Abstract
Objectives
To quantitatively evaluate regional lymph nodes in rectal cancer patients by using an automated, computer-aided approach, and to assess the accuracy of this approach in differentiating benign and malignant lymph nodes.
Methods
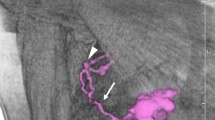
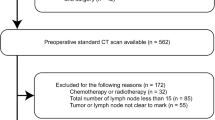
Patients (228) with newly diagnosed rectal cancer, confirmed by biopsy, underwent enhanced computed tomography (CT). Patients were assigned to the benign node or malignant node group according to histopathological analysis of node samples. All CT-detected lymph nodes were segmented using the edge detection method, and seven quantitative parameters of each node were measured. To increase the prediction accuracy, a hierarchical model combining the merits of the support and relevance vector machines was proposed to achieve higher performance.
Results
Of the 220 lymph nodes evaluated, 125 were positive and 95 were negative for metastases. Fractal dimension obtained by the Minkowski box-counting approach was higher in malignant nodes than in benign nodes, and there was a significant difference in heterogeneity between metastatic and non-metastatic lymph nodes. The overall performance of the proposed model is shown to have accuracy as high as 88% using morphological characterisation of lymph nodes.
Conclusions
Computer-aided quantitative analysis can improve the prediction of node status in rectal cancer.




Similar content being viewed by others
References
Kim YS, Kim JH, Yoon SM, Choi EK, Ahn SD, Lee SW, Kim JC, Yu CS, Kim HC, Kim TW, Chang HM (2009) Lymph node ratio as a prognostic factor in patients with stage III rectal cancer treated with total mesorectal excision followed by chemoradiotherapy. Int J Radiat Oncol Biol Phys 74:796–802
Moug SJ, Saldanha JD, McGregor JR, Balsitis M, Diament RH (2009) Positive lymph node retrieval ratio optimises patient staging in colorectal cancer. Br J Cancer 100:1530–1533
Peschaud F, Benoist S, Julié C, Beauchet A, Penna C, Rougier P, Nordlinger B (2008) The ratio of metastatic to examined lymph nodes is a powerful independent prognostic factor in rectal cancer. Ann Surg 248:1067–1073
Zerhouni EA, Rutter C, Hamilton SR, Balfe DM, Megibow AJ, Francis IR, Moss AA, Heiken JP, Tempany CM, Aisen AM, Weinreb JC, Gatsonis C, McNeil BJ (1996) CT and MR imaging in the staging of colorectal carcinoma: report of the Radiology Diagnostic Oncology Group II. Radiology 200:443–451
Kim NK, Kim MJ, Yun SH, Sohn SK, Min JS (1999) Comparative study of transrectal ultrasonography, pelvic computerized tomography, and magnetic resonance imaging in preoperative staging of rectal cancer. Dis Colon Rectum 42:770–775
Lahaye MJ, Engelen SM, Nelemans PJ, Beets GL, van de Velde CJ, van Engelshoven JM, Beets-Tan RG (2005) Imaging for predicting the risk factors–the circumferential resection margin and nodal disease–of local recurrence in rectal cancer: a meta-analysis. Semin Ultrasound CT MR 26:259–268
Maier A, Fuchsjäger M (2003) Preoperative staging of rectal cancer. Eur J Radiol 47:89–97
Kim CK, Kim SH, Chun HK, Lee WY, Yun SH, Song SY, Choi D, Lim HK, Kim MJ, Lee J, Lee SJ (2006) Preoperative staging of rectal cancer: accuracy of 3-Tesla magnetic resonance imaging. Eur Radiol 16:972–980
Kim SH, Lee JM, Lee MW, Kim GH, Han JK, Choi BI (2008) Diagnostic accuracy of 3.0-Tesla rectal magnetic resonance imaging in preoperative local staging of primary rectal cancer. Invest Radiol 43:587–593
Koh DM, Chau I, Tait D, Wotherspoon A, Cunningham D, Brown G (2008) Evaluating mesorectal lymph nodes in rectal cancer before and after neoadjuvant chemoradiation using thin-section T2-weighted magnetic resonance imaging. Int J Radiat Oncol Biol Phys 71:456–461
Lahaye MJ, Beets GL, Engelen SM, Kessels AG, de Bruïne AP, Kwee HW, van Engelshoven JM, van de Velde CJ, Beets-Tan RG (2009) Locally advanced rectal cancer: MR imaging for restaging after neoadjuvant radiation therapy with concomitant chemotherapy. Part II. What are the criteria to predict involved lymph nodes? Radiology 252:81–91
Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG, Dallimore NS, Williams GT (2003) Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology 227:371–377
Kim JH, Beets GL, Kim MJ, Kessels AG, Beets-Tan RG (2004) High-resolution MR imaging for nodal staging in rectal cancer: are there any criteria in addition to the size? Eur J Radiol 52:78–83
Vapnik VN (1998) Statistical learning theory. Wiley-Interscience, New York
Zheng Y, Yang X, Beddoe G (2007) Reduction of false positives in polyp detection using weighted support vector machines. Conf Proc IEEE Eng Med Biol Soc 4433–4439
Axelberg PGV, Gu IY-H, Bollen MH (2007) Support vector machine for classification of voltage disturbances. IEEE Trans Power Delivery 22:1297–1303
Cawley GC, Talbot NLC (2003) Efficient leave-one-out cross-validation of kernel fisher discriminant classifiers. Pattern Recognition 36:2585–2592
An SJ, Liu WQ, Venkatesh S (2006) Efficient cross-validation of the complete two stages in KFD classifier Formulation. 18th Int Conference. Pattern Recognition 3:240–244
Koh DM, Brown G, Temple L, Blake H, Raja A, Toomey P, Bett N, Farhat S, Norman AR, Daniels I, Husband JE (2005) Distribution of mesorectal lymph nodes in rectal cancer: in vivo MR imaging compared with histopathological examination. Initial observations. Eur Radiol 15:1650–1657
Lahaye MJ, Engelen SM, Kessels AG, de Bruïne AP, von Meyenfeldt MF, van Engelshoven JM, van de Velde CJ, Beets GL, Beets-Tan RG (2008) USPIO-enhanced MR imaging for nodal staging in patients with primary rectal cancer: predictive criteria. Radiology 246:804–811
Koh DM, Brown G, Temple L, Raja A, Toomey P, Bett N, Norman AR, Husband JE (2004) Rectal cancer: mesorectal lymph nodes at MR imaging with USPIO versus histopathologic findings - initial observations. Radiology 231:91–99
Acknowledgement
Supported by grants 80171207 and 60902076 from the National Nature Science Foundation of China; grant 10ykjcll from the Fundamental Research Funds for the Central Universities; grant 2010 J-E151 from Guangzhou Technology Support Program; and grant 2010A030500004 from Science and Technology Planning Project of Guangdong Province
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
This appendix has been provided by the authors to give readers additional information about their work.
Quantitative measurements of lymph nodes
To achieve comprehensive characterization of a lymph node, 19 parameters were computed automatically based on segmented image. Among which seven were chosen to consist of a compact but highly representative subset. The detailed definitions of the parameters are listed below:
-
Area: the area of the node;
-
Major axis length & minor axis length: the major & minor axis of the ellipse that covers the node with same normalized second central moments;
-
Solidity: the ratio of the area of the node and its convex area;
-
Density: the ratio between the summation of grey value within the node and its area;
-
Heterogeneity: Fraction of pixels that deviate more than a certain range (10% default) from the average intensity.
-
Fractal dimension: Minkowski dimension of the boundary of the node, computed by box-counting method.
-
Minkowski dimension: a way of determining the fractal dimension of set S in a Euclidean space Rn. It is estimated by limit of \( {\lim_{{\tau \to 0}}}\frac{{{N_{\tau }}}}{{1/\varepsilon }} \), where N(ε) is the number of boxes of side length ε required to cover the set S.
Rights and permissions
About this article
Cite this article
Cui, C., Cai, H., Liu, L. et al. Quantitative analysis and prediction of regional lymph node status in rectal cancer based on computed tomography imaging. Eur Radiol 21, 2318–2325 (2011). https://doi.org/10.1007/s00330-011-2182-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2182-7