Abstract
Objectives
To investigate the frequency of pancreatic duct (PD) variants and their effect on pancreatic exocrine function in a population-based study using non-invasive secretin-stimulated magnetic resonance cholangiopancreatography (sMRCP).
Methods
Nine hundred and ninety-five volunteers, 457 women and 538 men, aged 51.9 ± 13.4 years, underwent navigator-triggered, T2-weighted, 3D turbo spin echo MRCP on a 1.5 T system after 1 unit/kg secretin administration. Two readers evaluated images for PD variants. Pancreatic exocrine function and morphological signs of chronic pancreatitis such as abnormalities of the main PD, side branch dilatation, and pancreatic cysts were evaluated and related to PD variants using a Kruskal-Wallis test and post hoc analysis.
Results
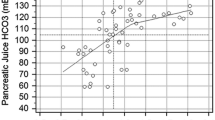
Of all sMRCP, 93.2 % were of diagnostic quality. Interobserver reliability for detection of PD variants was found to be kappa 0.752 (95 %CI, 0.733 – 0.771). Normal PD variants were observed in 90.4 % (n = 838/927). Variants of pancreas divisum was identified in 9.6 % (n = 89/927). Abnormalities of the main PD, side branch dilatation, and pancreatic cysts were observed in 2.4 %, 16.6 %, and 27.7 %, respectively, and were not significantly different between pancreas divisum and non-divisum group (P = 0.122; P = 0.152; P = 0.741). There was no association between PD variants and pancreatic exocrine function (P = 0.367).
Conclusion
PD variants including pancreas divisum are not associated with morphological signs of chronic pancreatitis or restriction of pancreatic exocrine function.
Key Points
• MRCP allows the evaluation of pancreatic duct variants and morphological change.
• Pancreatic duct variants are not associated with morphological signs of chronic pancreatitis.
• Pancreas divisum is not accompanied by restriction of pancreatic exocrine function.
• Pancreatic duct variants including pancreas divisum are limited in their clinical relevance.


Similar content being viewed by others
Abbreviations
- PD:
-
Pancreatic duct
- sMRCP:
-
Secretin-stimulated magnetic resonance cholangiopancreatography
- CP:
-
Chronic pancreatitis
- MRCP:
-
Magnetic resonance cholangiopancreatography
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- MRI:
-
Magnetic resonance imaging
- TSE:
-
Turbo spin echo
- MIP:
-
Maximum-intensity projection
- APD:
-
Accessory pancreatic duct
- MPD:
-
Main pancreatic duct
- CBD:
-
Common bile duct
- TEV:
-
Total excreted volume
- PFO:
-
Pancreatic flow output
- BMI:
-
Body mass index
References
Mayerle J, Lerch MM (2007) Is it necessary to distinguish between alcoholic and nonalcoholic chronic pancreatitis? J Gastroenterol 42:127–130
Lerch MM, Mayerle J (2013) 50 years of progress in pathophysiology, diagnosis and treatment of chronic pancreatitis. Z Gastroenterol 51:358–362
Dufour MC, Adamson MD (2003) The epidemiology of alcohol-induced pancreatitis. Pancreas 27:286–290
Lowenfels AB, Maisonneuve P, Cavallini G et al (1994) Prognosis of chronic pancreatitis: an international multicenter study. International Pancreatitis Study Group. Am J Gastroenterol 89:1467–1471
Klöppel G, Maillet B (1995) Development of chronic pancreatitis from acute pancreatitis: a pathogenetic concept. Zentralbl Chir 120:274–277
Bret PM, Reinhold C, Taourel P et al (1996) Pancreas divisum: evaluation with MR cholangiopancreatography. Radiology 199:99–103
Takehara Y, Ichijo K, Tooyama N et al (1995) Enhanced delineation of the pancreatic duct in MR cholangiopancreatography (MRCP) with a combined use of secretin. Nihon Igaku Hoshasen Gakkai Zasshi 55:255–256
Matos C, Metens T, Devière J et al (2001) Pancreas divisum: evaluation with secretin-enhanced magnetic resonance cholangiopancreatography. Gastrointest Endosc 53:728–733
Mosler P, Akisik F, Sandrasegaran K et al (2012) Accuracy of magnetic resonance cholangiopancreatography in the diagnosis of pancreas divisum. Dig Dis Sci 57:170–174
Manfredi R, Costamagna G, Brizi MG et al (2000) Severe chronic pancreatitis versus suspected pancreatic disease: dynamic MR cholangiopancreatography after secretin stimulation. Radiology 214:849–855
Bali MA, Sztantics A, Metens T et al (2005) Quantification of pancreatic exocrine function with secretin-enhanced magnetic resonance cholangiopancreatography: normal values and short-term effects of pancreatic duct drainage procedures in chronic pancreatitis. Initial results. Eur Radiol 15:2110–2121
Bali MA, Sontou R, Arvanitakis M et al (2007) Evaluation of the stimulating effect of a low dose of secretin compared to the standard dose on the exocrine pancreas with MRCP: preliminary results in normal subjects (MRCP quantification of secretin stimulation). Abdom Imaging 32:743–748
Heverhagen JT, Müller D, Battmann A et al (2001) MR hydrometry to assess exocrine function of the pancreas: initial results of noninvasive quantification of secretion. Radiology 218:61–67
Hegenscheid K, Kühn J, Völzke H, et al. (2009) Whole-body magnetic resonance imaging of healthy volunteers: pilot study results from the population-based SHIP study. Fortschr Röntgenstr 181:748–759
Völzke H, Alte D, Schmidt CO, et al. (2011) Cohort profile: the study of health in Pomerania. Int J Epidemiol 40:294–307
Yu J, Turner MA, Fulcher AS, Halvorsen RA (2006) Congenital anomalies and normal variants of the pancreaticobiliary tract and the pancreas in adults: part 2, pancreatic duct and pancreas. AJR Am J Roentgenol 187:1544–1553
Akisik MF, Sandrasegaran K, Aisen AA et al (2006) Dynamic secretin-enhanced MR cholangiopancreatography. Radiographics 26:665–677
Matos C, Metens T, Devière J et al (1997) Pancreatic duct: morphologic and functional evaluation with dynamic MR pancreatography after secretin stimulation. Radiology 203:435–441
Cappeliez O, Delhaye M, Devière J et al (2000) Chronic pancreatitis: evaluation of pancreatic exocrine function with MR pancreatography after secretin stimulation. Radiology 215:358–364
Mensel B, Messner P, Mayerle J et al (2014) Secretin-stimulated MRCP in volunteers: assessment of safety, duct visualization, and pancreatic exocrine function. AJR Am J Roentgenol 202:102–108
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Hoffmeister A, Mayerle J, Dathe K, et al. (2012) [Method report to the S3 guideline chronic pancreatitis: definition, etiology, diagnostics and conservative, interventional endoscopic and surgical therapy of the chronic pancreatitis]. In: Z Gastroenterol. pp 1225–1236
Stimec B, Bulajić M, Korneti V et al (1996) Ductal morphometry of ventral pancreas in pancreas divisum. Comparison between clinical and anatomical results. Ital J Gastroenterol 28:76–80
Bühler H, Seefeld U, Deyhle P et al (1983) Clinical significance of pancreas divisum. Schweiz Med Wochenschr 113:320–324
Sarner M, Cotton PB (1984) Classification of pancreatitis. Gut 25:756–759
Axon AT (1989) Endoscopic retrograde cholangiopancreatography in chronic pancreatitis. Cambridge classification. Radiol Clin N Am 27:39–50
Walsh TN, Rode J, Theis BA, Russell RC (1992) Minimal change chronic pancreatitis. Gut 33:1566–1571
Layer P, Yamamoto H, Kalthoff L et al (1994) The different courses of early- and late-onset idiopathic and alcoholic chronic pancreatitis. Gastroenterology 107:1481–1487
Pezzilli R (2012) Pancreas divisum and acute or chronic pancreatitis. JOP 13:118–119
Delhaye M, Engelholm L, Cremer M (1985) Pancreas divisum: congenital anatomic variant or anomaly? Contribution of endoscopic retrograde dorsal pancreatography. Gastroenterology 89:951–958
Bernard JP, Sahel J, Giovannini M, Sarles H (1990) Pancreas divisum is a probable cause of acute pancreatitis: a report of 137 cases. Pancreas 5:248–254
Morgan DE, Logan K, Baron TH et al (1999) Pancreas divisum: implications for diagnostic and therapeutic pancreatography. AJR Am J Roentgenol 173:193–198
Rustagi T, Golioto M (2013) Diagnosis and therapy of pancreas divisum by ERCP: a single center experience. J Dig Dis 14:93–99
Nicholson JA, Johnstone M, Greenhalf W (2012) Divisum may be preserving pancreatic function in CFTR patients-but at a cost. Am J Gastroenterol 107:1758–1759
DiMagno MJ, Dimagno EP (2012) Pancreas divisum does not cause pancreatitis, but associates with CFTR mutations. Am J Gastroenterol 107:318–320
Bertin C, Pelletier A-L, Vullierme MP et al (2012) Pancreas divisum is not a cause of pancreatitis by itself but acts as a partner of genetic mutations. Am J Gastroenterol 107:311–317
Cavestro GM, Zuppardo RA, Bertolini S et al (2010) Connections between genetics and clinical data: role of MCP-1, CFTR, and SPINK-1 in the setting of acute, acute recurrent, and chronic pancreatitis. Am J Gastroenterol 105:199–206
Garg PK, Khajuria R, Kabra M, Shastri SS (2009) Association of SPINK1 gene mutation and CFTR gene polymorphisms in patients with pancreas divisum presenting with idiopathic pancreatitis. J Clin Gastroenterol 43:848–852
Acknowledgements
The scientific guarantor of this publication is: Jens-Peter Kühn, MD, PhD; Department of Radiology and Neuroradiology, University Medicine, Ernst Moritz Arndt University Greifswald Ferdinand-Sauerbruch-Straße 1 Greifswald 17475, Germany. kuehn@uni-greifswald.de. The authors of this manuscript declare relationships with the following companies: the Eva Luise and Horst Köhler Foundation, by the Deutsche Krebshilfe/Dr.Mildred-Scheel-Stiftung (109102), the Deutsche Forschungsgemeinschaft (DFG GRK840-D2/E3/E4, MA 4115/1-2/3, EV 168/2-1), the Federal Ministry of Education and Research (BMBF GANI-MED 03IS2061A and BMBF 0314107, 01ZZ9603, 01ZZ0103, 01ZZ0403, 03ZIK012), and the European Union (EU-FP-7: EPC-TM and EU-FP7-REGPOT-2010-1). This study has received funding by: the Community Medicine Research net (CMR) of the University of Greifswald, Germany. The CMR encompasses several research projects that share data from the population-based SHIP project (http://ship.community-medicine.de).
SHIP is funded by following institutions: Federal Ministry of Education and Research (grants 01ZZ9603, 01ZZ0103, 01ZZ0403, 01ZZ0701, 03ZIK012), Ministry of Cultural Affairs as well as the Social Ministry of the Federal State of Mecklenburg-West Pomerania, Federal Ministry of Nutrition, Agriculture and Consumer’s Safety (07HS003), German Research Foundation (projects Gr 1912/5-1, Ko 799/5-1, Vo 955/5-1, Vo 955/6-1, Vo 955/10-1), Competence Network Heart Failure (01GI0205), Competence Network Diabetes (01GI0855), German Asthma and COPD Network (COSYCONET; BMBF 01GI0883), Genopathomik (BMBF FZK 03138010), Alfried Krupp von Bohlen und Halbach Foundation, Alexander v. Humboldt Foundation, Leibniz Society, Siemens AG, Health Care Sector (Erlangen, Germany), Pfizer Pharma GmbH (SBU Endocrinology and Ophthalmology; Berlin Germany), Novo Nordisk (Mainz, Germany), Data Input GmbH (Darmstadt, Germany), GABA International AG (Therwil, Switzerland), Imedos Systems (Jena, Germany), and Heinen and Löwenstein (Bad Ems, Germany). No complex statistical methods were necessary for this paper. Institutional review board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. The local ethics committee approved the study, and written informed consent was obtained from all participating volunteers before secretin-stimulated MRCP.
Approval from the institutional animal care committee was not required because animals were not part of the study. Some study subjects or cohorts have been previously reported in: the population-based Study of Health in Pomerania (SHIP), which is a project conducted in Northeast Germany. The objectives of this interdisciplinary study are to estimate the occurrence of diseases findings and further associations.
The method for calculation of pancreatic flow output was previously published in Mensel et al. 2014. (Mensel B, Messner P, Mayerle J, et al. (2014) Secretin-Stimulated MRCP in Volunteers: Assessment of Safety, Duct Visualization, and Pancreatic Exocrine Function. AJR Am J Roentgenol 202: 102-108. Doi: 10.2214/AJR.12.10271
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bülow, R., Simon, P., Thiel, R. et al. Anatomic variants of the pancreatic duct and their clinical relevance: an MR-guided study in the general population. Eur Radiol 24, 3142–3149 (2014). https://doi.org/10.1007/s00330-014-3359-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3359-7