Abstract
Objective
To investigate whether a trained group of technicians using a modified breathing command during gadoxetate-enhanced liver MRI reduces respiratory motion artefacts compared to non-trained technicians using a traditional breathing command.
Materials and methods
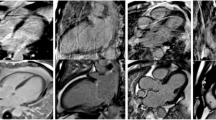
The gadoxetate-enhanced liver MR images of 30 patients acquired using the traditional breathing command and the subsequent 30 patients after training the technicians to use a modified breathing command were analyzed. A subgroup of patients (n = 8) underwent scans both by trained and untrained technicians. Images obtained using the traditional and modified breathing command were compared for the presence of breathing artefacts [respiratory artefact-based image quality scores from 1 (best) to 5 (non-diagnostic)].
Results
There was a highly significant improvement in the arterial phase image quality scores in patients using the modified breathing command compared to the traditional one (P < 0.001). The percentage of patients with severe and extensive breathing artefacts in the arterial phase decreased from 33.3 % to 6.7 % after introducing the modified breathing command (P = 0.021). In the subgroup that underwent MRI using both breathing commands, arterial phase image quality improved significantly (P = 0.008) using the modified breathing command.
Conclusion
Training technicians to use a modified breathing command significantly improved arterial phase image quality of gadoxetate-enhanced liver MRI.
Key Points
• A modified breathing command reduced respiratory artefacts on arterial-phase gadoxetate-enhanced MRI (P < 0.001).
• The modified command decreased severe and extensive arterial-phase breathing artefacts (P = 0.021).
• Training technicians to use a modified breathing command improved arterial-phase images.



Similar content being viewed by others
References
Thian YL, Riddell AM, Koh DM (2013) Liver-specific agents for contrast-enhanced MRI: role in oncological imaging. Cancer Imaging 13:567
Van Beers BE, Pastor CM, Hussain HK (2012) Primovist, Eovist: what to expect? J Hepatol 57:421–429
Kim B, Byun J, Kim H et al (2015) Enhancement patterns and pseudo-washout of hepatic haemangiomas on gadoxetate disodium-enhanced liver MRI. Eur Radiol. doi:10.1007/s00330-015-3798-9
Kim R, Lee J, Shin CI et al (2015) Differentiation of intrahepatic mass-forming cholangiocarcinoma from hepatocellular carcinoma on gadoxetic acid-enhanced liver MR imaging. Eur Radiol. doi:10.1007/s00330-015-4005-8
Song K, Kim S, Lim H, Jung SH, Sohn I, Kim H (2015) Subcentimeter hypervascular nodule with typical imaging findings of hepatocellular carcinoma in patients with history of hepatocellular carcinoma: natural course on serial gadoxetic acid-enhanced MRI and diffusion-weighted imaging. Eur Radiol 25:2789–2796
Scharitzer M, Ba-Ssalamah A, Ringl H et al (2013) Preoperative evaluation of colorectal liver metastases: comparison between gadoxetic acid-enhanced 3.0-T MRI and contrast-enhanced MDCT with histopathological correlation. Eur Radiol 23:2187–2196
Koh J, Chung Y, Nahm J et al (2015) Intrahepatic mass-forming cholangiocarcinoma: prognostic value of preoperative gadoxetic acid-enhanced MRI. Eur Radiol. doi:10.1007/s00330-015-3846-5
Joo I, Lee J, Lee D, Jeon J, Han J, Choi B (2015) Noninvasive diagnosis of hepatocellular carcinoma on gadoxetic acid-enhanced MRI: can hypointensity on the hepatobiliary phase be used as an alternative to washout? Eur Radiol 25:2859–2868
Davenport MS, Viglianti BL, Al-Hawary MM et al (2013) Comparison of acute transient dyspnea after intravenous administration of gadoxetate disodium and gadobenate dimeglumine: effect on arterial phase image quality. Radiology 266:452–461
Davenport MS, Caoili EM, Kaza RK, Hussain HK (2014) Matched within-patient cohort study of transient arterial phase respiratory motion–related artifact in MR imaging of the liver: gadoxetate disodium versus gadobenate dimeglumine. Radiology 272:123–131
Davenport MS, Bashir MR, Pietryga JA, Weber JT, Khalatbari S, Hussain HK (2014) Dose-toxicity relationship of gadoxetate disodium and transient severe respiratory motion artifact. Am J Roentgenol 203:796–802
Pietryga JA, Burke LMB, Marin D, Jaffe TA, Bashir MR (2014) Respiratory motion artifact affecting hepatic arterial phase imaging with gadoxetate disodium: examination recovery with a multiple arterial phase acquisition. Radiology 271:426–434
Bashir MR, Castelli P, Davenport MS et al (2015) Respiratory motion artifact affecting hepatic arterial phase MR imaging with gadoxetate disodium is more common in patients with a prior episode of arterial phase motion associated with gadoxetate disodium. Radiology 274:141–148
Motosugi U (2015) Gadoxetic acid-induced acute transient dyspnea: the perspective of japanese radiologists. Magn Reson Med Sci 14:163–164
Bergmann K, Agris J, Balzer T (2013) Does intravenous administration of gadoxetate disodium have any effect on breath-hold times. Radiology 268:926–927
Hayashi T, Saitoh S, Tsuji Y et al (2015) Influence of gadoxetate disodium on oxygen saturation and heart rate during dynamic contrast-enhanced MR imaging. Radiology 276:756–765
Luetkens J, Kupczyk P, Doerner J et al (2015) Respiratory motion artefacts in dynamic liver MRI: a comparison using gadoxetate disodium and gadobutrol. Eur Radiol. doi:10.1007/s00330-015-3736-x
Fujinaga Y, Ohya A, Tokoro H et al (2014) Radial volumetric imaging breath-hold examination (VIBE) with k-space weighted image contrast (KWIC) for dynamic gadoxetic acid (Gd-EOB-DTPA)-enhanced MRI of the liver: advantages over cartesian VIBE in the arterial phase. Eur Radiol 24:1290–1299
Chandarana H, Feng L, Ream J et al (2015) Respiratory motion-resolved compressed sensing reconstruction of free-breathing radial acquisition for dynamic liver magnetic resonance imaging. Investig Radiol. doi:10.1097/RLI.0000000000000179
Budjan J, Ong M, Riffel P et al (2014) CAIPIRINHA-Dixon-TWIST (CDT)-volume-interpolated breath-hold examination (VIBE) for dynamic liver imaging: comparison of gadoterate meglumine, gadobutrol and gadoxetic acid. Eur J Radiol 83:2007–2012
Acknowledgments
The scientific guarantor of this publication is Andreas Gutzeit. The authors of this manuscript declare relationships with the following companies: Johannes M. Froehlich works as a consultant for a contrast media company. The other authors had full control of data and information that might have represented a conflict of interest for the author who is a consultant of a company. The authors state that this work has not received any funding. The professional biostatistician Nicole Graf (www.biostatistics.ch) kindly provided statistical advice for this manuscript. The institutional review board had generally approved retrospective studies. Written informed consent concerning anonymized data evaluation had been obtained from all subjects (patients) in this study. Neither this cohort nor a subset thereof has been published elsewhere. Methodology: retrospective, observational, performed at one institution. We would like to thank our innovative and wonderful technician team, who helped us examine all the patients: Sara Schwarz MT, Sarah Suter MT, Florentina Podrimaj MT, Christian Meier MT, Barbara Eichenberger MT and Katrin Pucher MT. We would also like to thank Rene Patzwahl MD, who gave us the idea for this project after intense discussion of the first paper by Davenport et al. [9].
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gutzeit, A., Matoori, S., Froehlich, J.M. et al. Reduction in respiratory motion artefacts on gadoxetate-enhanced MRI after training technicians to apply a simple and more patient-adapted breathing command. Eur Radiol 26, 2714–2722 (2016). https://doi.org/10.1007/s00330-015-4086-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-4086-4