Abstract
Objectives
Lung cancer risk models should be externally validated to test generalizability and clinical usefulness. The Danish Lung Cancer Screening Trial (DLCST) is a population-based prospective cohort study, used to assess the discriminative performances of the PanCan models.
Methods
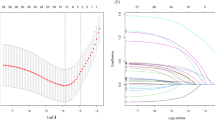
From the DLCST database, 1,152 nodules from 718 participants were included. Parsimonious and full PanCan risk prediction models were applied to DLCST data, and also coefficients of the model were recalculated using DLCST data. Receiver operating characteristics (ROC) curves and area under the curve (AUC) were used to evaluate risk discrimination.
Results
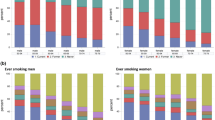
AUCs of 0.826–0.870 were found for DLCST data based on PanCan risk prediction models. In the DLCST, age and family history were significant predictors (p = 0.001 and p = 0.013). Female sex was not confirmed to be associated with higher risk of lung cancer; in fact opposing effects of sex were observed in the two cohorts. Thus, female sex appeared to lower the risk (p = 0.047 and p = 0.040) in the DLCST.
Conclusions
High risk discrimination was validated in the DLCST cohort, mainly determined by nodule size. Age and family history of lung cancer were significant predictors and could be included in the parsimonious model. Sex appears to be a less useful predictor.
Key points
• High accuracy in logistic modelling for lung cancer risk stratification of nodules.
• Lung cancer risk prediction is primarily based on size of pulmonary nodules.
• Nodule spiculation, age and family history of lung cancer are significant predictors.
• Sex does not appear to be a useful risk predictor.



Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- BCCA:
-
British Columbia Cancer Agency
- CT:
-
Computed tomography
- DLCST:
-
Danish Lung Cancer Screening Trial
- NLST:
-
National Lung Screening Trial
- OR:
-
Odds ratio
- PanCan:
-
Pan-Canadian Early Detection of Lung Cancer Study
- ROC:
-
Receiver operating characteristics
- SD:
-
Standard deviation
References
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 2:74–108
Aberle DR, Adams AM, Berg CD et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 5:395–409
Bach PB, Mirkin JN, Oliver TK et al (2012) Benefits and harms of CT screening for lung cancer: a systematic review. JAMA 22:2418–2429
Bach PB, Kattan MW, Thornquist MD et al (2003) Variations in lung cancer risk among smokers. J Natl Cancer Inst 6:470–478
Spitz MR, Hong WK, Amos CI et al (2007) A risk model for prediction of lung cancer. J Natl Cancer Inst 9:715–726
Spitz MR, Etzel CJ, Dong Q et al (2008) An expanded risk prediction model for lung cancer. Cancer Prev Res (Phila) 4:250–254
Cassidy A, Myles JP, Liloglou T, Duffy SW, Field JK (2006) Defining high-risk individuals in a population-based molecular-epidemiological study of lung cancer. Int J Oncol 5:1295–1301
Tammemagi CM, Pinsky PF, Caporaso NE et al (2011) Lung cancer risk prediction: prostate, lung, colorectal and ovarian cancer screening trial models and validation. J Natl Cancer Inst 13:1058–1068
Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES (1997) The probability of malignancy in solitary pulmonary nodules. Application to small radiologically indeterminate nodules. Arch Intern Med 8:849–855
Gould MK, Ananth L, Barnett PG (2007) A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest 2:383–388
Li Y, Wang J (2012) A mathematical model for predicting malignancy of solitary pulmonary nodules. World J Surg 4:830–835
McWilliams A, Tammemagi MC, Mayo JR et al (2013) Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med 10:910–919
Wille MM, Thomsen LH, Dirksen A et al (2014) Emphysema progression is visually detectable in low-dose CT in continuous but not in former smokers. Eur Radiol 24:2692–2699
Pedersen JH, Ashraf H, Dirksen A et al (2009) The Danish randomized lung cancer CT screening trial–overall design and results of the prevalence round. J Thorac Oncol 5:608–614
Tas F, Ciftci R, Kilic L, Karabulut S (2013) Age is a prognostic factor affecting survival in lung cancer patients. Oncol Lett 5:1507–1513
Cote ML, Liu M, Bonassi S et al (2012) Increased risk of lung cancer in individuals with a family history of the disease: a pooled analysis from the International Lung Cancer Consortium. Eur J Cancer 13:1957–1968
Pauk N, Kubik A, Zatloukal P, Krepela E (2005) Lung cancer in women. Lung Cancer 1:1–9
Belani CP, Marts S, Schiller J, Socinski MA (2007) Women and lung cancer: epidemiology, tumor biology, and emerging trends in clinical research. Lung Cancer 1:15–23
Mizuno S, Takiguchi Y, Fujikawa A et al (2009) Chronic obstructive pulmonary disease and interstitial lung disease in patients with lung cancer. Respirology 3:377–383
Wilson DO, Weissfeld JL, Balkan A et al (2008) Association of radiographic emphysema and airflow obstruction with lung cancer. Am J Respir Crit Care Med 7:738–744
Acknowledgments
The scientific guarantor of this publication is Asger Dirksen. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. Bram Van Ginneken works for Fraunhofer MEVIS in Bremen, Germany. This study has received funding by The Danish Ministry of Health and AstraZeneca. One of the authors has significant statistical expertise. Institutional review board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Some study subjects have been previously reported in DLCST studies regarding lung cancer screening, lung function, lung density, airway segmentation, and visual assessment of emphysema, airway abnormalities and interstitial abnormalities in the Danish Lung Cancer Screening Trial. However, analyses of this study are new and have not been published before. All relevant references are disclosed. Methodology: prospective, diagnostic study, performed at two institutions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Winkler Wille, M.M., van Riel, S.J., Saghir, Z. et al. Predictive Accuracy of the PanCan Lung Cancer Risk Prediction Model -External Validation based on CT from the Danish Lung Cancer Screening Trial. Eur Radiol 25, 3093–3099 (2015). https://doi.org/10.1007/s00330-015-3689-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3689-0