV:
-
Extracellular volume fraction
- HTN:
-
Hypertension
- LA:
-
Left atrium
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle
- LVEDVi:
-
Left ventricular end-diastolic volume index
- LVEF:
-
Left ventricular ejection fraction
- LVESVi:
-
Left ventricular end-systolic volume index
- LVH:
-
Left ventricular hypertrophy
- MaxDBP:
-
Maximum diastolic blood pressure
- MaxSBP:
-
Maximum systolic blood pressure
- PSIR:
-
Phase sensitive inversion recovery
- ROI:
-
Region of interest
- SV:
-
Stroke volume
References
Chobanian AV, Bakris GL, Black HR et al (2003) Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42:1206–1252
Drazner MH (2011) The progression of hypertensive heart disease. Circulation 123:327–334
Diez J, Gonzalez A, Lopez B, Querejeta R (2005) Mechanisms of disease: pathologic structural remodeling is more than adaptive hypertrophy in hypertensive heart disease. Nat Clin Pract Cardiovasc Med 2:209–216
Rossi MA (1998) Pathologic fibrosis and connective tissue matrix in left ventricular hypertrophy due to chronic arterial hypertension in humans. J Hypertens 16:1031–1041
Ciulla M, Paliotti R, Hess DB et al (1997) Echocardiographic patterns of myocardial fibrosis in hypertensive patients: endomyocardial biopsy versus ultrasonic tissue characterization. J Am Soc Echocardiogr: Off Publ Am Soc Echocardiogr 10:657–664
Aurigemma GP, Silver KH, Priest MA, Gaasch WH (1995) Geometric changes allow normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. J Am Coll Cardiol 26:195–202
Guerin AP, Adda H, London GM, Marchais SJ (2004) Cardiovascular disease in renal failure. Minerva Irol Nefrol Ital J Urol Nephrol 56:279–288
Kali A, Cokic I, Tang RL et al (2014) Determination of location, size, and transmurality of chronic myocardial infarction without exogenous contrast media by using cardiac magnetic resonance imaging at 3 T. Circ Cardiovasc Imaging 7:471–481
Deux JF, Rahmouni A, Garot J (2008) Cardiac magnetic resonance and 64-slice cardiac CT of lipomatous metaplasia of chronic myocardial infarction. Eur Heart J 29:570
Bravo PE, Zimmerman SL, Luo HC et al (2013) Relationship of delayed enhancement by magnetic resonance to myocardial perfusion by positron emission tomography in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging 6:210–217
Esposito A, De Cobelli F, Perseghin G et al (2009) Impaired left ventricular energy metabolism in patients with hypertrophic cardiomyopathy is related to the extension of fibrosis at delayed gadolinium-enhanced magnetic resonance imaging. Heart 95:228–233
Flett AS, Hasleton J, Cook C et al (2011) Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance. J Am Coll Cardiol Img 4:150–156
Kuruvilla S, Janardhanan R, Antkowiak P et al (2015) Increased extracellular volume and altered mechanics are associated with LVH in hypertensive heart disease, not hypertension alone. J Am Coll Cardiol Img 8:172–180
Treibel TA, Zemrak F, Sado DM et al (2015) Extracellular volume quantification in isolated hypertension - changes at the detectable limits? J Cardiovasc Magn Reson: Off J Soc Cardiovasc Magn Reson 17:74
Forman JP, Scheven L, de Jong PE, Bakker SJ, Curhan GC, Gansevoort RT (2012) Association between sodium intake and change in uric acid, urine albumin excretion, and the risk of developing hypertension. Circulation 125:3108–3116
Burns J, Sivananthan MU, Ball SG, Mackintosh AF, Mary DA, Greenwood JP (2007) Relationship between central sympathetic drive and magnetic resonance imaging-determined left ventricular mass in essential hypertension. Circulation 115:1999–2005
Kellman P, Arai AE, McVeigh ER, Aletras AH (2002) Phase-sensitive inversion recovery for detecting myocardial infarction using gadolinium-delayed hyperenhancement. Magn Reson Med 47:372–383
Messroghli DR, Radjenovic A, Kozerke S, Higgins DM, Sivananthan MU, Ridgway JP (2004) Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med 52:141–146
Kellman P, Wilson JR, Xue H et al (2012) Extracellular volume fraction mapping in the myocardium, part 2: initial clinical experience. J Cardiovasc Magn Reson: Off J Soc Cardiovasc Magn Reson 14:64
Kellman P, Hansen MS (2014) T1-mapping in the heart: accuracy and precision. J Cardiovasc Magn Reson: Off J Soc Cardiovasc Magn Reson 16:2
Lu M, Zhao S, Yin G et al (2013) T1 mapping for detection of left ventricular myocardial fibrosis in hypertrophic cardiomyopathy: a preliminary study. Eur J Radiol 82:e225–e231
Lu M, Zhao S, Jiang S et al (2013) Fat deposition in dilated cardiomyopathy assessed by CMR. J Am Coll Cardiol Img 6:889–898
Schelbert EB, Testa SM, Meier CG et al (2011) Myocardial extravascular extracellular volume fraction measurement by gadolinium cardiovascular magnetic resonance in humans: slow infusion versus bolus. J Cardiovasc Magn Reson: Off J Soc Cardiovasc Magn Reson 13:16
Ugander M, Oki AJ, Hsu LY et al (2012) Extracellular volume imaging by magnetic resonance imaging provides insights into overt and sub-clinical myocardial pathology. Eur Heart J 33:1268–1278
Moon JC, Messroghli DR, Kellman P et al (2013) Myocardial T1 mapping and extracellular volume quantification: a Society for Cardiovascular Magnetic Resonance (SCMR) and CMR Working Group of the European Society of Cardiology consensus statement. J Cardiovasc Magn Reson: Off J Soc Cardiovasc Magn Reson 15:92
Kellman P, Wilson JR, Xue H, Ugander M, Arai AE (2012) Extracellular volume fraction mapping in the myocardium, part 1: evaluation of an automated method. J Cardiovasc Magn Reson: Off J Soc Cardiovasc Magn Reson 14:63
White SK, Sado DM, Fontana M et al (2013) T1 mapping for myocardial extracellular volume measurement by CMR: bolus only versus primed infusion technique. J Am Coll Cardiol Img 6:955–962
Liu CY, Liu YC, Wu C et al (2013) Evaluation of age-related interstitial myocardial fibrosis with cardiac magnetic resonance contrast-enhanced T1 mapping: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 62:1280–1287
Bandula S, Banypersad SM, Sado D et al (2013) Measurement of Tissue interstitial volume in healthy patients and those with amyloidosis with equilibrium contrast-enhanced MR imaging. Radiology 268:858–864
Wong TC, Piehler K, Meier CG et al (2012) Association between extracellular matrix expansion quantified by cardiovascular magnetic resonance and short-term mortality. Circulation 126:1206–1216
Kis A, Murdoch C, Zhang M et al (2009) Defective peroxisomal proliferators activated receptor gamma activity due to dominant-negative mutation synergizes with hypertension to accelerate cardiac fibrosis in mice. Eur J Heart Fail 11:533–541
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Minjie Lu and Shihua Zhao.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Funding
This study was supported in parts by the Research Grant of National Natural Science Foundation of China (81571647, 81370036 and 81620108015), Capital Clinically Characteristic Applied Research Fund (Z151100004015141), Beijing Natural Science Foundation (7152124) and the Fundamental Research Funds for the Central Universities (3332013105). This work was also partially supported by the Division of Intramural Research, National Heart, Lung and Blood Institute, National Institutes of Health, USA.
Statistics and biometry
One of the authors has significant statistical expertise.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Methodology
• prospective
• cross-sectional study
• performed at one institution
Rights and permissions
About this article
Cite this article
Wang, S., Hu, H., Lu, M. et al. Myocardial extracellular volume fraction quantified by cardiovascular magnetic resonance is increased in hypertension and associated with left ventricular remodeling. Eur Radiol 27, 4620–4630 (2017). https://doi.org/10.1007/s00330-017-4841-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4841-9