Abstract
Objectives
Assessment of perianal fistulas is important to guide management of Crohn's disease (CD). Our objectives were to analyze the feasibility of magnetization transfer (MT) imaging to assess fistulas and to evaluate its contribution in assessing disease activity.
Methods
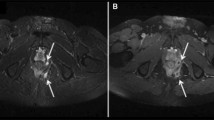
During 15 months, all patients referred for perianal fistulas in CD underwent 3T-MRI including diffusion, T2/T1-weighted gadolinium-enhanced sequences and MT sequences (one with an off-resonance saturation pulse of 800 and one with 1200 Hz). We collected Van Assche score, fistula activity signs by analyzing T2, diffusion and contrast enhancement. We calculated MT ratio (MTR) with a ROI in the largest fistula.
Results
Twenty-nine patients (mean 34.9 years, range 17-53) were included. Van Assche score was 11.7, range 4–21. In 22 patients, the fistula presented with a bright T2 and diffusion signal with contrast enhancement, and was characterized as active. Mean MTR was respectively 47.2 (range 12–68) and 34.3 (range 11–57) at 800 and 1200 Hz. MTR at 800 Hz was significantly lower in non-active (34, range 12–55) than in active fistulas (51, range 24–68) (p < 0.02).
Conclusions
MTR is feasible for the assessment of fistulas in CD and in the future could be used to help identify active and non-active fistulas.
Key Points
• MTR is feasible for the assessment of perianal fistulas in CD.
• MT allows quantitative imaging of perianal fistula activity in CD.
• MTR could be used to help identify active and non-active fistulas in CD.





Similar content being viewed by others
Abbreviations
- CD:
-
Crohn’s disease
- MT:
-
Magnetization transfer
- MTR:
-
Magnetization transfer ratio
References
Schwartz DA, Loftus EV Jr, Tremaine WJ et al (2002) The natural history of fistulizing Crohn’s disease in Olmsted County, Minnesota. Gastroenterology 122:875–880
Ingle SB, Loftus EV Jr (2007) The natural history of perianal Crohn's disease. Dig Liver Dis 39:963–969
Lapidus A (2006) Crohn’s disease in Stockholm County during 1990-2001: an epidemiological update. World J Gastroenterol 12:75–81
Sandborn WJ, Fazio VW, Feagan BG, Hanauer SB, American gastroenterological association clinical practice committee (2003) AGA technical review on perianal Crohn’s disease. Gastroenterology 125:1508–1530
Present DH, Rutgeerts P, Targan S et al (1999) Infliximab for the treatment of fistulas in patients with Crohn's disease. N Engl J Med 340:1398–1405
Irvine EJ (1995) Usual therapy improves perianal Crohn's disease as measured by a new disease activity index. McMaster IBD Study Group. J Clin Gastroenterol 20:27–32
Dejaco C, Harrer M, Waldhoer T, Miehsler W, Vogelsang H, Reinisch W (2003) Antibiotics and azathioprine for the treatment of perianal fistulas in Crohn's disease. Aliment Pharmacol Ther 18:1113–1120
Bell SJ, Halligan S, Windsor AC, Williams AB, Wiesel P, Kamm MA (2003) Response of fistulating Crohn's disease to infliximab treatment assessed by magnetic resonance imaging. Aliment Pharmacol Ther 17:387–393
Van Assche G, Vanbeckevoort D, Bielen D et al (2003) Magnetic resonance imaging of the effects of infliximab on perianal fistulizing Crohn's disease. Am J Gastroenterol 98:332–339
Panes J, Bouhnik Y, Reinisch W et al (2013) Imaging techniques for assessment of inflammatory bowel disease: joint ECCO and ESGAR evidence-based consensus guidelines. J Crohn's Colitis 7:556–585
Savoye-Collet C, Savoye G, Koning E, Dacher JN, Lerebours E (2011) Fistulizing perianal Crohn's disease: contrast-enhanced magnetic resonance imaging assessment at 1 year on maintenance anti-TNF-alpha therapy. Inflamm Bowel Dis 17:1751–1758
Horsthuis K, Lavini C, Bipat S, Stokkers PC, Stoker J (2009) Perianal Crohn disease: evaluation of dynamic contrast-enhanced MR imaging as an indicator of disease activity. Radiology 251:380–387
Ziech ML, Lavini C, Bipat S et al (2013) Dynamic contrast-enhanced MRI in determining disease activity in perianal fistulizing Crohn disease: a pilot study. AJR Am J Roentgenol 200:W170–W177
Tozer P, Ng SC, Siddiqui MR et al (2012) Long-term MRI-guided combined anti-TNF-α and thiopurine therapy for Crohn's perianal fistulas. Inflamm Bowel Dis 18:1825–1834
Savoye G, Savoye-Collet C (2010) How deep is remission in perianal Crohn's disease and do imaging modalities matter? Am J Gastroenterol 105:1445–1446
Tissot O, Bodnar D, Henry L, Dubreuil A, Valette PJ (1996) Ano-perineal fistula in MRI. Contribution of T2 weighted sequences]. [Article in French. J Radiol 77:253–260
Szurowska E, Wypych J, Izycka-Swieszewska E (2007) Perianal fistulas in Crohn’s disease: MRI diagnosis and surgical planning: MRI in fistulazing perianal Crohn’s disease. Abdom Imaging 32:705–718
Halligan S, Stoker J (2006) Imaging of fistula in ano. Radiology 239:18–33
Hori M, Oto A, Orrin S, Suzuki K, Baron RL (2009) Diffusion-weighted MRI: a new tool for the diagnosis of fistula in ano. J Magn Reson Imaging 30:1021–1026
Dohan A, Eveno C, Oprea R et al (2014) Diffusion-weighted MR imaging for the diagnosis of abscess complicating fistula-in-ano: preliminary experience. Eur Radiol 24:2906–2915
Yoshizako T, Wada A, Takahara T et al (2012) Diffusion-weighted MRI for evaluating perianal fistula activity: feasibility study. Eur J Radiol 81:2049–2053
Adler J, Swanson SD, Schmiedlin-Ren P et al (2011) Magnetization transfer helps detect intestinal fibrosis in an animal model of Crohn disease. Radiology 259:127–135
Dillman JR, Swanson SD, Johnson LA et al (2014) Comparison of noncontrast MRI magnetization transfer and T2 -Weighted signal intensity ratios for detection of bowel wall fibrosis in a Crohn's disease animal model. J Magn Reson Imaging. doi:10.1002/jmri.24815 [Epub ahead of print]
Pazahr S, Blume I, Frei P et al (2013) Magnetization transfer for the assessment of bowel fibrosis in patients with Crohn’s disease: initial experience. MAGMA 26:291–301
Adler J, Rahal K, Swanson SD et al (2013) Anti-tumor necrosis factor α prevents bowel fibrosis assessed by messenger RNA, histology, and magnetization transfer MRI in rats with Crohn’s disease. Inflamm Bowel Dis 19:683–690
Henkelman RM, Stanisz GJ, Graham SJ (2001) Magnetization transfer in MRI: a review. NMR Biomed 14:57–64
Wolff SD, Balaban RS (1994) Magnetization transfer imaging: practical aspects and clinical applications. Radiology 192:593–599
Parks AG, Gordon PH, Hardcastle JD (1976) A classification of fistula-in-ano. Br J Surg 63:1–12
Kumar V, Jagannathan NR, Kumar R et al (2008) Evaluation of the role of magnetization transfer imaging in prostate: a preliminary study. Magn Reson Imaging 26:644–649
Ng SC, Plamondon S, Gupta A et al (2009) Prospective evaluation of anti-tumor necrosis factor therapy guided by magnetic resonance imaging for Crohn’s perineal fistulas. Am J Gastroenterol 104:2973–2986
Acknowledgments
The authors are grateful to Nikki Sabourin-Gibbs, Rouen University Hospital, for her help in editing the manuscript. The scientific guarantor of this publication is Celine Savoye-Collet. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: diagnostic or prognostic study performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinson, C., Dolores, M., Cruypeninck, Y. et al. Magnetization transfer ratio for the assessment of perianal fistula activity in Crohn's disease. Eur Radiol 27, 80–87 (2017). https://doi.org/10.1007/s00330-016-4350-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-016-4350-2