Abstract
Background
This technical note introduces diffusion-weighted (DW) MR neurography (MRN) of the sacral plexus with unidirectional motion probing gradients (MPGs).
Methods
This is compared with DW MRN with three-directional and six-directional MPGs.
Results and conclusion
This paper indicates that DW MRN of the sacral plexus should be performed with unidirectional MPGs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Magnetic resonance (MR) imaging, using three-dimensional high-resolution fat-suppressed T2-weighted or T1-weighted sequences, is a useful technique for evaluating pathological conditions of the sacral plexus [1, 2]. Diffusion-weighted (DW) MR imaging (DWI) has recently been introduced as an alternative way to visualize nerves [3–5]. DW MR neurography (MRN) is based on the concept of diffusion-weighted whole-body imaging with background body signal suppression (DWIBS), which allows multiple thin-slice DWI data sets to be obtained [6]. Using this technique, structures of high signal intensity on fat-suppressed T2- and T1-weighted images adjacent to the nerves, such as veins, are well suppressed thanks to the use of motion probing gradients (MPGs), and the trajectory of the nerves is well visualized on maximum intensity projection (MIP) images. DW MRN is different from diffusion tensor imaging (DTI) in that it is just imaging of nerves and does not track the anisotropy of nerves [3–5]. Furthermore, for DW MRN, MPGs are usually applied in no more than three different directions, whereas DTI requires a minimum of six different MPG directions [2–4]. However, the number of directions of MPGs that offers the best visualization of the nerves in DW MRN remains unknown. Theoretically, perpendicular positioning of the MPGs of a DWI sequence of the nerves offers the highest signal for them, as diffusion is relatively more impeded perpendicular to the nerve [7]. The purpose of this study was therefore to introduce DW MRN of the sacral plexus with unidirectional MPGs (anterior-posterior direction only) and to compare it with DW MRN with three-directional and six-directional MPGs.
Materials and methods
Subjects
Our institutional review board approved protocol optimization using volunteer subjects, and written informed consent was obtained from all subjects before the MR examination. Five healthy volunteers [three men, two women, mean age 33.5 years (range, 23–45 years)] underwent DW MRN of the sacral plexus.
DW MRN
All subjects were examined with a 3.0-T MR unit (Achieva; Philips Healthcare, Best, The Netherlands) using a five-element phased-array surface coil. DW MRN was acquired using uni-, three- and six-directional MPGs. Imaging parameters are displayed in Table 1. Of note, image acquisition was performed in the axial plane, because, in our experience, direct coronal imaging tends to suffer from severe image distortion because of the requirement of a larger field of view. MR imaging was performed from the level of the L4 nerve to the inguinal region, including the sciatic nerve, in all volunteers.
MIP post-processing
Two types of coronal MIP images were created: conventional (entire volume) and soap-bubble MIP images. Conventional MIP images included the entire part of the imaged area. Soap-bubble MIP images were generated by dedicated software (SoapBubble, release 5.0; Philips Healthcare). Soap-bubble software allows a curved subvolume of the DW MRN data set to be obtained that closely encompasses the sacral plexus [4, 8]. In each volunteer, the reconstructed soap-bubble volume of DW MRN data sets obtained with uni-, three- and six-directional MPGs was identical. The reconstruction thickness of MIP images was 4 mm.
Image evaluation
Two board-certified radiologists blindly and independently evaluated DW MRN images obtained with uni-, three- and six-directional MPGs, and post-processed with conventional or soap-bubble MIP, using a four-grade scoring system (0 = nerve not visualized; 1 = a part of the nerve is visualized, but the maximum visualized length is less than 1 cm; 2 = nerve moderately well visualized; 3 = nerve clearly visualized), which was applied to the following segments of the sacral plexus: the anterior part of L4, L5, S1, S2, S3, S4 and the lumbosacral trunk, the conjoint part of the sacral plexus and the sciatic nerve.
Furthermore, one board-certified radiologist manually placed regions of interest (ROIs) in both the left and right lumbosacral trunks and sciatic nerves, and in the fat surrounding the nerves, on axial source images of DW MRN datasets obtained with uni-, three- and six-directional MPGs, with size and shape of ROIs being kept as equal as possible among the three sequences. The apparent signal-to-noise ratio (SNR) was calculated as SI(nerve)/SD (SI(fat)), where SI(nerve) is the signal intensity (SI) of the nerve and SD (SI(fat) is the standard deviation of the SI of surrounding fat. The apparent contrast-to-noise ratio (CNR) was calculated as SI(nerve)/SI(fat), where SI(nerve) is the SI of the nerve and SI(fat) is the SI of of surrounding fat.
Statistical analysis
Overall differences in visual scores with regard to depiction of sacral plexus segments according to applied DW MRN sequences (with uni-, three- or six- directional MPGs) and according to the applied post-processing method (conventional MIP or soap-bubble MIP) were assessed using the non-parametric Friedman test. The non-parametric Wilcoxon test was used for paired comparisons when the overall comparison was significant.
Differences in mean SNRs and mean CNRs among the different DW MRN sequences (with uni-, three- or six- directional MPGs) were assessed by using one-way repeated-measures analysis of variance (ANOVA) with a Bonferroni post-hoc test.
The level of statistically significant difference was set at P < 0.05 for all tests. Statistical analyses were performed by using SPSS software, version 16.0 (SPSS, Chicago, IL).
Results
Anatomy of the sacral plexus on DW MRN
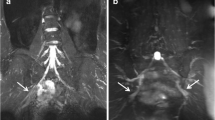
A representative example of DW MRN of the sacral plexus with unidirectional MPGs and post-processed with soap-bubble MIP is shown in Fig. 1.
Diffusion-weighted MR neurography (DW MRN) obtained with unidirectional MPGs and post-processed with soap-bubble MIP in volunteer 1, showing anatomical details of the sacral plexus. Bilateral nerve roots L4 to S3, lumbosacral trunk (LST) and sciatic nerve (SN) are visualized. The femoral nerve (FN), partly originating from nerve root L4, is also demonstrated
Qualitative image evaluation
Qualitative scores are displayed in Table 2. The Friedman test revealed statistically significant differences in visual scores with regard to depiction of sacral plexus segments between the different DW MRN sequences and post-processing methods used, for both observer 1 (chi-squared 197.294, df = 5; P < 0.001) and observer 2 (chi-squared 166.745, df = 5; P < 0.001). Results of pairwise comparisons are displayed in Table 3. DW MRN obtained with unidirectional MPGs and post-processed with soap-bubble MIP was significantly better at visualizing the lumbosacral plexus than all other approaches (P < 0.001 for both observers). Overall visual scores (of both observers combined) for the visualization of the separate sacral plexus segments using DW MRN with unidirectional MPGs and post-processed with soap-bubble MIP are displayed in Table 4. All sacral plexus segments had an overall score of 2 or higher, except for the anterior divisions of the third and fourth sacral nerves (Table 4).
Quantitative image evaluation
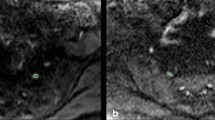
Mean and median SNRs and CNRs are displayed in Table 5. The one-way repeated measures ANOVA revealed a significant overall effect of the type of DW MRN sequence used on both SNR (F = 87.692, df = 2, 57; P < 0.001) and CNR (F = 17.181, df = 2, 57; P < 0.001). Pairwise comparisons revealed that the mean SNR of DW MRN obtained with unidirectional MPGs was significantly higher than that of DW MRN obtained with three- and six-directional MPGs (P < 0.001 for both), and the mean SNR of DW MRN obtained with three-directional MPGs was significantly higher than that of DW MRN obtained with six-directional MPGs (P < 0.001). In addition, the mean CNR of DW MRN obtained with unidirectional MPGs was significantly higher than that of DW MRN obtained with three- and six-directional MPGs (P < 0.003 and P < 0.001), but mean CNR of DW MRN obtained with three-directional MPGs was not significantly different from that of DW MRN obtained with six-directional MPGs (P = 0.063). A representative illustration of the results of the present study is displayed in Fig. 2.
DW MRN post-processed with conventional (entire volume) MIP (left) and soap-bubble MIP (right), obtained with unidirectional (a, d), three-directional (b, e) and six-directional (c, f) MPGs. Quality of DW MRN images post-processed with soap-bubble MIP (d, e, f) is superior to that of corresponding images post-processed with conventional MIP (a, b, c). Quality of images with unidirectional encoding (a, d) is better than those with three-directional encoding (b, e) and those with six-directional encoding (c, f)
Discussion
In the present study we showed that the visualization of the sacral plexus in DW MRN with unidirectional MPGs is superior to that of DW MRN with three-directional or six-directional MPGs. A comparison of DW MRN using three-directional and six-directional MPGs was previously made by Tsuchiya et al. [9], but this comparison was rather unfair because a longer scan time and a higher number of excitations were used for DW MRN with six-directional MPGs. In the present study, a fair comparison (i.e., equal image acquisition time and same effective number of excitations) was made between DW MRN using three-directional and six-directional MPGs, which showed that the former had an obvious tendency to better visualize the sacral plexus. In addition, and more importantly, this study shows that DW MRN with unidirectional MPGs is superior to DW MRN with both three-directional and six-directional MPGs in the same image acquisition time.
We propose two possible explanations for the superiority of DW MRN with unidirectional MPGs over DW MRN with three- or six-directional MPGs. First, DWI is prone to image distortion because of the use of echo-planar imaging [10], and the use of multi-directional MPGs may lead to different distortion directions. These different distortion directions may cause ineffective averaging of single-axis images to create the diffusion trace image, resulting in image blurring and signal decrease in the diffusion trace image. DW MRN with unidirectional MPGs does not have this disadvantage. Second, MPGs applied parallel to the peripheral nerves may not be effective at visualizing them, as diffusion is anisotropic in the human nervous system, including the peripheral nerves [7]. In the present study, unidirectional MPGs were placed in the anterior-posterior direction, which is most perpendicular to the trajectories of the sacral plexus nerves.
In the present study, we also showed that, regardless of the number of MPGs used for DW MRN, the soap-bubble MIP approach is superior to the conventional MIP approach in visualizing the sacral plexus. The effectiveness of the soap-bubble MIP approach was previously shown in a feasibility study on DW MRN of the brachial plexus [4]. In summary, the soap-bubble technique allows projection of a user-defined curved subvolume, encompassing the entire nerve plexus, in a single plane; this enables visualization of the nerve plexus over its entire length and eliminates the superimposing of anatomical structures.
A limitation of the proposed DW MRN technique (unidirectional MPGs, soap-bubble MIP post-processing) is that the anterior divisions of the third and fourth sacral nerve were not always well visualized. Reducing the slice thickness may have allowed better visualization of these nerve roots, although at the expense of a prolonged examination time. In addition, the use of more sophisticated multichannel systems and dedicated coils might further increase the quality of DW MRN images of the sacral plexus. Another limitation is that only healthy volunteers were included and that the clinical impact of the proposed DW MRN technique has not been evaluated yet in a patient population. Further research in a large series of patients is required. Additionally, it is not known whether the proposed DW MRN technique using unidirectional MPGs in the anterior-posterior direction only also performs well in the visualization of other peripheral nerves. Obviously, the course of the peripheral nerves is three-dimensional, and some peripheral nerves run relatively parallel to the anterior-posterior direction. Theoretically, these nerves are not well visualized when using unidirectional MPGs in the anterior-posterior direction only. Therefore, further evaluation of this new DW MRN approach in other parts of the body is necessary. Nevertheless, the significant increase in SNR we observed has encouraged us to obtain better DW MRN images even in other body parts.
In conclusion, the results of this study indicate that DW MRN of the sacral plexus should be performed with unidirectional MPGs. Post-processing the acquired DW MRN images with soap-bubble MIP yields better visualization of the sacral plexus than post-processing with conventional MIP.
References
Maravilla KR, Bowen BC (1998) Imaging of the peripheral nervous system: evaluation of peripheral neuropathy and plexopathy. AJNR Am J Neuroradiol 19:1011–1023
Viallon M, Vargas MI, Jlassi H, Lövblad KO, Delavelle J (2008) High-resolution and functional magnetic resonance imaging of the brachial plexus using an isotropic 3D T2 STIR (short term inversion recovery) SPACE sequence and diffusion tensor imaging. Eur Radiol 18:1018–1023
Takahara T, Yamashita T, Yanagimachi N, Iino M, Koizumi J, Imai Y (2004) Imaging of peripheral nerve disease using diffusion-weighted neurography (DWN) [abstr]. In: Radiological Society of North America scientific assembly and annual meeting program. Oak Brook, Ill: Radiological Society of North America 394
Takahara T, Hendrikse J, Yamashita T et al (2008) Diffusion-weighted MR neurography of the brachial plexus: Feasibility study. Radiology 249:653–660
Yamashita T, Kwee TC, Takahara T (2009) Whole-body magnetic resonance neurography. New Eng J Med in press
Takahara T, Imai Y, Yamashita T, Yasuda S, Nasu S, Van Cauteren M (2004) Diffusion weighted whole body imaging with background body signal suppression (DWIBS): technical improvement using free breathing, STIR and high resolution 3D display. Radiat Med 22:275–282
Beaulieu C (2002) The basis of anisotropic water diffusion in the nervous system—a technical review. NMR Biomed 15:435–455
Etienne A, Botnar RM, Van Muiswinkel AM, Boesiger P, Manning WJ, Stuber M (2002) “Soap-bubble” visualization and quantitative analysis of 3D coronary magnetic resonance angiograms. Magn Reson Med 48:658–666
Tsuchiya K, Imai M, Tateishi H, Nitatori T, Fujikawa A, Takemoto S (2007) Neurography of the spinal nerve roots by diffusion tensor scanning applying motion-probing gradients in six directions. Magn Reson Med Sci 6:1–5
Poustchi-Amin M, Mirowitz SA, Brown JJ, McKinstry RC, Li T (2001) Principles and applications of echo-planar imaging: a review for the general radiologist. Radiographics 21:767–779
Acknowledgement
I would like to acknowledge Mr. Niels Blanken and Mrs. Greet Bouwman for their technical assistance.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Previous presentation
Presented at the annual meeting of the Radiological Society of North America (RSNA) in 2008.
Grant support
This work was partly funded by a grant from the Dutch Scientific Foundation (NWO) for Taro Takahara.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Takahara, T., Hendrikse, J., Kwee, T.C. et al. Diffusion-weighted MR neurography of the sacral plexus with unidirectional motion probing gradients. Eur Radiol 20, 1221–1226 (2010). https://doi.org/10.1007/s00330-009-1665-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-009-1665-2