Abstract
Objective
To assess morphological vascular changes due to an increase in liver fibrosis by using micro-flow imaging (MFI) of contrast-enhanced ultrasound.
Methods
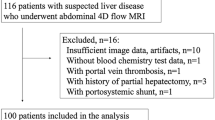
MFI was performed in 47 patients who underwent liver biopsy, and in 10 normal cases. For 27/57 cases, we performed MFI twice in order to assess the reproducibility of the examination, thus yielding a total of 84 examinations. Seven physicians interpreted each case individually by assigning confidence levels for the presence or absence of three imaging features that were related to alteration of portal vein morphology: angle widening, tapering/interruption and tortuosity.
Results
Pearson’s correlation coefficient between the average rating scores based on tortuosity and the histological fibrosis stage was 0.806 (p < 0.001). The diagnostic accuracy of the average area under the ROC curve, which was estimated by use of the confidence levels of tapering/interruption, tortuosity and angle widening, was 0.964 for F1 vs. F2–4, 0.968 for F1–2 vs. F3–4 and 0.910 for F1–3 vs. F4. The average correlation coefficient between the ratings on different images from the same patients was 0.838.
Conclusion
Assessment of morphological intrahepatic vascular changes on MFI may be useful for grading liver fibrosis.








Similar content being viewed by others
References
Anthony PP, Ishak KG, Nayak NC et al (1978) The morphology of cirrhosis. Recommendations on definition, nomenclature, and classification by a working group sponsored by the World Health Organization. J Clin Pathol 31:395–414
Daniel PM, Prichard MML, Reynell PC (1952) The portal circulation in experimental cirrhosis of the liver. J Pathol Bacteriol 114:53–60
Popper H, Elias H, Patty DE (1952) Vascular pattern of the cirrhotic liver. Am J Clin Pathol 22:717–729
Sugimoto K, Moriyasu F, Kamiyama N et al (2008) Analysis of morphological vascular changes of hepatocellular carcinoma by micro flow imaging using contrast-enhanced sonography. Hepatol Res 38:790–799
Shiraishi J, Sugimoto K, Moriyasu F, Kamiyama N, Doi K (2008) Computer-aided diagnosis for the classification of focal liver lesions by use of contrast-enhanced ultrasonography. Med Phys 35:1734–1746
Wilson SR, Jang HJ, Kim TK, Iijima H, Kamiyama N, Burns PN (2008) Real-time temporal maximum-intensity projection imaging of hepatic lesions with contrast-enhanced sonography. AJR Am J Roentgenol 190:691–695
Burns PN (2002) Contrast ultrasound technology. In: Solbital L, Martegani A, Leen E, Correas JM, Burns PN, Becker D (eds) Contrast-enhanced ultrasound of liver diseases. Springer, Milan, pp 1–19
Ichida F, Tsuji T, Omata M et al (1996) New Inuyama classification: new criteria for histological assessment of chronic hepatitis. Int Hepatol Commun 6:112–119
Desmet VJ, Gerber M, Hoofnagle JH, Manns M, Scheuer PJ (1994) Classification of chronic hepatitis: diagnosis, grading and staining. Hepatology 19:1513–1520
Ludwing J (1993) The nomenclature of chronic active hepatitis; An obituary. Gastroenterology 105:274
MacMahon H, Engelman R, Behlen FM et al (1999) Computer-aided diagnosis of pulmonary nodules: results of a large-scale observer test. Radiology 213:723
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
Strader DB, Wright T, Thomas DL, Seeff LB (2004) Diagnosis, management, and treatment of hepatitis C. Hepatology 39:1147–1171
Bruix J, Sherman M (2005) Management of hepatocellular carcinoma. Hepatology 42:1208–1236
De Franchis R (2005) Evolving consensus in portal hypertension: report of the Baveno IV Consensus Workshop on Methodology of Diagnosis and Therapy in Portal Hypertension. J Hepatol 43:167–176
Kelty RH, Baggenstoss AH, Butt HR (1950) The relation of the regenerated liver nodule to the vascular bed in cirrhosis. Gastroenterology 15:285–295
Wai CT, Greenson JK, Fontana RJ et al (2003) A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with hepatitis C. Hepatology 38:518–526
Imbert-Bismut F, Ratziu V, Pieroni L, Charlotte F, Benhamou Y, Poynard T (2001) Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. Lancet 357:1069–1075
Rocky DC, Bissel DM (2006) Noninvasive measures of liver fibrosis. Hepatology 43:S113–S120
Bataller R, Brenner DA (2005) Liver fibrosis. J Clin Invest 115:209–218
Colli A, Fraquelli M, Andreoletti M, Marino B, Zuccoli E, Conte D (2003) Severe liver fibrosis or cirrhosis: accuracy of US for detection - analysis of 300 cases. Radiology 227:89–94
Fridrich-Rust M, Ong MF, Herrmann E et al (2007) Real-time elastography for noninvasive assessment of liver fibrosis in chronic viral hepatitis. AJR Am J Roentgenol 188:758–764
Aguirre DA, Behling CA, Alpert E, Hassanein TI, Sirlin CB (2006) Liver fibrosis: noninvasive diagnosis with double contrast material-enhanced MR imaging. Radiology 239:425–437
Annet L, Materne R, Danse E, Jamart J, Horsmans Y, Van Beers BE (2003) Hepatic flow parameters measured with MR imaging and Doppler US: correlation with degree of cirrhosis and portal hypertension. Radiology 229:409–414
Koinuma M, Ohashi I, Hanafusa K, Shibuya H (2005) Apparent diffusion coefficient measurements with diffusion-weighted magnetic resonance imaging for evaluation of hepatic fibrosis. J Magn Reson Imaging 22:80–85
Huwart L, Sempoux C, Salameh N et al (2007) Liver fibrosis: noninvasive assessment with MR elastography versus aspirate aminotransferase-to-platelet ratio index. Radiology 245:458–466
Poniachik J, Bernstein DE, Reddy KR et al (1996) The role of laparoscopy in the diagnosis of cirrhosis. Gastrointest Endosc 43:568–571
Pagliaro L, Rinaldi F, Craxi A et al (1983) Percutaneous blind biopsy versus laparoscopy with guided biopsy in diagnosis of cirrhosis: a prospective, randomized trial. Dig Dis Sci 28:39–43
Maharaj B, Maharaj RJ, Leary WP et al (1986) Sampling variability and its influence on the diagnostic yield of percutaneous needle biopsy of the liver. Lancet 1:523–525
Acknowledgments
The authors are grateful to Tomihiko Hirokawa, MD, Liu Guang-Jian, MD, Yasuharu Imai, MD, Junich Taira, MD, and Takatomo Sano, MD, for participating as observers; and to Mrs. Elisabeth Lanzl for improving the manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
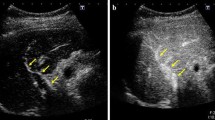
Contrast-enhanced US images with MFI in a 39-year-old healthy man. The cine loop shows regularly and continuously branching portal veins and the regularity of the blood-flow speed of the portal vein branches immediately after the flash, and also shows the spatial and temporal homogeneity of the enhancement of the liver parenchyma a few seconds after the flash. (MPG 1372 kb)
Contrast-enhanced US images with MFI in a 68-year-old woman with F2 disease. MFI cine loop shows slight tortuosity and meandering of the portal vein branches and the irregularity of the blood-flow speed of the portal vein branches immediately after the flash compared with normal liver (S1), and also shows the spatial and temporal heterogeneity of the enhancement of the liver parenchyma a few seconds after the flash. The cine loop also shows dilatation of the hepatic arterial branches immediately after the flash. (MPG 1149 kb)
Contrast-enhanced US images with MFI in a 65-year-old woman with F4 disease. MFI cine loop shows chaotic vascular changes, and also shows the severe spatial and temporal heterogeneity of the liver’s parenchymal enhancement compared with normal liver and F2 disease (S1–S2). (MPG 1384 kb)
Rights and permissions
About this article
Cite this article
Sugimoto, K., Shiraishi, J., Moriyasu, F. et al. Analysis of intrahepatic vascular morphological changes of chronic liver disease for assessment of liver fibrosis stages by micro-flow imaging with contrast-enhanced ultrasound: preliminary experience. Eur Radiol 20, 2749–2757 (2010). https://doi.org/10.1007/s00330-010-1852-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-010-1852-1