Abstract
Purpose
To evaluate a self-test for Dutch breast screening radiologists introduced as part of the national quality assurance programme.
Methods and materials
A total of 144 radiologists were invited to complete a test-set of 60 screening mammograms (20 malignancies). Participants assigned findings such as location, lesion type and BI-RADS. We determined areas under the receiver operating characteristics (ROC) curves (AUC), case and lesion sensitivity and specificity, agreement (kappa) and correlation between reader characteristics and case sensitivity (Spearman correlation coefficients).
Results
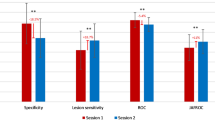
A total of 110 radiologists completed the test (76 %). Participants read a median number of 10,000 screening mammograms/year. Median AUC value was 0.93, case and lesion sensitivity was 91 % and case specificity 94 %. We found substantial agreement for recall (κ = 0.77) and laterality (κ = 0.80), moderate agreement for lesion type (κ = 0.57) and BI-RADS (κ = 0.45) and no correlation between case sensitivity and reader characteristics.
Conclusion
Areas under the ROC curve, case sensitivity and lesion sensitivity were satisfactory and recall agreement was substantial. However, agreement in lesion type and BI-RADS could be improved; further education might be aimed at reducing interobserver variation in interpretation and description of abnormalities. We offered individual feedback on interpretive performance and overall feedback at group level. Future research will determine whether performance has improved.
Key Points
• We introduced and evaluated a self-test for Dutch breast screening radiologists.
• ROC curves, case and lesion sensitivity and recall agreement were all satisfactory.
• Agreement in BI-RADS interpretation and description of abnormalities could be improved.
• These are areas that should be targeted with further education and training.
• We offered individual feedback on interpretative performance and overall group feedback.





Similar content being viewed by others
References
Holland R, Rijken HJ, Hendriks JH (2007) The Dutch population-based mammography screening: 30-years experience. Breast Care 2:12–18
National Evaluation Team for Breast Cancer Screening (2012) Preliminary results breast cancer screening programme in the Netherlands, 2011. NETCB, Rotterdam
Australian Government Department of Health and Aging (2009) BreastScreen Australia Evaluation: evaluation final report. Department of Health and Aging, Canberra
The Royal College of Radiologists (2007) Standards for self-assessment of performance. RCR, London
United States Food and Drug Administration (2012) Mammography quality standards act and program 2012. http://www.fda.gov/radiationemitting-products/mammographyqualitystandardsactandprogram/default.htm. Accessed 21 Nov 2012
Soh BP, Lee W, Kench PL et al (2012) Assessing reader performance in radiology, an imperfect science: lessons from breast screening. Clin Radiol 67:623–628
Scott HJ, Gale A (2006) Breast screening: PERFORMS identifies key mammographic training needs. Br J Radiol 79:S127–S133
Cook AJ, Elmore JG, Zhu W et al (2012) Mammographic interpretation: radiologists' ability to accurately estimate their performance and compare it with that of their peers. AJR Am J Roentgenol 199:695–702
Geller BM, Ichikawa L, Miglioretti DL, Eastman D (2012) Web-based mammography audit feedback. AJR Am J Roentgenol 198:562–567
Shapiro S, Coleman EA, Broeders M et al (1998) Breast cancer screening programmes in 22 countries: current policies, administration and guidelines. International Breast Cancer Screening Network (IBSN) and the European Network of Pilot Projects for Breast Cancer Screening. Int J Epidemiol 27:735–742
Yankaskas BC, Klabunde CN, Ancelle-Park R et al (2004) International comparison of performance measures for screening mammography: can it be done? J Med Screen 11:187–193
Timmers JM, van Doorne-Nagtegaal HJ, Zonderland HM et al (2012) The Breast Imaging Reporting and Data System (BI-RADS) in the Dutch breast cancer screening programme: its role as an assessment and stratification tool. Eur Radiol 22:5
Eng J (2012) ROC analysis: web-based calculater for ROC curves. http://www.jrocfit.org. Accessed 21 Nov 2012
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46
Ciatto S, Ambrogetti D, Morrone D, Del Turco M (2006) Analysis of the results of a proficiency test in screening mammography at the CSPO of Florence: review of 705 tests. Radiol Med 111:797–803
Onega T, Smith M, Miglioretti DL et al (2012) Radiologist agreement for mammographic recall by case difficulty and finding type. J Am Coll Radiol 9:788–794
Reed WM, Lee WB, Cawson JN, Brennan PC (2010) Malignancy detection in digital mammograms: important reader characteristics and required case numbers. Acad Radiol 17:1409–1413
Esserman L, Cowley H, Eberle C et al (2002) Improving the accuracy of mammography: volume and outcome relationships. J Natl Cancer Inst 94(5):369–375
Miglioretti DL, Gard CC, Carney PA et al (2009) When radiologists perform best: the learning curve in screening mammogram interpretation. Radiology 253:632–640
Pusic MV, Andrews JS, Kessler DO et al (2012) Prevalence of abnormal cases in an image bank affects the learning of radiograph interpretation. Med Educ 46:289–298
Carney PA, Bogart TA, Geller BM et al (2012) Association between time spent interpreting, level of confidence, and accuracy of screening mammography. Am J Roentgenol 198:970–978
Elmore JG, Jackson SL, Abraham L et al (2009) Variability in interpretive performance at screening mammography and radiologists' characteristics associated with accuracy. Radiology 253:641–651
Kerlikowske K, Grady D, Barclay J et al (1998) Variability and accuracy in mammographic interpretation using the American College of Radiology Breast Imaging Reporting and Data System. J Natl Cancer Inst 90:1801–1809
Lazarus E, Mainiero MB, Schepps B et al (2006) BI-RADS lexicon for US and mammography: interobserver variability and positive predictive value. Radiology 239:385–391
Pinto A, Acampora C, Pinto F et al (2011) Learning from diagnostic errors: a good way to improve education in radiology. Eur J Radiol 78:372–376
Gur D, Bandos AI, Cohen CS et al (2008) The "laboratory" effect: comparing radiologists' performance and variability during prospective clinical and laboratory mammography interpretations. Radiology 249:47–53
Acknowledgements
The authors especially would like to acknowledge the careful work of Paul van de Looi in organising and developing the test set. We also thank the expert panel for their time in composing the test set and the participating radiologists for providing the data for this work
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Timmers, J.M.H., Verbeek, A.L.M., Pijnappel, R.M. et al. Experiences with a self-test for Dutch breast screening radiologists: lessons learnt. Eur Radiol 24, 294–304 (2014). https://doi.org/10.1007/s00330-013-3018-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-013-3018-4