Abstract
Objective
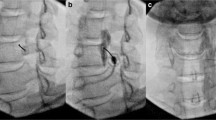
To describe and evaluate the feasibility and efficacy of CT-guided radiofrequency neurolysis (RFN) vs. local blockade of the stellate ganglion in the management of chronic refractory type I complex regional pain syndrome (CRPS) of the upper limb.
Methods
Sixty-seven patients were included in this retrospective study between 2000 and 2011. All suffered from chronic upper limb type I CRPS refractory to conventional pain therapies. Thirty-three patients underwent stellate ganglion blockade and 34 benefited from radiofrequency neurolysis of the stellate ganglion. CT guidance was used in both groups. The procedure was considered effective when pain relief was ≥50 %, lasting for at least 2 years.
Results
Thirty-nine women (58.2 %) and 28 men (41.8 %) with a mean age of 49.5 years were included in the study. Univariate analysis performed on the blockade and RFN groups showed a significantly (P < 0.0001) higher success rate in the RFN group (67.6 %, 23/34) compared with the blockade group (21.2 %, 7/33) with an odds ratio of 7.76.
Conclusion
CT-guided radiofrequency neurolysis of the stellate ganglion is a safe and successful treatment of chronic refractory type I CRPS of the upper limb. It appears to be more effective than stellate ganglion blockade.
Key Points
• Complex regional pain syndrome is painful, disabling and often refractory to treatment.
• Sixty-seven percent of patients had lasting pain relief (2 years) after radiofrequency neurolysis.
• Retrospective study showed a significantly higher success rate for radiofrequency neurolysis.
• CT guidance is mandatory for a successful and safe procedure.




Similar content being viewed by others
References
Roberts WJ (1986) A hypothesis on the physiological basis for causalgia and related pains. Pain 24:297–311
Quisel A, Gill JM, Witherell P (2005) Complex regional pain syndrome: which treatments show promise? J Fam Pract 54:599–603
Cepeda MS, Carr DB, Lau J (2005) Local anesthetic sympathetic blockade for complex regional pain syndrome. Cochrane Database Syst Rev (4):CD004598
Yucel I, Demiraran Y, Ozturan K, Degirmenci E (2009) Complex regional pain syndrome type I: efficacy of stellate ganglion blockade. J Orthop Traumatol 10:179–183
Nascimento MS, Klamt JG, Prado WA (2010) Intravenous regional block is similar to sympathetic ganglion block for pain management in patients with complex regional pain syndrome type I. Braz J Med Biol Res 43:1239–1244
Kastler A, Aubry S, Barbier-Brion B, Jehl J, Kastler B (2012) Radiofrequency neurolysis in the management of inguinal neuralgia: preliminary study. Radiology 262:701–707
Chua NH, Vissers KC, Sluijter ME (2011) Pulsed radiofrequency treatment in interventional pain management: mechanisms and potential indications-a review. Acta Neurochir (Wien) 153:763–771
Ellis H, Feldman S (1979) Anatomy for the anaesthtists, 3rd edn. Blackwell Scientific Publications, Oxford
Hogan QH, Erickson SJ (1992) MR imaging of the stellate ganglion: normal appearance. AJR Am J Roentgenol 158:655–659
Merskey HBN (1994) Classification of chronic pain. IASP Press
Collins SL, Moore RA, McQuay HJ (1997) The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain 72:95–97
Kastler B (2006) Interventional radiology in pain treatment. Springer, Berlin
Wang JK, Johnson KA, Ilstrup DM (1985) Sympathetic blocks for reflex sympathetic dystrophy. Pain 23:13–17
Ackerman WE, Zhang JM (2006) Efficacy of stellate ganglion blockade for the management of type 1 complex regional pain syndrome. South Med J 99:1084–1088
Schurmann M, Gradl G, Wizgal I et al (2001) Clinical and physiologic evaluation of stellate ganglion blockade for complex regional pain syndrome type I. Clin J Pain 17:94–100
Albazaz R, Wong YT, Homer-Vanniasinkam S (2008) Complex regional pain syndrome: a review. Ann Vasc Surg 22:297–306
Hogan QH, Abram SE (1997) Neural blockade for diagnosis and prognosis. A review. Anesthesiology 86:216–241
Higa K, Hirata K, Hirota K, Nitahara K, Shono S (2006) Retropharyngeal hematoma after stellate ganglion block: Analysis of 27 patients reported in the literature. Anesthesiology 105:1238–1245, discussion 1235A–1236A
Chaturvedi A, Dash H (2010) Locked-in syndrome during stellate ganglion block. Indian J Anaesth 54:324–326
Carron H, Litwiller R (1975) Stellate ganglion block. Anesth Analg 54:567–570
Allen G, Samson B (1986) Contralateral Horner’s syndrome following stellate ganglion block. Can Anaesth Soc J 33:112–113
Abdi S, Zhou Y, Patel N, Saini B, Nelson J (2004) A new and easy technique to block the stellate ganglion. Pain Physician 7:327–331
Elias M (2000) Cervical sympathetic and stellate ganglion blocks. Pain Physician 3:294–304
Moore DC, Bridenbaugh LD Jr (1956) The anterior approach to the stellate ganglion use without a serious complication in two thousand blocks. J Am Med Assoc 160:158–162
Hogan QH, Erickson SJ, Haddox JD, Abram SE (1992) The spread of solutions during stellate ganglion block. Reg Anesth 17:78–83
Guntamukkala M, Hardy PA (1991) Spread of injectate after stellate ganglion block in man: an anatomical study. Br J Anaesth 66:643–644
Bogduk N, Macintosh J, Marsland A (1987) Technical limitations to the efficacy of radiofrequency neurotomy for spinal pain. Neurosurgery 20:529–535
Cosman ER, Rittman WJ, Nashold BS, Makachinas TT (1988) Radiofrequency lesion generation and its effect on tissue impedance. Appl Neurophysiol 51:230–242
Forouzanfar T, van Kleef M, Weber WE (2000) Radiofrequency lesions of the stellate ganglion in chronic pain syndromes: retrospective analysis of clinical efficacy in 86 patients. Clin J Pain 16:164–168
Geurts J, Stolker R (1993) Percutaneous radiofrequency lesion of the stellate ganglion in the treatment of pain in upper extremity reflex sympathetic dystrophy. Pain Clin 6:17–25
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kastler, A., Aubry, S., Sailley, N. et al. CT-guided stellate ganglion blockade vs. radiofrequency neurolysis in the management of refractory type I complex regional pain syndrome of the upper limb. Eur Radiol 23, 1316–1322 (2013). https://doi.org/10.1007/s00330-012-2704-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-012-2704-y