Abstract
Objectives
Investigating the association between baseline cartilage volume measurements (and initial 24th month volume loss) with medial compartment Joint-Space-Loss (JSL) progression (>0.7 mm) during 24–48th months of study.
Methods
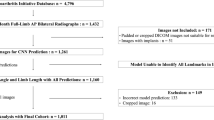
Case and control cohorts (Biomarkers Consortium subset from the Osteoarthritis Initiative (OAI)) were defined as participants with (n=297) and without (n=303) medial JSL progression (during 24–48th months). Cartilage volume measurements (baseline and 24th month loss) were obtained at five knee plates (medial-tibial, lateral-tibial, medial-femoral, lateral-femoral and patellar), and standardized values were analysed. Multivariate logistic regression was used with adjustment for known confounders. Artificial-Neural-Network analysis was conducted by Multi-Layer-Perceptrons (MLPs) including baseline determinants, and baseline (1) and interval changes (2) in cartilage volumes.
Results
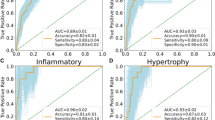
Larger baseline lateral-femoral cartilage volume was predictive of medial JSL (OR: 1.29 (1.01–1.64)). Greater initial 24th month lateral-femoral cartilage volume-loss (OR: 0.48 (0.27–0.84)) had protective effect on medial JSL during 24–48th months of study. Baseline and interval changes in lateral-femoral cartilage volume, were the most important estimators for medial JSL progression (importance values: 0.191(0.177–0.204), 0.218(0.207–0.228)) in the ANN analyses.
Conclusions
Cartilage volumes (both at baseline and their change during the initial 24 months) in the lateral femoral plate were predictive of medial JSL progression.
Key Points
• Baseline lateral femoral cartilage volume is directly associated with medial JSL progression.
• 24-month lateral femoral cartilage loss is inversely associated with medial JSL progression.
• Lateral femoral cartilage volume is most important in association with medial JSL progression.




Similar content being viewed by others
Abbreviations
- ANN:
-
Artificial-Neural-Network
- JSL:
-
Joint Space Loss
- KL:
-
grade radiographic Kellgren and Lawrence (KL) grade
- MLP:
-
Multi-Layer-Perceptron
- OA:
-
Osteoarthritis
- OAI:
-
Osteoarthritis Initiative
- WOMAC:
-
grade Western-Ontario-and-McMaster score
References
Demehri S, Hafezi-Nejad N, Carrino JA (2015) Conventional and novel imaging modalities in osteoarthritis: current state of the evidence. Curr Opin Rheumatol 27:295–303
Roemer FW, Guermazi A (2014) Osteoarthritis year in review 2014: imaging. Osteoarthr Cartil 22:2003–2012
Pelletier JP, Cooper C, Peterfy C et al (2013) What is the predictive value of MRI for the occurrence of knee replacement surgery in knee osteoarthritis? Ann Rheum Dis 72:1594–1604
Roemer FW, Kwoh CK, Hannon MJ et al (2015) What comes first? Multi-tissue involvement leading to radiographic osteoarthritis: MRI-based trajectory analysis over 4 years in the Osteoarthritis Initiative. Arthritis Rheumatol. doi:10.1002/art.39176
Eckstein F, Boudreau RM, Wang Z et al (2014) Trajectory of cartilage loss within 4 years of knee replacement--a nested case–control study from the Osteoarthritis Initiative. Osteoarthr Cartil 22:1542–1549
Roemer FW, Zhang Y, Niu J et al (2009) Tibiofemoral joint osteoarthritis: risk factors for MR-depicted fast cartilage loss over a 30-month period in the multicenter osteoarthritis study. Radiology 252:772–780
Wildi LM, Martel-Pelletier J, Abram F, Moser T, Raynauld JP, Pelletier JP (2013) Assessment of cartilage changes over time in knee osteoarthritis disease-modifying osteoarthritis drug trials using semiquantitative and quantitative methods: pros and cons. Arthritis Care Res (Hoboken) 65:686–694
Roemer FW, Guermazi A, Felson DT et al (2011) Presence of MRI-detected joint effusion and synovitis increases the risk of cartilage loss in knees without osteoarthritis at 30-month follow-up: the MOST study. Ann Rheum Dis 70:1804–1809
Roemer FW, Kwoh CK, Hannon MJ et al (2012) Risk factors for magnetic resonance imaging-detected patellofemoral and tibiofemoral cartilage loss during a six-month period: the joints on glucosamine study. Arthritis Rheum 64:1888–1898
Roemer FW, Kwoh CK, Hannon MJ et al (2015) Can structural joint damage measured with MR imaging be used to predict knee replacement in the following year? Radiology 274:810–820
Atukorala I, Kwoh CK, Guermazi A et al (2014) Synovitis in knee osteoarthritis: a precursor of disease? Ann Rheum Dis. doi:10.1136/annrheumdis-2014-205894
Guermazi A, Hayashi D, Roemer F et al (2015) Severe radiographic knee osteoarthritis - does Kellgren and Lawrence grade 4 represent end stage disease? - the MOST study. Osteoarthr Cartil. doi:10.1016/j.joca.2015.04.018
Sharma L, Chmiel JS, Almagor O et al (2014) Significance of preradiographic magnetic resonance imaging lesions in persons at increased risk of knee osteoarthritis. Arthritis Rheumatol 66:1811–1819
Reichenbach S, Yang M, Eckstein F et al (2010) Does cartilage volume or thickness distinguish knees with and without mild radiographic osteoarthritis? The Framingham Study. Ann Rheum Dis 69:143–149
Jones G, Ding C, Scott F, Glisson M, Cicuttini F (2004) Early radiographic osteoarthritis is associated with substantial changes in cartilage volume and tibial bone surface area in both males and females. Osteoarthr Cartil 12:169–174
Cicuttini FM, Wluka AE, Forbes A, Wolfe R (2003) Comparison of tibial cartilage volume and radiologic grade of the tibiofemoral joint. Arthritis Rheum 48:682–688
Teichtahl AJ, Wluka AE, Wang Y et al (2014) The longitudinal relationship between changes in body weight and changes in medial tibial cartilage, and pain among community-based adults with and without meniscal tears. Ann Rheum Dis 73:1652–1658
Antony B, Ding C, Stannus O, Cicuttini F, Jones G (2011) Association of baseline knee bone size, cartilage volume, and body mass index with knee cartilage loss over time: a longitudinal study in younger or middle-aged adults. J Rheumatol 38:1973–1980
Ding C, Cicuttini F, Scott F, Glisson M, Jones G (2003) Sex differences in knee cartilage volume in adults: role of body and bone size, age and physical activity. Rheumatology (Oxford) 42:1317–1323
Cicuttini FM, Wluka A, Bailey M et al (2003) Factors affecting knee cartilage volume in healthy men. Rheumatology (Oxford) 42:258–262
Cicuttini FM, Wluka AE, Wang Y, Davis SR, Hankin J, Ebeling P (2002) Compartment differences in knee cartilage volume in healthy adults. J Rheumatol 29:554–556
Arno S, Walker PS, Bell CP et al (2012) Relation between cartilage volume and meniscal contact in medial osteoarthritis of the knee. Knee 19:896–901
Bennell KL, Bowles KA, Wang Y, Cicuttini F, Davies-Tuck M, Hinman RS (2011) Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis 70:1770–1774
Hunter DJ, Niu JB, Zhang Y et al (2008) Premorbid knee osteoarthritis is not characterised by diffuse thinness: the Framingham Osteoarthritis Study. Ann Rheum Dis 67:1545–1549
Hunter DJ, Nevitt M, Losina E, Kraus V (2014) Biomarkers for osteoarthritis: current position and steps towards further validation. Best Pract Res Clin Rheumatol 28:61–71
Eckstein F, Collins J, Nevitt M et al. (2015) Cartilage Thickness Change as an Imaging Biomarker of Knee Osteoarthritis Progression - Data from the FNIH OA Biomarkers Consortium. Arthritis Rheumatol Accepted
Ornetti P, Brandt K, Hellio-Le Graverand MP et al (2009) OARSI-OMERACT definition of relevant radiological progression in hip/knee osteoarthritis. Osteoarthr Cartil 17:856–863
Dam EB, Lillholm M, Marques J, Nielsen M (2015) Automatic segmentation of high-and low-field knee MRIs using knee image quantification with data from the osteoarthritis initiative. J Med Imaging 2:024001–024001
Kerkhof HJ, Bierma-Zeinstra SM, Arden NK et al (2014) Prediction model for knee osteoarthritis incidence, including clinical, genetic and biochemical risk factors. Ann Rheum Dis 73:2116–2121
Zhang W, McWilliams DF, Ingham SL et al (2011) Nottingham knee osteoarthritis risk prediction models. Ann Rheum Dis 70:1599–1604
Hafezi-Nejad N, Guermazi A, Roemer FW, Eng J, Zikria B, Demehri S (2015) Long term Use of Analgesics and Risk of Osteoarthritis Progressions and Knee Replacement: Propensity Score Matched Cohort Analysis of Data from the Osteoarthritis Initiative. Osteoarthr Cartil. doi:10.1016/j.joca.2015.11.003
Hafezi-Nejad N, Zikria B, Eng J, Carrino JA, Demehri S (2015) Predictive value of semi-quantitative MRI-based scoring systems for future knee replacement: data from the osteoarthritis initiative. Skeletal Radiol 44:1655–1662
Lemeshow S, Hosmer DW Jr (1982) A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol 115:92–106
Toney LK, Vesselle HJ (2014) Neural networks for nodal staging of non-small cell lung cancer with FDG PET and CT: importance of combining uptake values and sizes of nodes and primary tumor. Radiology 270:91–98
Forsstrom JJ, Dalton KJ (1995) Artificial neural networks for decision support in clinical medicine. Ann Med 27:509–517
Harada Y, Tokuda O, Fukuda K et al (2011) Relationship between cartilage volume using MRI and Kellgren-Lawrence radiographic score in knee osteoarthritis with and without meniscal tears. AJR Am J Roentgenol 196:W298–304
Jackson BD, Teichtahl AJ, Morris ME, Wluka AE, Davis SR, Cicuttini FM (2004) The effect of the knee adduction moment on tibial cartilage volume and bone size in healthy women. Rheumatology (Oxford) 43:311–314
Teichtahl AJ, Davies-Tuck ML, Wluka AE, Jones G, Cicuttini FM (2009) Change in knee angle influences the rate of medial tibial cartilage volume loss in knee osteoarthritis. Osteoarthr Cartil 17:8–11
Zhai G, Ding C, Cicuttini F, Jones G (2007) A longitudinal study of the association between knee alignment and change in cartilage volume and chondral defects in a largely non-osteoarthritic population. J Rheumatol 34:181–186
Cicuttini F, Wluka A, Hankin J, Wang Y (2004) Longitudinal study of the relationship between knee angle and tibiofemoral cartilage volume in subjects with knee osteoarthritis. Rheumatology (Oxford) 43:321–324
Chapman GJ, Parkes MJ, Forsythe L, Felson DT, Jones RK (2015) Ankle motion influences the external knee adduction moment and may predict who will respond to lateral wedge insoles?: an ancillary analysis from the SILK trial. Osteoarthr Cartil. doi:10.1016/j.joca.2015.02.164
Hunt MA, Takacs J (2014) Effects of a 10-week toe-out gait modification intervention in people with medial knee osteoarthritis: a pilot, feasibility study. Osteoarthr Cartil 22:904–911
Hitzl W, Wirth W, Maschek S et al (2015) Greater Lateral Femorotibial Cartilage Loss in Osteoarthritis Initiative Participants with Incident Knee Replacement: A Prospective Cohort Study. Arthritis Care Res (Hoboken). doi:10.1002/acr.22608
Hanna F, Wluka AE, Ebeling PR, O'Sullivan R, Davis SR, Cicuttini FM (2006) Determinants of change in patella cartilage volume in healthy subjects. J Rheumatol 33:1658–1661
de Lange-Brokaar BJ, Bijsterbosch J, Kornaat PR et al (2015) Radiographic progression of knee osteoarthritis is associated with MRI abnormalities in both the patellofemoral and tibiofemoral joint. Osteoarthr Cartil. doi:10.1016/j.joca.2015.09.021
Preis O, Blake MA, Scott JA (2011) Neural network evaluation of PET scans of the liver: a potentially useful adjunct in clinical interpretation. Radiology 258:714–721
Lee HJ, Hwang SI, Han SM et al (2010) Image-based clinical decision support for transrectal ultrasound in the diagnosis of prostate cancer: comparison of multiple logistic regression, artificial neural network, and support vector machine. Eur Radiol 20:1476–1484
Pizzuto F, Voci P, Bartolomucci F et al (2009) Usefulness of coronary flow reserve measured by echocardiography to improve the identification of significant left anterior descending coronary artery stenosis assessed by multidetector computed tomography. Am J Cardiol 104:657–664
Schwarzer G, Vach W, Schumacher M (2000) On the misuses of artificial neural networks for prognostic and diagnostic classification in oncology. Stat Med 19:541–561
Acknowledgements
The scientific guarantor of this publication is Dr. Shadpour Demehri, Nima Hafezi Nejad.
The authors of this manuscript declare relationships with the following companies: Nima Hafezi-Nejad and Bashir Zikria have no conflicts of interest. Ali Guermazi is the president and shareholder of Boston Imaging Core Lab, LLC. He is consultant to Genzyme, MerckSerono, TissueGene and OrthoTrophix. Frank W Roemer is the CMO and shareholder of Boston Imaging Core Lab, LLC. Shadpour Demehri has grants from GERRAF 2014 – 2016; Carestream Health Inc. 2013 – 2015 for Cone – Beam CT clinical trial. He is a consultant to Toshiba Medical Systems. Erik Dam is shareholder of Biomediq. Biomediq holds the property rights of the KneeIQ framework. David Hunter and Kent Kwoh have no relevant conflicts of interest.
This study has received funding by:
The research leading to these results has received funding from the D-BOARD consortium, a European Union Seventh Framework Programme (FP7/2007-2013) under grant agreement n° 305815. The OAI collection was provided by the Osteoarthritis Initiative with the cartilage and menisci segmentations performed by iMorphics. The OAI is a public-private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation, GlaxoSmithKline; and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Scientific and financial support for the FNIH OA Biomarkers Consortium and the study are made possible through grants, direct and in-kind contributions provided by: AbbVie; Amgen Inc.; Arthritis Foundation; Bioiberica S.A.; DePuy Mitek, Inc.; Flexion Therapeutics, Inc.; GlaxoSmithKline; Merck Serono; Rottapharm | Madaus; Sanofi; Stryker; The Pivotal OAI MRI Analyses (POMA) Study, NIH HHSN2682010000. We thank the Osteoarthritis Research Society International (OARSI) for their leadership and expertise on the FNIH OA Biomarker Consortium project. Private sector funding for the Consortium and OAI is managed by the FNIH. We also gratefully acknowledge financial support from the Danish Research Foundation (“Den Danske Forskningsfond”). The research leading to these results has received funding from the D-BOARD consortium, a European Union Seventh Framework Programme (FP7/2007-2013) under grant agreement n° 305815. The OAI collection was provided by the Osteoarthritis Initiative with the cartilage and menisci segmentations performed by iMorphics.
One of the authors has significant statistical expertise.
Institutional Review Board approval was not required because this study uses the data from the OAI (FNIH Biomarkers Consortium) study which is accessible through the OAI web portal at https://oai.epi-ucsf.org.
Some study subjects or cohorts previously reported in this study use the data from the OAI (FNIH Biomarkers Consortium) study which is accessible through the OAI web portal at https://oai.epi-ucsf.org.
For related reports please see:
Hunter DJ, Nevitt M, Losina E, Kraus V (2014) Biomarkers for osteoarthritis: current position and steps towards further validation. Best practice & research Clinical rheumatology 28:61–1
Also: https://oai.epi-ucsf.org/datarelease/docs/FNIH/OaBioFnihDataOverview.pdf
Methodology: prospective, cohort study, observational, multicentre study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hafezi-Nejad, N., Guermazi, A., Roemer, F.W. et al. Prediction of medial tibiofemoral compartment joint space loss progression using volumetric cartilage measurements: Data from the FNIH OA biomarkers consortium. Eur Radiol 27, 464–473 (2017). https://doi.org/10.1007/s00330-016-4393-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4393-4