Abstract
Objective
To investigate the high-resolution computed tomography (HRCT) features that distinguish lung adenocarcinomas in situ (AISs) and minimally invasive adenocarcinomas (MIAs) from invasive adenocarcinomas (IACs) appearing as ground-glass nodules (GGNs), and to select candidates for sublobar resection.
Methods
Two hundred and twenty-nine patients with 237 GGNs of less than 2 cm (139 AIS-MIA nodules and 98 IAC nodules) confirmed by surgery and pathology were retrospectively reviewed. The HRCT features of the AIS-MIAs and IACs were analysed and compared. Receiver operating characteristic (ROC) analyses were conducted to determine the cutoff values for the qualitative variables and their diagnostic performances.
Results
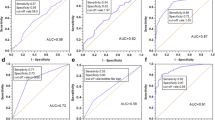
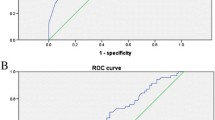
Significant differences were found in the density, nodule and solid component diameters, CT values of the ground-glass and solid components, lobulated shape, spiculated margin, abnormal pulmonary vein and artery, air bronchogram, and pleural indentation of the GGNs between the two groups. Multivariate and ROC analyses revealed that larger diameter of nodules (≥12.2 mm) and solid components (≥6.7 mm), and higher CT values of the solid components (≥ -192 HU) in the GGNs with air bronchogram were significantly associated with IACs.
Conclusions
HRCT can identify distinguishing morphological features between AIS-MIAs and IACs, and is helpful for selecting candidates for sublobar resection.
Key Points
• IACs appearing as GGNs were often ≥ 12.2 mm in diameter.
• IACs were often ≥ 6.7 mm in solid component diameter.
• The solid components of the IACs often exhibited ≥ -192 HU.
• IACs exhibited air bronchogram more frequently than AIS-MIAs.






Similar content being viewed by others
Abbreviations
- AIS:
-
Adenocarcinoma in situ
- MIA:
-
Minimally invasive adenocarcinoma
- IAC:
-
Invasive adenocarcinoma
- AAH:
-
Atypical adenomatous hyperplasia
- GGN:
-
Ground-glass nodule
- PGGN:
-
Pure ground-glass nodule
- MGGN:
-
Mixed ground-glass nodule
- HRCT:
-
High-resolution computed tomography
References
Nakata M, Saeki H, Takata I et al (2002) Focal ground-glass opacity detected by low-dose helical CT. Chest 121:1464–1467
Travis WD, Brambilla E, Noguchi M et al (2011) International association for the study of lung cancer/American thoracic society/European respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6:244–285
Zhang J, Wu J, Tan Q, Zhu L, Gao W (2013) Why do pathological stage IA lung adenocarcinomas vary from prognosis? A clinicopathologic study of 176 patients with pathological stage IA lung adenocarcinoma based on the IASLC/ATS/ERS classification. J Thorac Oncol 8:1196–1202
Van Schil PE, Asamura H, Rusch VW et al (2012) Surgical implications of the new IASLC/ATS/ERS adenocarcinoma classification. Eur Respir J 39:478–486
Tsutani Y, Miyata Y, Nakayama H et al (2014) Appropriate sublobar resection choice for ground glass opacity-dominant clinical stage IA lung adenocarcinoma wedge resection or segmentectomy. Chest 145:66–71
EI-Sherif A, Gooding WE, Santos R et al (2006) Outcomes of sublobar resection versus lobectomy for stage I non-small cell lung cancer: A 13-year analysis. Ann Thorac Surg 82:408–416
Altorki NK, Yip R, Hanaoka T et al (2014) Sublobar resection is equivalent to lobectomy for clinical stage IA lung cancer in solid nodules. J Thorac Cardiovasc Surg 147:754–762
Donahue JM, Morse CR, Wigle DA et al (2012) Oncologic efficacy of anatomic segmentectomy in stage IA lung cancer patients with T1a tumors. Ann Thorac Surg 2012(93):381–388
Nomori H, Iwatani K, Kobayashi H, Mori A, Yoshioka S (2006) Omission of mediastinal lymph node dissection in lung cancer: its techniques and diagnostic procedures. Ann Thorac Cardiovasc Surg 12:83–88
Nakahara R, Yokose T, Nagai K, Nishiwaki Y, Ochiai A (2001) Atypical adenomatous hyperplasia of the lung: a clinicopathological study of 118 cases including cases with multiple atypical adenomatous hyperplasia. Thorax 56:302–305
Zhang Y, Qiang JW, Ye JD, Ye XD, Zhang J (2014) High resolution CT in differentiating minimally invasive component in early lung adenocarcinoma. Lung Cancer 84:236–241
Kim HY, Shim YM, Lee KS, Han J, Yi CA, Kim YK (2007) Persistent pulmonary nodular ground-glass opacity at thin-section CT: histopathologic comparisons. Radiology 245:267–275
Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH (2013) Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology 268:265–273
Eguchi T, Yoshizawa A, Kawakami S et al (2014) Tumor size and computed tomography attenuation of pulmonary pure ground-glass nodules are useful for predicting pathological invasiveness. PLoS ONE 9:e97867
Liu LH, Liu M, Wei R et al (2015) CT findings of persistent pure ground glass opacity: can we predict the invasiveness? Asian Pac J Cancer Prev 16:1925–1928
Cohen JG, Reymond E, Lederlin M et al (2015) Differentiating pre- and minimally invasive from invasive adenocarcinoma using CT-features in persistent pulmonary part-solid nodules in Caucasian patients. Eur J Radiol 84:738–744
Lee HK, Goo JM, Park SJ et al (2014) Correlation between the size of the solid component on thin-section CT and the invasive component on pathology in small lung adenocarcinomas manifesting as ground-glass nodules. J Thorac Oncol 9:74–82
Noguchi M, Morikawa A, Kawasaki M et al (1995) Small adenocarcinoma of the lung - histologic characteristics and prognosis. Cancer 75:2844–2852
Park CM, Goo JM, Lee HJ, Lee CH, Chun EJ, Im JG (2007) Nodular ground-glass opacity at thin-section CT: histologic correlation and evaluation of change at follow up. RadioGraphics 27:391–408
Lee HJ, Goo JM, Lee CH et al (2009) Predictive CT findings of malignancy in ground-glass nodules on thin-section chest CT: the effects on radiologist performance. Eur Radiol 19:552–560
Gao F, Li M, Ge XJ et al (2013) Multi-detector spiral CT study of the relationships between pulmonary ground-glass nodules and blood vessels. Eur Radiol 23:3271–3277
Qiang JW, Zhou KR, Lu G et al (2004) The relationship between solitary pulmonary nodule and bronchus: MSCT-pathologic correlation. Clin Radiol 59:1121–1127
Cui Y, Ma DQ, Liu WH (2009) Value of multiplanar reconstruction in MSCT in demonstrating the relationship between solitary pulmonary nodule and bronchus. Clin Imaging 33:15–21
Yoshino I, Nakanishi R, Kodate M et al (2000) Pleural retraction and intra-tumoral air-bronchogram as prognostic factors for stage I pulmonary adenocarcinoma following complete resection. Int Surg 85:105–112
Yamazaki K, Yoshino I, Yohena T et al (2007) Clinically predictive factors of pathologic upstaging in patients with peripherally located clinical stage IA non-small cell lung cancer. Lung Cancer 55:365–369
Ikehara M, Saito H, Kondo T et al (2012) Comparison of thin-section CT and pathological findings in small solid-density type pulmonary adenocarcinoma: prognostic factors from CT findings. Eur J Radiol 81:189–194
Acknowledgments
The scientific guarantor of this publication is Jin Wei Qiang. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by grants from national natural science foundation of China (81171340) and Science and Technology Commission of Shanghai (10411956800). One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: retrospective, diagnostic or prognostic study, performed at one institution.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Zhang, Y., Shen, Y., Qiang, J.W. et al. HRCT features distinguishing pre-invasive from invasive pulmonary adenocarcinomas appearing as ground-glass nodules. Eur Radiol 26, 2921–2928 (2016). https://doi.org/10.1007/s00330-015-4131-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4131-3