Abstract
Objectives
To evaluate a novel, ready-to-use, iodinated polyvinyl alcohol polymer embolic implant.
Methods
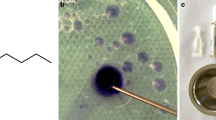
Under good laboratory practice conditions, 26 pigs were investigated. A complex arteriovenous malformation (AVM) model was created in 16 animals, and a simple rete model was used in the remaining 10 animals. The novel material was used for embolization in 22 animals, and a commercially available liquid embolic material in 4 animals as a control group. Animals were killed at 2 days, 3 months and 6 months. Feasibility, efficacy and safety were evaluated radiologically, clinically and histologically.
Results
Preparation was easy, without risk of catheter clogging or adhesiveness. Embolic delivery was well controlled under subtracted fluoroscopy. Visibility was homogeneous throughout the injection and the material behaved cohesively upon delivery. Best lesion penetration was obtained with the use of proximal microballoon occlusion. Unforeseen over-dilution of the test material by DMSO prefilled in the microballoon hub changed the material properties and caused inadvertent cerebral embolization leading to death in five animals. This phenomenon was avoided by practical measures. The casts produced no beam-hardening artefacts on CT scans. Histology showed excellent biocompatibility.
Conclusions
Embolization with this novel, iodinated, precipitating polymer was feasible and effective. Care should be taken during delivery to avoid over-dilution of the material by prefilled DMSO. The material is promising for embolization of AVMs and hypervascular lesions.
Key Points
• The intrinsically opaque precipitating polymer has adequate fluoroscopic visibility
• The polymer does not induce shading or beam-hardening artefacts on CT
• The novel liquid embolic material does not require lengthy preparation
• Lack of implant adherence reduces the risk of entrapment of the delivery catheter





Similar content being viewed by others
Abbreviations
- AVM:
-
Arteriovenous malformation
- CCA:
-
Ccommon carotid artery
- DMSO:
-
Dimethyl sulfoxide
- EVOH:
-
Ethylene vinyl alcohol copolymer
References
Jahan R, Murayama Y, Gobin YP, Duckwiler GR, Vinters HV, Viñuela F (2001) Embolization of arteriovenous malformations with Onyx: clinicopathological experience in 23 patients. Neurosurgery 48:984–997
Kerber C (1976) Balloon catheter with a calibrated leak. A new system for superselective angiography and occlusive catheter therapy. Radiology 120:547–550
Molyneux AJ, Cekirge S, Saatci I, Gál G (2004) Cerebral Aneurysm Multicenter European Onyx (CAMEO) trial: results of a prospective observational study in 20 European centers. AJNR Am J Neuroradiol 25:39–51
Pierot L, Cognard C, Herbreteau D et al (2013) Endovascular treatment of brain arteriovenous malformations using a liquid embolic agent: results of a prospective, multicentre study (BRAVO). Eur Radiol 23:2838–2845
Wanke I, Jäckel MC, Goericke S, Panagiotopoulos V, Dietrich U, Forsting M (2009) Percutaneous embolization of carotid paragangliomas using solely Onyx. AJNR Am J Neuroradiol 30:1594–1597
Zelenák K, Sopilko I, Svihra J, Kliment J (2009) Successful embolization of a renal artery pseudoaneurysm with arteriovenous fistula and extravasations using Onyx after partial nephrectomy for renal cell carcinoma. Cardiovasc Intervent Radiol 32:163–165
Lenhart M, Paetzel C, Sackmann M et al (2010) Superselective arterial embolisation with a liquid polyvinyl alcohol copolymer in patients with acute gastrointestinal haemorrhage. Eur Radiol 20:1994–1999
Vanninen RL, Manninen I (2007) Onyx, a new liquid embolic material for peripheral interventions: preliminary experience in aneurysm, pseudoaneurysm, and pulmonary arteriovenous malformation embolization. Cardiovasc Intervent Radiol 30:196–200
Jordan O, Doelker E, Rüfenacht DA (2005) Biomaterials used in injectable implants (liquid embolics) for percutaneous filling of vascular spaces. Cardiovasc Intervent Radiol 28:561–569
Taki W, Yonekawa Y, Iwata H, Uno A, Yamashita K, Amemiya H (1990) A new liquid material for embolization of arteriovenous malformations. AJNR Am J Neuroradiol 11:163–168
Chaloupka JC, Vi F, Vinters HV, Robert J (1994) Technical feasibility and histopathologic studies of ethylene vinyl copolymer (EVAL) using a swine endovascular embolization model. AJNR Am J Neuroradiol 15:1107–1115
Taki W, Nishi S, Yamashita K et al (1992) Selection and combination of various endovascular techniques in the treatment of giant aneurysms. J Neurosurg 77:37–42
Schirmer CM, Zerris V, Malek AM (2006) Electrocautery-induced ignition of spark showers and self-sustained combustion of onyx ethylene-vinyl alcohol copolymer. Neurosurgery 59:ONS413–ONS418
Weber W, Kis B, Siekmann R, Kuehne D (2007) Endovascular treatment of intracranial arteriovenous malformations with onyx: technical aspects. AJNR Am J Neuroradiol 28:371–377
Szajner M, Roman T, Markowicz J, Szczerbo-Trojanowska M (2013) Onyx(®) in endovascular treatment of cerebral arteriovenous malformations – a review. Pol J Radiol 78:35–41
Dudeck O, Jordan O, Hoffmann K-T et al (2006) Intrinsically radiopaque iodine-containing polyvinyl alcohol as a liquid embolic agent: evaluation in experimental wide-necked aneurysms. J Neurosurg 104:290–297
Dudeck O, Jordan O, Hoffmann KT et al (2006) Embolization of experimental wide-necked aneurysms with iodine-containing polyvinyl alcohol solubilized in a low-angiotoxicity solvent. AJNR Am J Neuroradiol 27:1849–1855
Massoud TF, Ji C, Vi F et al (1994) An experimental arteriovenous malformation model in swine: anatomic basis and construction technique. AJNR Am J Neuroradiol 15:1537–1545
Link DP, Strandberg JD, Virmani R, Blashka K, Mourtada F, Samphilipo MA (1996) Histopathologic appearance of arterial occlusions with hydrogel and polyvinyl alcohol embolic material in domestic swine. J Vasc Interv Radiol 7:897–905
Bilbao JI, de Luis E, García de Jalón JA et al (2008) Comparative study of four different spherical embolic particles in an animal model: a morphologic and histologic evaluation. J Vasc Interv Radiol 19:1625–1638
Panagiotopoulos V, Gizewski E, Asgari S, Regel J, Forsting M, Wanke I (2009) Embolization of intracranial arteriovenous malformations with ethylene-vinyl alcohol copolymer (Onyx). AJNR Am J Neuroradiol 30:99–106
Spiotta AM, James RF, Lowe SR et al (2015) Balloon-augmented Onyx embolization of cerebral arteriovenous malformations using a dual-lumen balloon: a multicenter experience. J Neurointerv Surg 7:721–727
Chapot R, Stracke P, Velasco A et al (2014) The pressure cooker technique for the treatment of brain AVMs. J Neuroradiol 41:87–91
Acknowledgements
We thank Nikola Cesarovic, DVM, and Flora Nicholls-Vuille, DVM, Division of Surgical Research, University Hospital of Zurich, Zurich, Switzerland, for their valuable contribution to the surgical procedures in the animals.
The scientific guarantor of this publication is I.W. O.J. is a shareholder of Antia Therapeutics AG. This study received funding from Antia Therapeutics AG. One of the authors (K.K.) has significant statistical expertise. Approval from the institutional animal care committee was obtained.
Methodology: Prospective/experimental study performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 38 kb)
Rights and permissions
About this article
Cite this article
Kulcsár, Z., Karol, A., Kronen, P.W. et al. A novel, non-adhesive, precipitating liquid embolic implant with intrinsic radiopacity: feasibility and safety animal study. Eur Radiol 27, 1248–1256 (2017). https://doi.org/10.1007/s00330-016-4463-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4463-7