Abstract
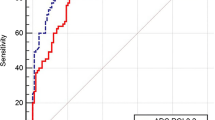
The aim was to evaluate whether morphological criteria in addition to the size criterion results in better diagnostic performance of MRI for the detection of cervical lymph node metastases in patients with head and neck squamous cell carcinoma (HNSCC). Two radiologists evaluated 44 consecutive patients in which lymph node characteristics were assessed with histopathological correlation as gold standard. Assessed criteria were the short axial diameter and morphological criteria such as border irregularity and homogeneity of signal intensity on T2-weighted and contrast-enhanced T1-weighted images. Multivariate logistic regression analysis was performed: diagnostic odds ratios (DOR) with 95% confidence intervals (95% CI) and areas under the curve (AUCs) of receiver-operating characteristic (ROC) curves were determined. Border irregularity and heterogeneity of signal intensity on T2-weighted images showed significantly increased DORs. AUCs increased from 0.67 (95% CI: 0.61–0.73) using size only to 0.81 (95% CI: 0.75–0.87) using all four criteria for observer 1 and from 0.68 (95% CI: 0.62–0.74) to 0.96 (95% CI: 0.94–0.98) for observer 2 (p < 0.001). This study demonstrated that the morphological criteria border irregularity and heterogeneity of signal intensity on T2-weighted images in addition to size significantly improved the detection of cervical lymph nodes metastases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The presence of cervical lymph node metastases is an important prognostic factor in patients with HNSCC as it worsens significantly the treatment outcome [1–8]. The choice of management depends on the existence and extent of lymph node metastases in the neck. Therapy could consist of surgery, radiation therapy, chemotherapy, or a combined therapy. However, all these therapies have a considerable morbidity and mortality. Therefore, treatment refinements like limitation of the field of radiation or a more selective neck dissection are necessary [9–15]. MRI is one of the imaging techniques that is used to guide treatment decisions, but the ability of MRI to discriminate between lymph nodes with and without metastasis is still poor [16].
A commonly used criterion for the assessment of cervical lymph node involvement on MRI is the short axial diameter, and several studies have been undertaken to determine the optimal cutoff size of the short axial diameter for discrimination between metastatic and non-metastatic lymph nodes. On MRI a commonly used size cutoff point is a short axial diameter of 10 mm, but a range varying from 9 to 15 mm has been described [17–21]. The challenge for radiologists remains the detection of metastases in small lymph nodes with a short axial diameter below 10 mm, because mere use of the size criterion will result in misclassification of these nodes as normal. In this respect, according to the literature, the performance of MRI is still poor for detection of lymph node metastases, and this concerns especially the detection of metastases in small lymph nodes [16].
In addition to the size criterion, the use of morphological criteria might have added value to detect metastatic disease in lymph nodes. The diagnostic value of morphological criteria has not been well evaluated in patients with HNSCC. In patients with rectal cancer, Kim et al. demonstrated that in addition to the size criterion, morphological criteria such as borders and heterogeneity could be helpful signs to predict nodal involvement [22].
The aim of our study was to evaluate the accuracy and additional diagnostic value of morphological criteria observed on MRI images, such as border irregularity and heterogeneity of the signal intensity on T2-weighted images and heterogeneity of enhancement on post-contrast T1-weighted images.
Materials and methods
Patients
This study was approved by the local medical ethics committee. Between January 2002 and December 2006 a series of 44 consecutive patients [mean age was 61 years (range: 40–86 years); 11 women and 33 men] with a HNSCC who underwent a unilateral or bilateral supraomohyoid neck dissection (SOHND) (dissection of levels I-III) or radical (modified) neck dissection [R(M)ND] (dissection of levels I-V) was studied. All patients underwent MR imaging as part of the routine diagnostic workup. This was performed on a 1.5-T machine (Gyroscan, Powertrack 6000, Philips, Best, The Netherlands) by using a head-neck coil (Philips, Best, The Netherlands). Table 1 presents the relevant parameters of the MRI protocol.
MR evaluation
One general radiologist (observer 1) and one radiologist specialized in head and neck imaging (observer 2) independently evaluated the MR images retrospectively. Both observers were blinded to each other’s MR assessments, clinical information, and the results of the histological examination.
In the first session, all lymph nodes were determined by position and slice number per neck level. The short axial diameter was recorded per lymph node. All lymph nodes were classified as normal (≤10 mm) or malignant (>10 mm).
After a time interval of 8 weeks, the same MR images were reviewed again by the same radiologists blinded to each others’ MR assessments, clinical information, and the results of the histological examination. For every lymph node the decision was made whether it was normal or metastatic using three morphologic criteria. The first criterion was border as observed on fat-suppressed T2-weighted images (smooth, lobulated, spiculated, indistinct) (Fig. 1 demonstrates the four different borders on the schematic drawing). Smooth (Fig. 2A) and lobulated (Fig. 2B) borders were considered as indicative of normal lymph nodes. Spiculated (Fig. 2C) and indistinct (Fig. 2D) borders were considered as indicative of metastatic lymph nodes. The second criterion was degree of homogeneity of the signal intensity on contrast-enhanced T1-weighted images. A homogeneous enhancement was considered as normal. A heterogeneous enhancement was considered as indicative of metastatic lymph nodes. The third criterion was degree of homogeneity of the signal intensity on T2-weighted images. A homogeneous signal intensity was considered as normal. A heterogeneous signal intensity was considered as indicative of metastatic lymph nodes (Fig. 3).
Transverse turbo spin-echo T2-weighted image of the neck showing an example of heterogeneous signal intensity (SI) in a lymph node in level II on the right side. The lymph node (arrowhead) with a homogenous SI, although a short axial diameter of 13 mm, showed no metastasis, whereas the smaller lymph node (arrow) (short axial diameter 9 mm) with a heterogeneous and eccentric area of low SI (small arrow) revealed metastasis at the pathologic examination
Pathological examination
All neck dissections were performed en bloc. Immediately after the resection, the surgeon positioned the neck dissection specimen on a schematic drawing of the neck in real proportions and fixed it with needles (Fig. 4). The pathologist manually identified and localized the lymph nodes per neck level in the specimen. The short axial diameter of all lymph nodes was recorded. Subsequently, lymph nodes were fixed, sectioned, and hematoxyline-eosine (HE) stained, and the presence of tumor in each lymph node was examined microscopically. The pathological results were used as the reference standard.
Matching MR assessment to pathological examination
The neck was subdivided according to the six different levels in agreement with the classification of the American Joint Committee on Cancer (AJCC); this classification was used by the radiologists when viewing the MR images and used by the pathologist when interpreting the specimen after neck dissection [23].
The results of the measurements on MRI were compared with the results of the pathologic examination of the neck dissection specimens. By recording the combination of the short axial diameter and the exact location of each lymph node, it was possible to perform a topographical correlation for each lymph node per neck level.
Statistical analysis
Inter-observer agreement with respect to the evaluation of the criterion nodal size, and the criteria border irregularity, homogeneity of contrast enhancement on T1-weighted images, and homogeneity of signal intensity on T2-weighted images was expressed by Cohen’s kappa coefficient (κ).
For each lymph node, the scores for the MRI criteria were correlated with the outcome of the histological examination of the neck dissection specimen: presence or absence of lymph node metastasis. Diagnostic performances of nodal size and the new criteria for the diagnosis of metastasis were evaluated using diagnostic parameters, such as sensitivity, specificity, and diagnostic odds ratio (DOR). In diagnosis, one always has to compromise between sensitivity and specificity: as sensitivity increases, specificity will decrease and vice versa. The DOR is a measure of diagnostic performance, which incorporates sensitivity and specificity and thus captures the trade-off between these measures. A DOR = 1 indicates that the test under study has no diagnostic value; a DOR >1 indicates that the test under study (in this case, the new MRI criteria) has the ability to discriminate between lymph nodes with and without metastasis. The larger the DOR is, the larger the discriminative ability [24].
Multivariate logistic regression analysis was used to evaluate whether a criterion, when used in combination with the other criteria, can be used as an independent indicator for differentiating metastatic from non-metastatic lymph nodes. The independent contribution of each criterion to the diagnostic performance is expressed as the DOR, which can be derived by exponentiation of the corresponding regression coefficient, where 95% confidence intervals (95% CI) are used to indicate whether the DOR is significantly different from DOR = 1. Multivariate logistic regression analysis was also used to examine which of the new MRI criteria were most predictive of the presence of metastases and whether the use of these new criteria in addition to size significantly improved the detection of cervical lymph nodes metastases in HNSCC.
The dependent variable in these models was the presence or absence of metastasis according to the pathological examination. The models incorporated as independent variable size as well as the three new MRI criteria. All criteria were entered as dichotomous variables, where abnormal and normal results were coded as 1 and 0, respectively.
Predicted probabilities of metastasis from these models were used to calculate the area under the curve (AUC) with 95% CI as measure of diagnostic performance. The AUC of the model incorporating both the new criteria and the size criterion was compared with the AUC of the model that incorporated only the size criterion. The difference in AUCs for the different models was tested using the method described by Hanley et al., which accounts for the fact that the AUCs are derived from the same sample of patients [25]. A p-value <0.05 was considered to be statistically significant.
Results
In 44 patients a neck dissection was performed: 9 supraomohyoid neck dissections and 37 radical (modified) neck dissections (in 2 patients a bilateral neck dissections). Distribution of the dissected neck levels was as follows; 32 level I, 41 level II, 34 level III, 25 level IV, and 8 level V.
At pathological examination a total of 261 lymph nodes was found: 71 lymph nodes with metastasis and 190 without metastasis (prevalence = 27.2%). In all levels together, a total of 111 lymph nodes was found in level II, 52 lymph nodes in level I, 65 lymph nodes in level III, 25 lymph nodes in level IV, and 8 lymph nodes in level V. Lymph node metastases were present in 33 patients (patient prevalence = 80.5%). The majority (82%) of 261 assessed lymph nodes was scored as having a size <10 mm. The average pathologic yield per patient was 11.5 lymph nodes.
At assessment of the MR images of the dissected neck levels, a total of 360 lymph nodes was detected. Of these lymph nodes, 99 were shown to have a short axial diameter of ≤3 mm. Because these lymph nodes were not detected at pathological examination, they were excluded from further analysis.
A total of 261 lymph nodes, which was found at pathological examination, was matched to lymph nodes that were detected on MRI by the two observers.
For observer 1, scores were lacking in 1 lymph node metastasis, leaving 260 lymph nodes for analysis: 70 lymph nodes with metastasis and 190 without metastasis. For observer 2, complete data were available for all 261 lymph nodes.
Observer agreement was κ = 1.00 for size, κ = 0.62 for border irregularity, κ = 0.51 for signal intensity on contrast-enhanced T1-weighted images, and κ = 0.51 for signal intensity on T2-weighted images.
Table 2 shows the sensitivity, specificity, and diagnostic odds ratio (DOR) with 95% confidence interval (95% CI) for the diagnosis of metastasis for the criteria border (abnormal versus normal) on T2-weighted images, signal intensity on contrast-enhanced T1-weighted images (heterogeneous versus homogeneous), and signal intensity on T2-weighted images (heterogeneous versus homogeneous) for the two observers. With respect to the new criteria, the highest DORs are found for border irregularity and signal intensity on T2-weighted images. The lowest DORs are found for the criterion contrast enhancement on T1-weighted images.
Table 3 shows the results for lymph nodes that were smaller than 10 mm. The DORs associated with the new criteria are smaller compared to the DORs for all lymph nodes, but are still elevated, indicating that the morphologic criteria are also useful for the detection of metastases in small lymph nodes.
Table 4 shows the results from multivariate logistic regression analyses. The DORs associated with border irregularity were 2.61 (95% CI: 1.12–6.08) and 66.2 (95% CI: 20.4 -217) for observer 1 and 2, respectively; for heterogeneity on T2-weighted images DORs were 2.97 (95% CI: 1.42–6.18) and 22.6 (95% CI: 6.40–80.1). The DORs associated with heterogeneity on T1-weighted images are not significantly different from DOR = 1. Another observation was that for observer 2, the DOR associated with size was 1.02, indicating that for this observer size had no additional diagnostic value when considered in combination with the other criteria.
The AUCs for predictive models using size only (≤10 mm versus >10 mm) were 0.67 (95% CI: 0.61–0.73) and 0.68 (95% CI: 0.62–0.74) for observer 1 and 2, respectively. After incorporation of the three new criteria into models, the AUCs increased significantly to 0.81 (95% CI: 0.75–0.87) for observer 1 and to 0.96 (95% CI: 0.94–0.98) for observer 2 (p < 0.001). When the criterion “homogeneity of the signal intensity on contrast-enhanced T1-weighted images” was omitted from the predictive model, there was only a very small decrease in AUC for observer 1 from 0.81 to 0.79 (95% CI: 0.73–0.85) and remained 0.96 (95% CI: 0.93–0.98) for observer 2. This observation indicates that this criterion has little added diagnostic value.
Discussion
The principal finding of this study was that in addition to the size criterion, new criteria, such as border irregularity and heterogeneity on T2-weighted images, result in a better diagnostic performance of MRI for the detection of cervical lymph node metastases in HNSCC.
Accurate assessment of cervical lymph node metastases in HNSCC is important regarding prognosis and choice of management. Detection of lymph node metastases is usually based on the short axial diameter as size criterion. However, many studies have shown that the size criterion alone was not accurate enough as predictor for lymph node metastasis [16]. Sensitivity is poor when the commonly chosen cutoff value of 10 mm is used, and although use of a lower cutoff value, as proposed by van den Brekel et al., results in higher sensitivity, lower cutoff values are associated with low specificity [26]. We evaluated in this study the effect on sensitivity and specificity when lowering the cutoff point from 10 to 7 mm in short axial diameter; sensitivity raised from 43% to 79%, but the associated specificity expectedly lowered from 92% to 64%. However, the corresponding diagnostic odds ratios (DORs) did not differ significantly (DOR = 8.16 with 95% CI 4.09–16.3 versus DOR = 6.43 with 95% CI 3.38–12.23). Another assessment of lymph node dimensions is the measurement of ratios of maximum longitudinal to maximum short axial diameter (l/s ratio). A ratio less than 2, like in round lymph nodes versus elliptical lymph nodes, is indicative of metastatic disease, but this is related to enlarged lymph nodes. Because in our presented series 82% of all assessed lymph nodes were not enlarged – showing short axial diameters less than 10 mm – we used in this study the 10-mm short axial diameter as cutoff point.
Additional morphological criteria for the detection of lymph node metastasis have been evaluated in this study: the degree of border irregularity on T2-weighted images, homogeneity of the signal intensity on contrast-enhanced T1-weighted images, and the homogeneity of the signal intensity on T2-weighted images of lymph nodes.
The results of univariate analyses, with which we compared the diagnostic performance of all four criteria under study, indicate that all criteria, when used alone, help to discriminate between lymph nodes with and without metastasis, but that the discriminative ability was lowest for degree of homogeneity of signal intensity on contrast-enhanced T1-weighted images. This finding also holds after restricting the analysis to lymph nodes smaller than 10 mm. However, when compared with the analysis involving all lymph nodes, DORs were lower, indicating that within small nodes the discriminative ability is poorer. An exception was border irregularity, which for observer 2 was still associated with a high DOR of about 100 (compared with a DOR of 112 in the analysis based on all lymph nodes).
Another morphological criterion that has been used is the presence of central necrosis. However, central necrosis is often seen in the larger involved lymph nodes, which based on their size only would have been classified as malignant anyhow [17–20]. The majority of lymph nodes in our series (82%) showed subcentrimetrical short axial diameters.
Curtin et al. have already described the diagnostic value of the appearance of internal abnormalities in lymph nodes on CT and MRI; however, the performance of MRI was not changed significantly by the addition of information on internal abnormalities [18].
Evaluation of the results of multivariate logistic regression analysis indicates that, if used in combination with the size criterion, for both observers the scores on border irregularity and heterogeneous signal intensity on T2-weighted images contribute significantly to the prediction of the presence of metastatic lymph nodes, whereas the criterion heterogeneity of signal intensity on contrast-enhanced T1-weighted images has no additional diagnostic value.
Explanations for the MR features in metastatic lymph nodes could be the following. Firstly, changes of a smooth or lobulated border of normal lymph nodes into a spiculated or indistinct border could be due to direct extra-nodal tumor infiltration into the peri-nodal fatty tissue. Secondly, this phenomenon could be explained by a desmoplastic reaction around the affected lymph node, the similar feature that can be observed around a primary tumor site. Thirdly, tumor infiltration and presence of softening or necrosis within lymph nodes usually show on the pathological examination an irregular and heterogeneous pattern. This architectural distortion of the nodal parenchyma results in an irregular signal intensity on T2-weighted images and in a heterogeneous signal intensity on the contrast-enhanced T1-weighted images.
The discrepancies in diagnostic performance between the two observers and low inter-observer agreement regarding the new morphological criteria could be explained by the fact that observer 2, experienced in head and neck radiology, was better aware of the diagnostic value of border irregularity and homogeneity of signal intensity than his colleague who had less experience in the assessment of lymph node involvement. In this respect, the results also show that the criterion size for lymph nodes has limited discriminative value for the experienced observer 2. For the more experienced observer, border irregularity and heterogeneity of signal intensity on T2-weighted images are more decisive in the diagnosis. This is reflected by the results of the univariate analysis with high DORs for the criteria border and signal intensity on T2-weighted images (112 and 28.6, respectively), when compared with the low DOR for the size criterion (7.96). Also, in the multivariate logistic regression analysis high DORs are presented for those criteria (66.2 and 22.6, respectively). This is in contrast to the DOR of 1.02 for the size criterion.
Conclusion
Newly assessed morphological criteria like border irregularity and heterogeneity of signal intensity on T2-weighted images in addition to size significantly improved the detection of cervical lymph node metastases on MRI in patients with HNSCC.
References
Kalnins IK, Leonard AG, Sako K et al (1977) Correlation between prognosis and degree of lymph node involvement in carcinoma of the oral cavity. Am J Surg 134:450–454
Jakobsen J, Hansen O, Jorgensen KE et al (1998) Lymph node metastases from laryngeal and pharyngeal carcinomas–calculation of burden of metastasis and its impact on prognosis. Acta Oncol 37:489–493
Kehrl W, Wenzel S, Niendorf A (1998) [Effect of various forms of metastatic lymph node involvement on prognosis of squamous epithelial carcinomas of the upper aerodigestive tract]. Laryngorhinootologie 77:569–575
Ganzer U, Meyer-Breiting E, Ebbers J et al (1982) [Effect of tumor size on lymph node metastasis and type of treatment on the prognosis of hypopharyngeal cancer]. Laryngol Rhinol Otol (Stuttg) 61:622–628
Leemans CR, Tiwari RM, van der Waal I et al (1992) [Neck lymph node dissection in squamous cell carcinoma originating in the head-and-neck area; the significance for the prognosis]. Ned Tijdschr Geneeskd 136:221–225
Foote RL, Olsen KD, Davis DL (1993) Base of tongue carcinoma: patterns of failure and predictors of recurrence after surgery alone. Head Neck 15:300–307
Leemans CR, Tiwari R, Nauta JJ et al (1994) Recurrence at the primary site in head and neck cancer and the significance of neck lymph node metastases as a prognostic factor. Cancer 73:187–190
Taylor JM, Mendenhall WM, Lavey RS (1991) Time-dose factors in positive neck nodes treated with irradiation only. Radiother Oncol 22:167–173
Newman JP, Terris DJ, Pinto HA et al (1997) Surgical morbidity of neck dissection after chemoradiotherapy in advanced head and neck cancer. Ann Otol Rhinol Laryngol 106:117–122
Hillel A, Patten C (1990) Neck dissection: morbidity and rehabilitation. Cancer Treat Res 52:133–147
Sanguineti G, Sormani MP, Benasso M et al (2002) Late local treatment morbidity after accelerated radiotherapy or alternating chemoradiotherapy for advanced head and neck carcinoma. Tumori 88:313–320
Bentzen SM, Saunders MI, Dische S et al (2001) Radiotherapy-related early morbidity in head and neck cancer: quantitative clinical radiobiology as deduced from the CHART trial. Radiother Oncol 60:123–135
Ferlito A, Rinaldo A, Robbins KT et al (2003) Changing concepts in the surgical management of the cervical node metastasis. Oral Oncol 39:429–435
Olsen KD, Caruso M, Foote RL (1994) Primary head and neck cancer. Histopathologic predictors of recurrence after neck dissection in patients with lump node involvement. Arch Otolaryngol Head Neck Surg 120:1370–1374
Byers RM, Wolf PF, Ballantyne AJ (1988) Rationale for elective modified neck dissection. Head Neck Surg 10:160–167
de Bondt RB, Nelemans PJ, Hofman PA et al (2007) Detection of lymph node metastases in head and neck cancer: A meta-analysis comparing US, USgFNAC, CT and MR imaging. Eur J Radiol
van den Brekel MW, Castelijns JA, Stel HV et al (1993) Modern imaging techniques and ultrasound-guided aspiration cytology for the assessment of neck node metastases: a prospective comparative study. Eur Arch Otorhinolaryngol 250:11–17
Curtin HD, Ishwaran H, Mancuso AA et al (1998) Comparison of CT and MR imaging in staging of neck metastases. Radiology 207:123–130
Braams JW, Pruim J, Freling NJ et al (1995) Detection of lymph node metastases of squamous-cell cancer of the head and neck with FDG-PET and MRI. J Nucl Med 36:211–216
Feinmesser R, Freeman JL, Noyek AM et al (1990) MRI and neck metastases: a clinical, radiological, pathological correlative study. J Otolaryngol 19:136–140
Sigal R, Vogl T, Casselman J et al (2002) Lymph node metastases from head and neck squamous cell carcinoma: MR imaging with ultrasmall superparamagnetic iron oxide particles (Sinerem MR) – results of a phase-III multicenter clinical trial. Eur Radiol 12:1104–1113
Kim JH, Beets GL, Kim MJ et al (2004) High-resolution MR imaging for nodal staging in rectal cancer: are there any criteria in addition to the size? Eur J Radiol 52:78–83
Fleming I, Cooper J, Henson D (1997) AJCC Staging manual. Lippenscott-Raven 5th ed, Philadelphia
Glas AS, Lijmer JG, Prins MH et al (2003) The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 56:1129–1135
Hanley JA, McNeil BJ (1983) A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology 148:839–843
van den Brekel MW, Castelijns JA, Snow GB (1998) The size of lymph nodes in the neck on sonograms as a radiologic criterion for metastasis: how reliable is it? AJNR Am J Neuroradiol 19:695–700
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
de Bondt, R.B.J., Nelemans, P.J., Bakers, F. et al. Morphological MRI criteria improve the detection of lymph node metastases in head and neck squamous cell carcinoma: multivariate logistic regression analysis of MRI features of cervical lymph nodes. Eur Radiol 19, 626–633 (2009). https://doi.org/10.1007/s00330-008-1187-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-008-1187-3