Abstract
Objectives
To compare the diagnostic accuracy of post-mortem magnetic resonance imaging (PMMR) specifically for non-cardiac thoracic pathology in fetuses and children, compared with conventional autopsy.
Methods
Institutional ethics approval and parental consent was obtained. A total of 400 unselected fetuses and children underwent PMMR before conventional autopsy, reported blinded to the other dataset.
Results
Of 400 non-cardiac thoracic abnormalities, 113 (28 %) were found at autopsy. Overall sensitivity and specificity (95 % confidence interval) of PMMR for any thoracic pathology was poor at 39.6 % (31.0, 48.9) and 85.5 % (80.7, 89.2) respectively, with positive predictive value (PPV) 53.7 % (42.9, 64.0) and negative predictive value (NPV) 77.0 % (71.8, 81.4). Overall agreement was 71.8 % (67.1, 76.2). PMMR was most sensitive at detecting anatomical abnormalities, including pleural effusions and lung or thoracic hypoplasia, but particularly poor at detecting infection.
Conclusions
PMMR currently has relatively poor diagnostic detection rates for the commonest intra-thoracic pathologies identified at autopsy in fetuses and children, including respiratory tract infection and diffuse alveolar haemorrhage. The reasonable NPV suggests that normal thoracic appearances at PMMR exclude the majority of important thoracic lesions at autopsy, and so could be useful in the context of minimally invasive autopsy for detecting non-cardiac thoracic abnormalities.
Key Points
• PMMR has relatively poor diagnostic detection rates for common intrathoracic pathology
• The moderate NPV suggests that normal PMMR appearances exclude most important abnormalities
• Lung sampling at autopsy remains the “gold standard” for pulmonary pathology
Similar content being viewed by others
Introduction
Paediatric and perinatal autopsy rates have declined over recent decades, leading to post-mortem cross-sectional imaging being proposed as a possible alternative or adjunctive approach [1, 2]. Post-mortem magnetic resonance imaging (PMMR), when used in conjunction with other ancillary investigations (collectively known as minimally invasive autopsy [MIA]), has recently been shown to have a high diagnostic accuracy rate for cause of death or main diagnosis compared with traditional autopsy in fetuses, stillbirths and children [3]. Whilst cardiac and neurological diagnoses account for the majority of causes of death in these age groups (12 and 28 % respectively [3]), less is known about how well thoracic pathology can be diagnosed across a range of likely diagnoses, gestational age and childhood age ranges.
A systematic review of post-mortem imaging [4] identified several previous studies [5–8] which had attempted to investigate the accuracy of non-cardiac thoracic diagnosis, and reported a relatively good estimated pooled sensitivity of 82 % (95 % confidence intervals 49, 95 %) and specificity of 86 % (58, 96 %) for lung pathology. However, these studies were not fully blinded between reporting radiologists and pathologists, included highly selected small cohort groups (range, 6–37 subjects), with pooled data from only 73 fetuses and no children, giving wide confidence intervals. Breeze et al. [9] independently reported a 2.5 % sensitivity and 87 % specificity for eight lung lesions in 30 fetuses, when assessed using PMMR, with a reported diagnostic accuracy of 83 %.
The aim of the MARIAS study was specifically to establish the diagnostic utility of less invasive autopsy, using PMMR, compared with traditional autopsy, in an unselected population for the major diagnosis or cause of death. These results have already been published [3]. Here, we use the detailed MARIAS dataset for sub-analysis of the PMMR findings specifically for non-cardiac thoracic abnormalities, irrespective of whether the abnormalities contributed to the main diagnosis or cause of death.
Materials and methods
Study participants
The study design has previously been described in detail [10]. Briefly, we performed pre-autopsy PMMR in an unselected sequential cohort of fetuses and children (up to 16 years), referred for conventional autopsy between March 2007 and September 2011, to Great Ormond Street Hospital for Children and University College Hospital, London. The study had institutional approval (reference 04/Q0508/41), and parental consent was obtained as stipulated by the ethics committee [3]. All fetuses and children (≤16 years) undergoing conventional autopsy were eligible for recruitment. PMMR was performed as soon as practically possible. Cases were excluded if consent was not available or if PMMR could not be performed before autopsy. The bodies were stored in a mortuary at 4 °C.
Imaging technique
Post-mortem magnetic resonance imagings (MRIs) were mostly scheduled to be done out of hours (6 pm to 8 am), causing least disturbance to clinical services. All examinations were performed on a 1.5-T MRI scanner (Avanto; Siemens Medical Solutions, Erlangen, Germany) with a conventional phased-array body coil, using whole-body three-dimensional (3D) T2-weighted turbo spin echo (TSE, TR 3,500 ms, TE 276 ms, voxel size 0.8 × 0.8 × 0.8 mm, 2 averages), 3D T1-weighted volumetric interpolated breath-hold examination (VIBE; TR 5.9 ms, TE 2.4 ms, flip angle 25°, voxel size 0.8 × 0.8 × 0.8 mm, 8 averages) and 3D constructive interference in the steady state (CISS) sequence (TR 9.2 ms, TE 4.6 ms, flip angle 70°, voxel size 0.6 × 0.6 × 0.6 mm, 4 averages), as published previously [10]. The first 20 cases (total 423) were used for MR sequence optimisation and for imager training.
Reporting PMMR images
PMMR images were reported by one of two specialist paediatric radiologists (O.O. and C.M.O.), with 12 and 18 years’ experience, using the OsiriX platform (OsiriX Foundation, Geneva, Switzerland). The radiologist was given the age and basic clinical details of the case, but was blinded to results of ancillary investigations and autopsy findings.
Reporting of autopsy data
Conventional autopsies were performed by one of several experienced specialist perinatal/paediatric pathologists (at least 8 years experience) in accordance with national guidelines, and were reported blinded to the MRI findings [3, 11].
Data and statistical analysis
Data were collected into a specific Microsoft Access database (version 2003; Microsoft, Redmond, WA, USA), which was developed as part of a study examining paediatric autopsies [12]. The radiologists and pathologists could only access their respective sections of the database until all data were reported. Prior to data unmasking, a pathologist (N.J.S.), radiologist (A.M.T.) and neonatologist (S.T.) reviewed all the PMMR and pathology reports, to define and categorise the findings according to predefined criteria [10]. The results presented here are those as recorded at the time of initial PMMR reporting, not following subsequent specialist unblinded review, so as to reflect how PMMR would be used in clinical practice.
In order to clarify the nature of the discrepancies, we then retrospectively reviewed the imaging and pathology findings. We excluded cardiac abnormalities, as they have been reported elsewhere [13] and divided specific thoracic diagnoses into one of seven categories, which were: respiratory tract infection (lung parenchymal consolidation at PMMR, pneumonia, pneumonitis and aspiration at autopsy), pulmonary haemorrhage, lung or thoracic hypoplasia/agenesis, pulmonary congestion/oedema, isolated pleural effusion, trachea-oesophageal fistula, and “other” categories.
Primary outcomes were sensitivity, specificity, positive-predictive valve (PPV) and negative predictive value (NPV), where PMMR (the index test) defined the diagnosis compared with conventional autopsy (the “gold standard”), with 95 % confidence intervals (CI). Concordance was defined as the sum of true positives and true negatives divided by all cases. Exact methods were used to calculate confidence intervals [14]. SPSS (version 19 for Macintosh; SPSS IBM, New York, USA) was used for data analysis. Sub-group analysis was performed based on age (fetuses <24 weeks gestation, fetuses ≥24 gestation, and children including all newborns, infants and children ≤16 years of age).
Results
Demographic data
PMMR was performed on 403 cases, although autopsy data could not be retrieved in 3 cases. Of the remaining 400 cases, 277/400 (69 %) were fetuses (consisting of 185 at ≤24 weeks’ gestation and 92 at >24 weeks’ gestation) and 123/400 (31 %) were children (consisting of 42 newborns aged <1 month, 53 infants >1 month to ≤12 months, 28 children >12 months to ≤16 years). Hospital-requested autopsies (fetal medicine unit or in-patients) accounted for 292 cases, with HM Coroner (Medical Examiner)-requested autopsies accounting for the remainder: 6 (2.2 %) fetuses and 102 (82.9 %) children. Mean (SD) time between death/delivery and PMMR was 4.5 (2.5) days.
Autopsy findings
Summary details of autopsy pathology in this dataset have been briefly reported previously [3]. Conventional autopsy studies revealed a total of 113/400 thoracic (28 %) abnormalities across all groups. At autopsy, in fetuses <24 weeks (n = 185), the thorax was normal in 146/185 (78.9 %) cases, abnormal in 35/185 (19 %) and non-diagnostic in 4/185 (2.1 %). Of the 113 abnormalities, the most common abnormalities reported were infection in 15/113 (13.3 %) and pulmonary hypoplasia in 11/113 (6 %) cases. In fetuses >24 weeks (n = 92), the thorax was abnormal in 16/92 (17 %), with infection being the commonest abnormality reported in 9/92 (10 %) cases. In newborns and children (n = 123), the thorax was abnormal in 62/123 (50.5 %) cases, with the commonest abnormalities being infection in 24/123 (19.5 %) and aspiration/haemorrhage in 12/123 (9.7 %) cases.
Non-diagnostic cases
There were 27/400 (6.7 %) non-diagnostic thoracic PMMR scans; all of which occurred in fetuses ≤24 weeks. There were two thoracic abnormalities (lung hypoplasia) in this group. Subsequent analysis of the data has been performed on the remaining 373 cases, which had 111/373 (29.8 %) thoracic abnormalities identified by conventional autopsy.
Comparison of PMMR to conventional autopsy
The overall sensitivity, specificity, PPV, NPV, and concordance across the three subgroups with 95 % confidence intervals are given in Table 1.
Thoracic PMMR had poor sensitivity and specificity across all groups, with slightly higher sensitivity in children than smaller fetuses (45 vs 30 %), but poorer specificity (61 vs 97 %), and poor overall concordance (71.8 %). Overall sensitivity was poor at 39.6 %, although specificity was higher at 85.5 %.
PMMR was most sensitive at detecting anatomical abnormalities, including pleural effusion (100 %) and lung or thoracic hypoplasia (60 %; Table 2). PMMR was particularly poor at detecting infection with sensitivity of 12.5 % and PPV of 25.0 %. Although overall concordance, specificity and NPV were high across different pathologies, this was largely due to the majority of normal cases in this study.
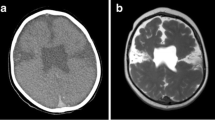
Examples of concordance between PMMR and conventional autopsy findings are shown in Figs. 1, 2, and 3; examples of a lack of concordance are shown in Figs. 4 and 5.
Example of false negative (miss) on PMMR. A miscarriage at 24 weeks due to presumed sepsis was initially reported as having normal lungs on PMMR but retrospective review reveals focal changes in the right lung (a). This was confirmed as ascending genital tract infection with congenital pneumonia at autopsy (b)
Fetuses <24 weeks
In fetuses <24 weeks, the thorax was abnormal in 33/158 cases (20.9 %). Ten correct positive thoracic diagnoses were made (10/33; sensitivity 30.3 %), of which there were six with lung or chest hypoplasia, one pleural effusion, two congenital diaphragmatic hernias and one hydrops (Table 3).
Twenty-three out of 33 (69.7 %) of diagnoses found at autopsy were not identified (apparent false negatives) on PMMR, including 15 infections, four lung hypoplasias, two trachea-oesophageal fistulae (ToFs), one abnormal lung lobation and one with absent nostrils as part of a complex facial malformation (Table 3). On unblinded review, 14 of the infection cases had normal unventilated post-mortem lung appearances; only one case had patchy lung changes, which could have been identified prospectively. The lungs looked normal in one case of hypoplasia, but were subjectively small in the other three cases, including one with associated renal dysplasia. There were five apparent false-positive diagnoses by PMMR: three lung hypoplasias and two pleural effusions (Table 3). One case of lung hypoplasia was in a case of skeletal dysplasia, but the other two were false-positives on unblinded review. Both pleural effusions were felt to be part of normal post-mortem changes at autopsy.
Fetuses >24 weeks
In fetuses >24 weeks, the thorax was abnormal in 16/92 cases (17.4 %). Six correct thoracic pathological diagnoses were made (6/16; sensitivity 37.5 %; Table 3). There were ten apparent false negatives (10/16; 62.5 %), including nine infections and one lung hypoplasia (Table 3). On unblinded review, the lungs had normal unventilated post mortem appearances in all nine infections. The lung hypoplasia was missed in a severely macerated 24-week-gestation fetus.
There were nine apparent false positives by PMMR: four pleural effusions, three lung hypoplasias and two focal lung lesions (Table 3). On unblinded review, all four pleural effusions were present but interpreted as normal post-mortem change at autopsy. In one of the lung hypoplasias, the lungs looked subjectively small on PMMR in a case of massive sacrococcygeal teratoma, but were histologically normal size and weight at autopsy. Two other lung hypoplasias were overcalls. In one “lung lesion”, the lungs looked patchy on PMMR but were normal at autopsy, including histological examination, and in the other the lungs looked normal on PMMR but were distorted by large amounts of intra-pleural gas.
Newborns and children
In newborns, infants and children, the thorax was abnormal in 62/123 cases (50.4 %). Twenty-eight correct pathological diagnoses were made (28/62; sensitivity 45.2 %; Table 3). Thirty-four thoracic diagnoses were not correctly identified (34/62; 54.8 %), including 18 infections, 8 with pulmonary haemorrhage, 2 trachea-oesophageal fistulae, 3 pulmonary congestion/oedema and 1 case each of lung hypoplasia, pulmonary hypertension and hyaline membrane disease (Table 3). On unblinded review, there were patchy lung changes, which could have been interpreted as abnormal in only six of the cases in which infection was diagnosed at autopsy; in the other 12 cases, the lungs looked normal on PMMR. Equally, there were patchy lung changes in five of the cases of pulmonary haemorrhage and two cases of pulmonary congestion and oedema, but the lungs looked normal in the other three and one case respectively. The lungs looked normal on PMMR in the cases of HMD, pulmonary hypertension and hypoplasia. The trachea-oesophageal fistulae were not identified.
There were 24 apparent false positives, including 18 infections, 2 lung hypoplasias, 2 focal lung lesions, 1 pleural effusion and 1 dilated oesophagus (Table 3). On unblinded review, there were patchy lung changes in 17 out of 18 cases of infection, and both cases of focal lung lesions, although none of these could be confirmed as abnormal at autopsy, including histology. In one case of lung hypoplasia the child had a skeletal dysplasia (osteogenesis imperfecta type IIa) with a small, dysmorphic ribcage, although the lungs were histologically normal and of normal weight at autopsy, but the other was an overcall. The case of pleural effusion was interpreted as normal post-mortem change at autopsy. The oesophagus was dilated in one case on PMMR but no abnormality was detected at autopsy.
Across all groups, the commonest abnormality was infection (consolidation on PMMR, pneumonia or pneumonitis at autopsy), accounting for 43 % of all diagnoses made, although only six correct diagnoses were made on PMMR, with 42 apparent false negatives and 18 false positives made. This gives a sensitivity of 12.5 % (5.9, 24.7) and specificity of 92.6 % (88.6, 95.2), and concordance of 79.3 % (74.3, 83.6) for infection alone (Table 2).
Discussion
In this large prospective study, PMMR demonstrated poor diagnostic utility for detection of thoracic pathology in fetuses, newborns and children. Whilst the specificity was high at 86 %, due to the large number of normal cases, the sensitivity and positive predictive value were poor at 40 and 54 % respectively. Overall diagnostic accuracy was reasonable at 72 %. PMMR was most sensitive at detecting anatomical abnormalities such as lung or chest hypoplasia and post-mortem pleural effusions, but poor at detecting infection and pulmonary haemorrhage.
PMMR showed a 9.5 % apparent false-positive rate for thoracic imaging, which is in keeping with results from other body systems [3]. Apparent false positives do not necessarily represent a significant failure of the minimally invasive autopsy model, since the vast majority (75 %) were overcalls of possible infection (consolidation/pneumonia) in children, which would lead to additional investigations and organ sampling for histopathological confirmation. There were several false positives where normal post-mortem accumulation of fluid in bodily cavities was identified but mis-interpreted as pathological pleural fluid, and most of the correct interpretations of lung hypoplasia were recorded in the context of skeletal dysplasia.
Our accuracy data in this large unselected population is lower than those previously published [5–8], with lower sensitivity and overall concordance, but similar specificity. This is likely to be due to the difficulty in diagnosing infection, particularly in children, where such cases were not included in the several previous studies. Breeze et al. [9] reported a reported a 62.5 % sensitivity (95 % CI = 29.0, 96.0) and 87 % specificity (95 % CI = 78.9, 100), for eight lung lesions over 30 fetuses. Our findings are similar, in that fetal lung hypoplasia was usually easily detected, but was also overcalled. Their series only had two false-positive lung diagnoses (2/30 = 6.7 %), and their PPV was 71.4 % (35.9, 91.8), NPV 87.0 % (67.9, 95.5), and overall concordance 83 % (66.4, 92.7 %), all greater than our data but with much wider confidence intervals. We postulate that lung PMMR is more difficult across a larger cohort of children when reported in a blinded fashion.
Infection (pneumonia or lung parenchymal consolidation) was by far both the commonest abnormality in our study, and also the most difficult to achieve correctly. There are several diagnostic difficulties highlighted by our study, and a small study of 44 children has previously identified similar difficulties in detecting lung parenchymal changes using whole-body post-mortem CT [15]. In unventilated fetal lungs, infection was missed in the majority of cases, and infection was equally overcalled and missed in the paediatric population, with or without patchy signal changes in the lungs at post-mortem. We conclude that infection or pneumonia is currently difficult to identify at fetal PMMR, and that lung sampling should be performed in all cases where sepsis is suspected or possible. In older children, misinterpreting consolidation as normal post-mortem change, and vice versa, represents a real challenge in PMMR, recognised by other authors [16]. Several features within the lungs may be interpreted as consolidation (as they would indicate such in life), whereas at autopsy the unequally distributed fluid accumulation within the lung parenchyma is a variant of normal post-mortem changes. We also failed to diagnose eight out of 12 cases of pulmonary haemorrhage, which were interpreted as ‘normal’ post-mortem changes. However, there are variable histological degrees of pulmonary congestion and intra-alveolar fluid in the majority of cases of infant death, regardless of cause. The high apparent false-negative rate (16.2 %; apparent pathologies present at autopsy which were not reported on PMMR) in this study also mainly relates to patchy but diffuse lung parenchymal change, i.e. pneumonia or haemorrhage. The majority of thoracic misses and overcalls in this study were in newborns and children, and mostly related to both overcalling and missing pneumonia.
A normal thoracic scan in fetuses predicts normal pathology in over 80 % of cases, probably because lung aeration does not present a confounding problem in differentiating between other causes of death, such as CDH or pulmonary hypoplasia, but this does not hold true for children. Our current practice is that unless a focal lung lesion is identified on PMMR, then standard lung histopathology should be performed in all childhood cases. It may be possible that in future this could be performed by percutaneous or endoscopic routes [17], but the accuracy of this approach to detect patchy lung pathology, compared with open sampling, remains undetermined.
Lung abnormalities are notoriously difficult to detect using other types of post-mortem imaging. For instance, lung opacities on post-mortem radiographs have little correlation with histologically diagnostic pneumonia [18]. Lung PMMR is unlikely to have higher diagnostic accuracy than thoracic MRI in life, and high-resolution computed tomography (CT) remains the mainstay of diagnostic imaging for parenchymal changes, including interstitial lung disease and more subtle pathology. Whilst infant and childhood lung MRI is improving, it is notoriously sequence-dependent and prone to respiratory and cardiac motion artefacts [19]. The post-mortem state negates several of these issues, but clearly brings new diagnostic challenges.
The main strength of this study is the double-blinded study design and large prospective data collection of unselected cases, which allows categorical reporting of both conventional autopsy and PMMR data, in an independent way. By identifying small pleural effusions, and lung parenchymal changes more accurately, it is likely that correct interpretation of PMMR images will be easier in the future.
A limitation of this study was that these cases were all interpreted by both specialist paediatric radiologists in a tertiary centre and, as such, is unlikely to represent the situation in many other centres. It also highlights both the difficulty in interpreting cases correctly, as these are predominantly interpretation rather than observational errors, and therefore emphasises the need for specialist education in this field in order to maximise the diagnostic yield from both imaging and autopsy. We did not perform post-mortem CT in our cohort, the diagnostic accuracy of which in this setting remains to be evaluated. We also did not measure temperature during PMMR in this study, which may have had an impact on the reporting radiologists’ ability to correctly interpret PMMR images [20]. We also did not evaluate more advanced MR techniques, such as T2 relaxometry of the lungs or diffusion-weighted imaging. Semi-quantitative measures of water redistribution may be able to differentiate pathological from non-pathological changes in the lungs, but such approaches require further investigation.
PMMR currently has relatively poor diagnostic detection rates for the commonest intra-thoracic pathologies identified at autopsy in fetuses and children, including infection and haemorrhage. The relatively high negative predictive value suggests that normal thoracic appearances at PMMR excludes the majority of important thoracic lesions at autopsy, and so could be useful in the context of minimally invasive autopsy for excluding non-cardiac thoracic abnormalities.
References
Shojania KG, Burton EC (2008) The vanishing nonforensic autopsy. N Engl J Med 358:873–875
Sieswerda-Hoogendoorn T, van Rijn RR (2010) Current techniques in postmortem imaging with specific attention to paediatric applications. Pediatr Radiol 40:141–152
Thayyil S, Sebire NJ, Chitty LS, Wade A, Chong WK, MARIAS Collaborative Group et al (2013) Post-mortem MRI versus conventional autopsy in fetuses and children: a prospective validation study. Lancet 382:223–333
Thayyil S, Chandrasekaran M, Chitty LS, Wade A, Skordis-Worrall J, Bennett-Britton I, Cohen M, Withby E, Sebire NJ, Robertson NJ, Taylor AM (2010) Diagnostic accuracy of post-mortem magnetic resonance imaging in fetuses, children and adults: a systematic review. Eur J Radiol 75:e142–e148
Huisman TA, Wisser J, Stallmach T, Krestin GP, Huch R, Kubik-Huch RAC (2002) MR autopsy in fetuses. Fetal Diagn Ther 17:58–64
Alderliesten ME, Peringa J, van der Hulst VP, Blaauwgeers HL, van Lith JMC (2003) Perinatal mortality: clinical value of postmortem magnetic resonance imaging compared with autopsy in routine obstetric practice. BJOG 110:378–382
Roberts IS, Benbow EW, Bisset R et al (2003) Accuracy of magnetic resonance imaging in determining cause of sudden death in adults: comparison with conventional autopsy. Histopathology 42:424–430
Patriquin L, Kassarjian A, Barish M et al (2001) Postmortem whole-body magnetic resonance imaging as an adjunct to autopsy: preliminary clinical experience. J Magn Reson Imaging 13:277–287
Breeze AC, Cross JJ, Hackett GA, Jessop FA, Joubert I, Lomas DJ, Set PA, Whitehead AL, Lees CC (2006) Use of a confidence scale in reporting postmortem fetal magnetic resonance imaging. Ultrasound Obstet Gynecol 28:918–924
Thayyil S, Sebire NJ, Chitty LS, Wade A, Olsen O, Gunny RS, Offiah A, Saunders DE, Owens CM, Chong WK, Robertson NJ, Taylor AM (2011) Post mortem magnetic resonance imaging in the fetus, infant and child: a comparative study with conventional autopsy (MARIAS protocol). BMC Pediatr 11:120
Royal College of Pathologists Working Party on the Autopsy (2006) Guidelines on Autopsy Practice: Scenario 9: Stillborn infant (singleton). June 2006. http://www.rcpath.org/Resources/RCPath/Migrated%20Resources/Documents/G/G001Autopsy-Stillbirths-Jun06.pdf. Accessed 01 Nov 2013
Weber MA, Klein NJ, Hartley JC, Lock PE, Malone M, Sebire NJ (2008) Infection and sudden unexpected death in infancy: a systematic retrospective case review. Lancet 371:1848–1853
Taylor AM, Sebire NJ, Ashworth MT, Schievano S, Scott RS, Chitty LS, Robertson N, Thayyil S, Magnetic Resonance Imaging Autopsy Study Collaborative Group et al (2014) Post-mortem cardiovascular magnetic resonance imaging in fetuses and children—a masked comparison study with conventional autopsy. Circulation 129:1937–1944
Wilson EB (1927) Probable inference, the law of succession, and statistical inference. J Am Stat Assoc 22:209–212
Proisy M, Marchand AJ, Loget P, Bouvet R, Roussey M, Pelé F, Rozel C, Treguier C, Darnault P, Bruneau B (2013) Whole-body post-mortem computed tomography compared with autopsy in the investigation of unexpected death in infants and children. Eur Radiol 23:1711–1719
Germerott T, Preiss US, Ebert LC, Ruder TD, Ross S, Flach PM, Ampanozi G, Filograna L, Thali MJ (2010) A new approach in virtopsy: postmortem ventilation in multislice computed tomography. Legal Med (Tokyo) 12:276–279
Sebire NJ, Weber MA, Thayyil S, Mushtaq I, Taylor A, Chitty LS (2012) Minimally invasive perinatal autopsies using magnetic resonance imaging and endoscopic postmortem examination (“keyhole autopsy”): feasibility and initial experience. J Matern Fetal Neonatal Med 25:513–518
Olsen OE (2006) Radiography following perinatal death: a review. Acta Radiol 47:91–99
Hirsch W, Sorge I, Krohmer S, Weber D, Meier K, Till H (2008) MRI of the lungs in children. Eur J Radiol 68:278–288
Ruder TD, Hatch GM, Siegenthaler L, Ampanozi G, Mathier S, Thali MJ, Weber OM (2012) The influence of body temperature on image contrast in post mortem MRI. Eur J Radiol 81:1366–1370
Acknowledgments
The scientific guarantor of this publication is Andrew M. Taylor. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. This study has received funding by the Policy Research Programme in the Department of Health (0550004). The views expressed are not necessarily those of the Department. The study was also supported by grants from the British Heart Foundation (CI/05/010). The MR facility at the UCL Centre for Cardiovascular Imaging was funded by the British Heart Foundation (CI/05/010). None of the funding bodies had any role in analysis of data, results or conclusions of the study. A.M.T. is supported by an NIHR Senior Research fellow award, NJS is supported by an NIHR Senior Investigator award, and O.A. and S.T. are supported by NIHR Clinician Scientist awards. L.S.C., N.J.S. and A.M.T. receive funding from the Great Ormond Street Hospital Children’s Charity. This work was undertaken at GOSH/ICH, UCLH/UCL including support from the NIHR GOSH Biomedical Research Centre. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study.
Some study subjects or cohorts have been previously reported by Thayyil et al. [3]. Methodology: prospective, diagnostic study, multicentre study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
MaRIAS (Magnetic Resonance Imaging Autopsy Study) Collaborative group
Ms. Shea Addison (Research Assistant, UCL), Dr. Michael Ashworth (Consultant in Paediatric Pathology, GOSH) Dr. Alan Bainbridge (MR Physicist, UCL), Dr. Jocelyn Brookes (Consultant in Interventional Radiology, UCH), Prof. Lyn Chitty (Consultant in Fetal Medicine and Genetics, UCL), Dr. WK ‘Kling’ Chong (Consultant in Paediatric Neuroradiology, GOSH), Dr. Andrew Cook (Senior Lecturer in Cardiac Morphology, UCL), Dr. Enrico de Vita (MR Physicist, UCL), Dr. Roxana Gunny (Consultant in Paediatric Neuroradiology, GOSH), Dr. Brian Harding (Consultant in Paediatric Neuropathology, GOSH), Dr. Tom Jacques (Consultant in Paediatric Neuropathology, GOSH), Mr. Rod Jones (Research MR radiographer, UCL), Dr. Mark Lythgoe (Director, Centre for Advanced Biomedical Imaging, UCL), Dr. Marion Malone (Consultant in Paediatric pathology, GOSH), Wendy Norman (Research MR radiographer, UCL), Dr. Oystein Olsen (Consultant in Paediatric Chest and Abdomen Imaging, GOSH), Dr. Cathy Owens (Consultant in Paediatric Chest and Abdomen Imaging, GOSH), Dr. Amaka C. Offiah (Consultant in Paediatric Musculoskeletal Imaging, previously GOSH, currently Sheffield Children’s Hospital), Dr. Nikki Robertson (Reader and Consultant in Neonatology, UCH), Dr. Tony Risdon (Consultant in Paediatric Forensic Pathology, GOSH), Prof. Neil Sebire (Professor of Perinatal and Paediatric Developmental Pathology, GOSH), Dr. Rosemary Scott (Consultant in Perinatal pathology, UCH), Dr. Dawn Saunders (Consultant in Paediatric Neuroradiology, GOSH), Dr. Silvia Schievano (Senior Research Fellow in Medical Engineering, UCL), Ms. Angie Scales (Family liaison sister, GOSH), Prof. Andrew Taylor (Chief Investigator; Professor of Cardiovascular Imaging, UCL), Sudhin Thayyil (Senior Clinical Lecturer and Honorary Consultant in Neonatology, UCL), Angie Wade (Senior Lecturer in Medical Statistics, UCL).
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Arthurs, O.J., Thayyil, S., Olsen, O.E. et al. Diagnostic accuracy of post-mortem MRI for thoracic abnormalities in fetuses and children. Eur Radiol 24, 2876–2884 (2014). https://doi.org/10.1007/s00330-014-3313-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3313-8








