Abstract
Objectives
We aimed to retrospectively investigate CT findings of minimally invasive adenocarcinoma (MIA) and to determine the appropriate method for measurement of solid portions in MIAs at CT.
Methods
From May 2012 to April 2014, 55 pulmonary nodules in 52 patients were pathologically confirmed as MIAs and were included in this study. CT findings of MIAs and measurements of solid portions at CT were evaluated by two independent radiologists.
Results
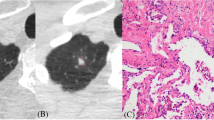
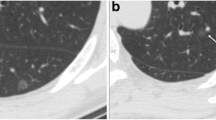
Mean size of MIAs was 10.5 mm ± 4.8 (range, 4–28 mm). Fifty-two MIAs manifested as 28 pure ground glass nodules (GGNs) (53.8 % %), 22 part-solid GGNs (42.3 % %), and 2 two solid nodules (3.8 % %) at CT. Lobulated border, bubble lucency, and pleural retraction were frequently found in both observers (26.9–42.3 % %). Differences according to window settings between solid portion size and invasive component size were not significantly different in both observers (p > 0.05). As for interobserver agreement, 95 % CIs for solid portion size in the mediastinal window setting (-2.2 to 3.4; mean, 0.6) were slightly narrower than those in the lung window setting (-2.6 to 3.1; mean, 0.3).
Conclusions
Nearly all MIAs appear as pure and part-solid GGNs. Mediastinal and lung window settings can be applied for measurement of solid portions at CT without a significant difference.
Key Points
• Nearly all MIAs appear as pure and part-solid GGNs.
• MIAs show frequent interval growth at follow-up.
• MIAs with solid portion ≥5 mm ranged from 7.7 % to 19.2 %.
• Mediastinal and lung window settings can be applied for solid portion measurement.




Similar content being viewed by others
Abbreviations
- MIA:
-
minimally invasive adenocarcinoma
- GGN:
-
ground glass nodule
- IASLC:
-
International Association for the Study of Lung Cancer
- ATS:
-
American Thoracic Society
- ERS:
-
European Respiratory Society
- AAH:
-
atypical adenomatous hyperplasia
- AIS:
-
adenocarcinoma in situ
References
Travis WD, Brambilla E, Noguchi M et al (2011) International association for the study of lung cancer/american thoracic society/european respiratory society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6:244–285
Travis WD, Garg K, Franklin WA et al (2005) Evolving concepts in the pathology and computed tomography imaging of lung adenocarcinoma and bronchioloalveolar carcinoma. J Clin Oncol 23:3279–3287
Borczuk AC, Qian F, Kazeros A et al (2009) Invasive size is an independent predictor of survival in pulmonary adenocarcinoma. Am J Surg Pathol 33:462–469
Goo JM, Park CM, Lee HJ (2011) Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR Am J Roentgenol 196:533–543
Park CM, Goo JM, Lee HJ, Lee CH, Chun EJ, Im JG (2007) Nodular ground-glass opacity at thin-section CT: histologic correlation and evaluation of change at follow-up. Radiographics 27:391–408
Zhang Y, Qiang JW, Ye JD, Zhang J (2014) High resolution CT in differentiating minimally invasive component in early lung adenocarcinoma. Lung Cancer 84:236–241
El-Sherif A, Gooding WE, Santos R et al (2006) Outcomes of sublobar resection versus lobectomy for stage I non-small cell lung cancer: a 13-year analysis. Ann Thorac Surg 82:408–415, discussion 415-416
Nakamura H, Kawasaki N, Taguchi M, Kabasawa K (2005) Survival following lobectomy vs limited resection for stage I lung cancer: a meta-analysis. Br J Cancer 92:1033–1037
Okada M, Koike T, Higashiyama M, Yamato Y, Kodama K, Tsubota N (2006) Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 132:769–775
Tsutani Y, Miyata Y, Nakayama H et al (2014) Appropriate sublobar resection choice for ground glass opacity-dominant clinical stage IA lung adenocarcinoma: wedge resection or segmentectomy. Chest 145:66–71
Naidich DP, Bankier AA, MacMahon H et al (2013) Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society. Radiology 266:304–317
Grills IS, Fitch DL, Goldstein NS et al (2007) Clinicopathologic analysis of microscopic extension in lung adenocarcinoma: defining clinical target volume for radiotherapy. Int J Radiat Oncol Biol Phys 69:334–341
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1:307–310
Lee KH, Goo JM, Park SJ et al (2014) Correlation between the size of the solid component on thin-section CT and the invasive component on pathology in small lung adenocarcinomas manifesting as ground-glass nodules. J Thorac Oncol 9:74–82
Lim HJ, Ahn S, Lee KS et al (2013) Persistent pure ground-glass opacity lung nodules >/= 10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest 144:1291–1299
Lee SM, Park CM, Goo JM, Lee HJ, Wi JY, Kang CH (2013) Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology 268:265–273
Park CM, Goo JM, Lee HJ et al (2006) CT findings of atypical adenomatous hyperplasia in the lung. Korean J Radiol 7:80–86
Lee HJ, Goo JM, Lee CH, Yoo CG, Kim YT, Im JG (2007) Nodular ground-glass opacities on thin-section CT: size change during follow-up and pathological results. Korean J Radiol 8:22–31
Gandara DR, Aberle D, Lau D et al (2006) Radiographic imaging of bronchioloalveolar carcinoma: screening, patterns of presentation and response assessment. J Thorac Oncol 1:S20–S26
Asamura H (2008) Minimally invasive approach to early, peripheral adenocarcinoma with ground-glass opacity appearance. Ann Thorac Surg 85:S701–S704
Yoshizawa A, Motoi N, Riely GJ et al (2011) Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol 24:653–664
Acknowledgments
The scientific guarantor of this publication is Dr. Jin Mo Goo. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by grant no 2013-0507 from the SK Telecom Research Fund. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was waived by the Institutional Review Board. Methodology: retrospective, observational, performed at one institution.
Conflict of interest
All authors have no conflicts to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, S.M., Goo, J.M., Lee, K.H. et al. CT findings of minimally invasive adenocarcinoma (MIA) of the lung and comparison of solid portion measurement methods at CT in 52 patients. Eur Radiol 25, 2318–2325 (2015). https://doi.org/10.1007/s00330-015-3616-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3616-4