Abstract
We determined the efficiency of a screening protocol based on coronary calcium scores (CCS) compared with exercise testing in patients with suspected coronary artery disease (CAD), a normal ECG and troponin levels. Three-hundred-and-four patients were enrolled in a screening protocol including CCS by electron beam computed tomography (Agatston score), and exercise testing. Decision-making was based on CCS. When CCS≥400, coronary angiography (CAG) was recommended. When CCS<10, patients were discharged. Exercise tests were graded as positive, negative or nondiagnostic. The combined endpoint was defined as coronary event or obstructive CAD at CAG. During 12±4 months, CCS≥400, 10–399 and <10 were found in 42, 103 and 159 patients and the combined endpoint occurred in 24 (57%), 14 (14%) and 0 patients (0%), respectively. In 22 patients (7%), myocardial perfusion scintigraphy was performed instead of exercise testing due to the inability to perform an exercise test. A positive, nondiagnostic and negative exercise test result was found in 37, 76 and 191 patients, and the combined endpoint occurred in 11 (30%), 15 (20%) and 12 patients (6%), respectively. Receiver-operator characteristics analysis showed that the area under the curve of 0.89 (95% CI: 0.85–0.93) for CCS was superior to 0.69 (95% CI: 0.61–0.78) for exercise testing (P<0.0001). In conclusion, measurement of CCS is an appropriate initial screening test in a well-defined low-risk population with suspected CAD.
Similar content being viewed by others
Introduction
The management of patients presenting with chest pain remains a major challenge. Although the majority is at low risk of acute coronary syndrome (ACS), obstructive coronary artery disease (CAD) is present in 20% of patients [1]. Furthermore, at least 2% of patients with ACS are mistakenly discharged, resulting in increased mortality [2].
Clinical assessment, an electrocardiogram (ECG), and cardiac markers, such as troponin, allow initial discrimination between a high- and low-risk of ACS [3]. However, risk stratification often requires additional diagnostic testing. Exercise testing and measurement of CCS are frequently used for coronary risk stratification [4–9]. However, exercise testing has a sensitivity and specificity for obstructive CAD of 68% and 77%, respectively, while sensitivity for left main/three-vessel CAD is 86% [10]. Therefore, exercise testing does not detect all patients with (severe) obstructive CAD and the finding of a negative test does not rule out the presence of CAD [1]. Measurement of coronary calcium scores (CCS) may provide more effective triage. The finding of any coronary calcium has a 93–99% sensitivity and 23–75% specificity for obstructive CAD, while the negative predictive value ranges from 95 to 100% [7, 8, 11–16]. A few studies have studied the value of CCS at the emergency department and have shown promising results [6–8]. However, studies comparing CCS and exercise tests have included only patients selected by abnormal exercise tests [17] or the need of coronary angiography [18, 19]. We therefore evaluated a screening protocol based on CCS in low-risk patients suspected of CAD and compared these findings with exercise test results.
Materials and methods
Patients
Consecutive low-risk patients with chest pain or other symptoms of CAD were included. Low-risk was defined as a normal 12-lead ECG, normal troponin, no hemodynamic instability and no abnormalities on physical examination or chest roentgenogram. Coronary risk factors were assessed by history and review of the medical record. Typical angina was defined as the presence of retrosternal pain, increasing with effort and responding to rest or nitroglycerin. If less than three of these characteristics were fulfilled, or a patient suffered from dyspnea, these patients were regarded as having atypical complaints. Other symptoms suggestive of CAD were arrhythmia, history of collaps or referral for screening. Patients with previously documented CAD were excluded. The pretest probability of significant CAD was assessed according to the method by Pryor et al. [20]. A high, and low test probability was defined as a probability of equal to or higher than, and below 44%, respectively [20].
Measurement of coronary calcium scores
Coronary calcium was measured using electron beam computed tomography (EBCT) (e-Speed, GE Medical Systems, South San Francisco, USA). According to patients’ weight and size the beam speed was set to 50 ms (for small or slender patients) or 100 ms (for larger patients). Prospective electrocardiographic triggering was used and set at 42% of the R-R interval. Scans were made without the use of a contrast agent with 130 kV and 895 mAs. A single collimation of 3.0 mm and an increment of 3.0 mm was applied. Radiation exposures were 0.3 mSv and 0.6 mSv for the 50 ms and 100 ms protocols, respectively. Individual exposures were not measured. Assessment of all CCS was performed by one reviewer blinded to the clinical data and the exercise test results. The CCS was obtained by multiplying each area of interest with a factor indicating peak density within the individual area, as was proposed by Agatston et al. [21].
Exercise testing
Bicycle exercise tests were performed in accordance with the guidelines [22, 23]. All tests were independently reviewed by a cardiologist (R.T.) and a research physician (C.G.), who reached a consensus in case of discriminative results. Exercise test end points were defined as follows: positive, in case of ECG evidence of myocardial ischemia (0.1 mV horizontal shift of the ST segment at 80 ms after the J point); intermediate, in case of 30 mmHg decrease in systolic blood pressure and/or ventricular arrhythmia and/or <0.1 mV ST depression and/or anginal complaints in the absence of ECG evidence of ischemia; negative, in the absence of any of the above mentioned criteria; and noninterpretable, if <85% of the predicted heart rate or a rate pressure product <18,000 was achieved. The predicted heart rate was corrected for length, age and sex, making use of a standardized table [24]. Intermediate and noninterpretable results are considered as “nondiagnostic results”. In case exercise testing was not possible, myocardial perfusion imaging was performed.
Myocardial perfusion scintigraphy
Six-hundred MBq of 99 mTc-tetrofosmin was injected at rest and the next day after adenosine or bicycle stress. SPECT images were acquired 1 h after tracer administration using a double-headed gamma-camera (Siemens E.Cam) equipped with low-energy high-resolution collimators. The camera heads were in perpendicular position. Other acquisition parameters were: 32 steps rotation, 20 s per step, 128×128 matrix size, rotation from the 45° right anterior oblique to the 135° left posterior oblique position with the patient laying supine. The scans were reconstructed after filtered-back-projection using a Butterworth 0.30/6 filter. All data were reorientated in order to produce short-axis (SA), horizontal long-axis (HLA) and vertical long-axis (VLA) sections. The perfusion images were scored on CAD by using a 17-segment polar map.
Screening protocol
The former screening protocol for low-risk patients with chest pain included exercise testing. In the current study, measurement of CCS was added. Exercise testing and measurement of CCS were performed in random order. Decision making was based on CCS (Fig. 1). In case of a low CCS, defined as CCS<10, patients were discharged and followed for the occurrence of cardiac events. In case of a high CCS, defined as CCS≥400, coronary angiography (CAG) was recommended to evaluate the presence of obstructive CAD. In case of an intermediate CCS, defined as CCS 10–399, primary prevention measures were recommended, and the decision to perform additional testing was left to the judgment of the treating cardiologist. Both EBCT and exercise testing were performed during office hours. Therefore, in some patients the tests were performed directly after presentation, while others were discharged first and underwent the tests within 3 weeks at the outpatient clinic. Follow-up was obtained in all patients to determine the clinical status at least 4 months after the measurement of CCS by review of the patient’s medical record, telephone interviews of patients or general practitioners. The project is part of a continuous quality-improvement program of the Thoraxcenter, initiated by the board of directors of the University Medical Center Groningen. The protocol was approved by the Institutional Review Board. Informed consent was given by all patients.
Angiographic analysis
All CAGs were analyzed by a senior cardiologist (F.Z.), blinded to the clinical data. By qualitative analysis the coronary arteries were graded as follows: normal coronary arteries, defined as the absence of any coronary lesion; non-obstructive CAD, if maximal luminal obstructions were <50%; and obstructive CAD, if lesions obstructed the lumen ≥50%.
Endpoints
The combined endpoint was defined as a combination of the angiographic endpoint and a cardiac event. The angiographic endpoint was defined as obstructive CAD at CAG (≥50% luminal obstruction). Cardiac events were defined as a revascularization procedure, myocardial infarction or coronary death. Myocardial infarction was defined as ST-elevation myocardial infarction (chest pain and ST-elevation over 1 mm in at least two contiguous leads) or non-ST-elevation acute coronary syndrome [defined as chest pain with positive cardiac markers (troponin or creatinin kinase) and/or dynamic ST-segment changes] [25, 26]. Revascularization procedures included percutaneous coronary intervention (PCI) and coronary artery bypass graft surgery (CABG). Decisions to perform a revascularization procedure were taken by the Thoraxcenter multidisciplinary heart team, which has extensive experience with the RAND-UCLA criteria and takes decisions in accordance with the ESC and ACC/AHA guidelines for PCI and CABG [27–31].
Statistical analysis
Continuous data are expressed as mean ± standard deviation. Significance was reached when P<0.05. To compare the diagnostic yield of CCS with exercise test results, receiver operating characteristic (ROC) curve analysis was performed, and positive and negative predictive values were measured. We compared the area under the curves (AUCs) of both tests for the combined endpoint in all patients and after exclusion of subjects with typical angina. Additional analysis on clinical outcome was performed in those patients in whom exercise testing was not possible and myocardial perfusion scintigraphy was performed, and in those with CCS≥400 in whom the cardiologist decided not to perform CAG. Calculations were performed using the statistical package SPSS version 12.0 (SPSS, Chicago, USA) and STATA 9.0 (College Station, Tex., USA).
Results
Baseline characteristics
From May 2004 till September 2005, 304 patients were consecutively enrolled. Of all exercise tests performed during this period in patients without previous CAD, 90% were included in the study. Clinical characteristics are shown in Table 1. Most patients (n=225) underwent diagnostic testing for atypical complaints. Typical anginal complaints were present in 59 patients, while in 20 patients diagnostic testing was performed for routine screening (n=10), collapse (n=3) or arrhythmia (n=7). The large majority (84%) had a low pretest probability of significant CAD. In 22 patients (7%) myocardial perfusion scintigraphy was performed instead of exercise testing due to the inability to perform an exercise test. The study population represented 90% of the exercise tests performed in new patients.
Follow-up
Follow-up was obtained in all 304 patients (100%). During 12±4 months, 83 CAGs were performed. In 38 patients obstructive CAD was found, followed by a revascularization procedure in 28 patients (21 PCIs and 11 CABGs) (Tables 2, 3). No myocardial infarctions or deaths occurred.
Coronary calcium scores by computed tomography
Low, intermediate and high CCS were detected by EBCT in 159 (52%), 103 (34%) and 42 (14%) patients, respectively. In one patient (0.3%) the CCS quantification failed due to respiration artifacts. In this patient calcium was visible in all coronary arteries and was graded to be of intermediate amount.
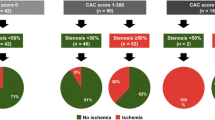
Calcium score ≥400
In 42 patients with a high CCS, positive, negative and nondiagnostic exercise test results were present in 13, 15 and 14 patients, respectively. These results are presented in Table 2. In 37 patients a CAG was performed, showing one- or two-vessel disease in 15 (40%) and three-vessel or left main disease in nine (24%) patients (Table 3). In five patients CAG was not performed because symptoms disappeared with anti-ischemic medication. All patients with CAD received pharmacologic therapy, a revascularization procedure was performed in 17 patients. No myocardial infarctions or deaths occurred. The combined endpoint was observed in 24 of 42 (57%) patients.
Calcium score 10–399
In 103 patients with an intermediate CCS, most patients had negative (n=63) or nondiagnostic (n=31) exercise test results, while the remainder (n=9) had positive exercise test results (Table 2). In 33 patients a CAG was performed, showing obstructive CAD in 14 patients (Tables 2, 3). In these 14 patients the CCS ranged from 23 to 379. All patients with CAD received pharmacologic treatment, a revascularization procedure was performed in nine patients. One patient presented with unstable angina 4 months after PCI due to in-stent-restenosis and underwent repeat PCI. One patient underwent re-PCI for stable angina. No myocardial infarctions or deaths occurred. The combined endpoint occurred in 14 of 103 (14%) patients.
Calcium score <10
In 159 patients with a low CCS, the majority had a negative exercise test result (n=113), but positive and nondiagnostic tests were present in, respectively, 15 and 31 patients. In 13 patients CAG was performed for the following reasons: abnormal exercise test or myocardial perfusion scintigraphy (n=7); typical angina (n=2) and miscellaneous reasons (n=4). In none of these patients obstructive CAD was found (Tables 2, 3). The combined endpoint therefore occurred in 0 (0%) patients.
Comparison with exercise testing
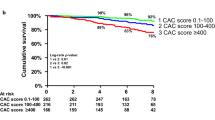
A positive, nondiagnostic and negative exercise test was present in 37 (12%), 76 (25%) and 191 patients (73%), respectively. The rates of high, intermediate and low CCS in these groups were, respectively, 35%, 24% and 41% (positive exercise test); 18%, 41% and 41% (nondiagnostic exercise test); and 8%, 33% and 59% (negative exercise test). The rates of the combined endpoint in the groups with positive and negative exercise test results were, respectively, 30% (11/37) and 6% (12/191). A combined endpoint occurred in 15 (20%) of the 76 subjects with an intermediate exercise test result, namely in nine of 39 subjects with a nondiagnostic test results and in six of 37 subjects with an noninterpretable exercise test result. The rates of the combined endpoint according to CCS and exercise test results are shown in Fig. 2. ROC statistics show an AUC of 0.89 (0.85–0.93) for CCS and 0.69 (0.61–0.78) for exercise testing (P<0.0001; Fig. 3). A CCS>400 yielded a positive predictive value of 57% (41–72%), while the negative predictive value of a CCS<10 was 100% (98–100%). The positive predictive vale of a positive exercise test was 30% (16–47%; P>0.05 compared with CCS>400). The negative predictive value of a negative exercise test result was 94% (89–97%; P<0.05 compared with CCS<10). The AUC for CCS and exercise testing were 0.90 (0.86–0.95) and 0.67 (0.57–0.77) for subjects with a low pretest probability of CAD , and 0.81 (0.68–0.94) and 0.88 (0.76–0.99) for subjects with a high pretest probability of CAD, respectively.
After exclusion of 59 patients with typical angina, ROC analysis showed an AUC of 0.93 (0.88–0.97) for CCS and 0.64 (0.51–0.78) for exercise testing (P<0.001). Additional analysis was performed in 277 patients, after exclusion of five patients with CCS ≥400 without CAG and 22 patients with myocardial perfusion imaging instead of exercise testing. The combined endpoint occurred in 21 (64%) of 33 patients with CCS≥400; in 11 (12%) of 93 patients with CCS 10–400, and in 0 (0%) of 151 patients with CCS<10. The combined endpoint occurred in eight (32%) of 25 patients with positive exercise test results, in 15 (20%) of 74 patients with nondiagnostic exercise test results, and in nine (5%) of 178 patients with negative exercise test results. ROC statistics show an AUC of 0.91 (0.86–0.95) for CCS and 0.72 (0.62–0.82) for exercise testing (P<0.001).
Discussion
The results of this study confirm that measurement of CCS provides effective triage in a well-defined patient group with suspected but low risk of coronary artery disease. In addition, our results indicate that the diagnostic yield of CCS is superior to exercise testing. We included only low-risk patients, which was defined as the absence of prior evidence of CAD, an abnormal 12-lead ECG or elevated serum cardiac markers. The major clinical advantage of our strategy has been facilitation of safe discharge from the hospital in a majority (52%) of these patients, as defined by a low CCS derived from CT. The diagnostic efficacy of our strategy is further demonstrated by high rates of obstructive CAD (especially three-vessel and left main disease) and revascularization procedures in patients with a high CCS.
Measurement of CCS and exercise testing provide fundamentally different diagnostic information. The first test provides information on the amount of calcium in the coronary arteries, while the second test’s purpose is to detect myocardial ischemia. Both an “anatomical” and “functional” approach as initial diagnostic tests in patients with suspected CAD may lead to effective risk stratification [1, 4]. The few studies on risk stratification based on CCS in low-risk patients with chest pain have shown promising results [6–8]. However, studies comparing CCS with exercise testing have not yet been performed in low-risk populations [18, 19]. The former approach at our institution was exercise testing. This was replaced by a protocol in which all patients underwent both exercise testing and CT, and decision making was based on CCS. The efficiency of the current protocol was confirmed by the following observations. First, during a mean follow-up of 12±4 months, no single hard event (myocardial infarction or death) occurred. Second, a large majority (57%) of patients with CCS≥400 had obstructive CAD, and 21% had three-vessel or left main disease. In a majority of these patients a revascularization procedure was necessary according to the ESC and ACC/AHA guidelines for PCI and CABG [27–31]. In subjects with a CCS<10, no coronary events occurred during follow-up. This contrasts with the exercise test results, with 6% of patients with negative exercise test results having obstructive CAD. The high negative predictive value of a low CCS is in concert with many earlier studies [8, 11, 14].
Another major advantage of measurement of CCS may become the detection of minor degrees of CAD. In 34% and 25%, respectively, of our study population, an intermediate amount of coronary calcium and a nondiagnostic exercise test result was present. In patients with CCS 10–399, the presence of CAD has been confirmed and therefore the initiation of primary prevention measures such as life style modification, aspirin and/or statin treatment can be initiated. In contrast to intermediate CCS findings, when exercise testing provides nondiagnostic results, uncertainty with regard to the presence of CAD remains.
Some issues remain to be answered. Due to recent technical improvements CCS can now also be measured by multidetector computed tomography (MDCT) [32–40]. Differences between CCS measurements on EBCT and MDCT have been shown to be similar to the reported individual EBCT and MDCT interscan variabilities of around 20% [32, 35]. Exclusion of coronary calcium by MDCT is as feasible as by EBCT [41, 42]. Comparative studies in low-risk patients with suspected CAD at our department, and in large populations of asymptomatic subjects [32], are currently underway.
We propose to use measurement of CCS as gatekeeper for additional invasive and noninvasive testing [43]. Our protocol enabled us to differentiate between high (CCS>400) and low risk (<100) subjects. However, one-third of our study population had an intermediate CCS (10–399) and obstructive CAD was found in 14% of these subjects. Ideally, in this patient category, a test with high sensitivity for myocardial ischemia should guide the decision to perform CAG, in addition to pharmacologic treatment, as stated above. However, so far, the evidence for use of a clinical protocol in such patients is lacking. Exercise testing can not fulfill this task. Stress echocardiography, myocardial perfusion scintigraphy or stress cardiac magnetic resonance imaging may be better options [44]. Another option is MDCT coronary angiography, which may be clinically useful an may may obviate the need of CAG when luminal stenoses are ruled out [45]. The need for optimization of the current protocol was highlighted by the observation that of the 83 CAGs performed obstructive CAD was found in 38 (46%).
Finally, is CCS more accurate than MDCT coronary angiography? So far, the role of MDCT coronary angiography in the evaluation of patients with suspected CAD has not become established. Compared with measurement of CCS, the advantage of MDCT coronary angiography lies in its information on luminal stenosis [45, 46]. This probably led to a higher number of patients that could be discharged in the evaluation of chest pain in case of negative results (68% with minimal or no stenoses [47] versus 52% with CCS<10 in the current study).
However, since very low CCS are associated with a high negative predictive value, performance of MDCT coronary angiography in such patients cannot be justified. We believe that CT coronary angiography may play a role in subjects with CCS>10. A recent study showed that, in a population scheduled for CAG, the diagnostic yield of MDCT coronary angiography was superior to exercise testing [48]. Further studies are needed to establish the role of MDCT coronary angiography in low risk subjects. In addition, cost-effectiveness should be taken in mind, since in patients with a high probability of CAD, direct CAG may be more cost-effective than a strategy with MDCT coronary angiography [49].
Remarks and limitations
We have chosen a follow-up study design. Our design was limited by the absence of a “gold standard” in every patient, since the procedure to determine the endpoints was influenced by the test results. The absolute numbers of obstructive CAD or clinical events according to exercise test results may therefore have been somewhat biased, since the screening protocol was based on CCS. Furthermore, in patients with low CCS CAG was not performed, thereby decreasing the likelihood of detecting CAD. Our follow-up design restricted the evaluation of cost-effectiveness, which is a limitation, since it was shown that CCS measurement may not be cost-effective [49]. Further studies should be performed to evaluate this issue. Obstructive CAD was measured by qualitative coronary analysis, which is less accurate when compared to quantitative coronary analysis. For this low risk population without previous CAD, symptoms by itself during exercise testing cannot be classified as a positive exercise test. Therefore, symptoms without ECG changes were classified as an intermediate test result. We did not report the intermediate and noninterpretable exercise test results separately, but presented these as one (“nondiagnostic”) group, since both test outcomes do not provide diagnostic certainty and clinical outcome was similar.
Conclusion
In patients with suspected CAD, with a normal ECG and normal cardiac markers, a screening protocol based on coronary calcium scores provides effective triage.
References
deFilippi CR, Rosanio S, Tocchi M, Parmar RJ, Potter MA, Uretsky BF, Runge MS (2001) Randomized comparison of a strategy of predischarge coronary angiography versus exercise testing in low-risk patients in a chest pain unit: in-hospital and long-term outcomes. J Am Coll Cardiol 37:2042–2049
Pope JH, Aufderheide TP, Ruthazer R, Woolard RH, Feldman JA, Beshansky JR, Griffith JL, Selker HP(2000) Missed diagnoses of acute cardiac ischemia in the emergency department. N Engl J Med 342:1163–1170
Hamm CW, Goldmann BU, Heeschen C, Kreymann G, Berger J, Meinertz T (1997) Emergency room triage of patients with acute chest pain by means of rapid testing for cardiac troponin T or troponin I. N Engl J Med 337:1648–1653
Amsterdam EA, Kirk JD, Diercks DB, Lewis WR, Turnipseed SD (2002) Immediate exercise testing to evaluate low-risk patients presenting to the emergency department with chest pain. J Am Coll Cardiol 40:251–256
Polanczyk CA, Johnson PA, Hartley LH, Walls RM, Shaykevich S, Lee TH (1998) Clinical correlates and prognostic significance of early negative exercise tolerance test in patients with acute chest pain seen in the hospital emergency department. Am J Cardiol 81:288–292
McLaughlin VV, Balogh T, Rich S (1999) Utility of electron beam computed tomography to stratify patients presenting to the emergency room with chest pain. Am J Cardiol 84:327–328, A8
Laudon DA, Vukov LF, Breen JF, Rumberger JA, Wollan PC, Sheedy PF (1999) Use of electron-beam computed tomography in the evaluation of chest pain patients in the emergency department. Ann Emerg Med 33:15–21
Georgiou D, Budoff MJ, Kaufer E, Kennedy JM, Lu B, Brundage BH (2001) Screening patients with chest pain in the emergency department using electron beam tomography: a follow-up study. J Am Coll Cardiol 38:105–110
Becker CR, Majeed A, Crispin A, Knez A, Schoepf UJ, Boekstegers P, Steinbeck G, Reiser MF (2005) CT measurement of coronary calcium mass: impact on global cardiac risk assessment. Eur Radiol 15:96–101
Gianrossi R, Detrano R, Mulvihill D, Lehmann K, Dubach P, Colombo A, McArthur D, Froelicher V (1989) Exercise-induced ST depression in the diagnosis of coronary artery disease. A meta-analysis. Circulation 80:87–98
Budoff MJ, Diamond GA, Raggi P, Arad Y, Guerci AD, Callister TQ, Berman D (2002) Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography. Circulation 105:1791–1796
Detrano R, Hsiai T, Wang S, Puentes G, Fallavollita J, Shields P, Stanford W, Wolfkiel C, Georgiou D, Budoff M, Reed J (1996) Prognostic value of coronary calcification and angiographic stenoses in patients undergoing coronary angiography. J Am Coll Cardiol 27:285–290
Kajinami K, Seki H, Takekoshi N, Mabuchi H (1995) Noninvasive prediction of coronary atherosclerosis by quantification of coronary artery calcification using electron beam computed tomography: comparison with electrocardiographic and thallium exercise stress test results. J Am Coll Cardiol 26:1209–1221
Keelan PC, Bielak LF, Ashai K, Jamjoum LS, Denktas AE, Rumberger JA, Sheedy II PF, Peyser PA, Schwartz RS (2001) Long-term prognostic value of coronary calcification detected by electron-beam computed tomography in patients undergoing coronary angiography. Circulation 104:412–417
Nallamothu BK, Saint S, Bielak LF, Sonnad SS, Peyser PA, Rubenfire M, Fendrick AM (2001) Electron-beam computed tomography in the diagnosis of coronary artery disease: a meta-analysis. Arch Intern Med 161:833–838
Clouse ME (2006) How useful is computed tomography for screening for coronary artery disease? Noninvasive screening for coronary artery disease with computed tomography is useful. Circulation 113:125–146
Lamont DH, Budoff MJ, Shavelle DM, Shavelle R, Brundage BH, Hagar JM (2002) Coronary calcium scanning adds incremental value to patients with positive stress tests. Am Heart J 143:861–867
Schmermund A, Baumgart D, Sack S, Mohlenkamp S, Gronemeyer D, Seibel R, Erbel R (2000) Assessment of coronary calcification by electron-beam computed tomography in symptomatic patients with normal, abnormal or equivocal exercise stress test. Eur Heart J 21:1674–1682
Shavelle DM, Budoff MJ, Lamont DH, Shavelle RM, Kennedy JM, Brundage BH (2000) Exercise testing and electron beam computed tomography in the evaluation of coronary artery disease. J Am Coll Cardiol 36:32–38
Pryor DB, Shaw L, McCants CB, Lee KL, Mark DB, Harrell FE Jr, Muhlbaier LH, Califf RM (1993) Value of the history and physical in identifying patients at increased risk for coronary artery disease. Ann Intern Med 118:81–90
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832
Gibbons RJ, Balady GJ, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VF, Mark DB, McCallister BD, Mooss AN, O’Reilly MG, Winters WL, Gibbons RJ, Antman EM, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Hiratzka LF, Jacobs AK, Russell RO, Smith SC (2002) ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines). J Am Coll Cardiol 40:1531–1540
Guidelines for cardiac exercise testing. ESC Working Group on Exercise Physiology, Physiopathology and Electrocardiography (1993) Eur Heart J 14:969–988
Ascoop CAPL, van Zeijl LGPM, Pool J, Simoons ML (1994) Cardiac exercise testing-I indications, staff, equipment, conduct and procedures. Guidelines for cardiac exercise testing. Neth J Cardiol 2:1–11
Van de Werf F, Ardissino D, Betriu A, Cokkinos DV, Falk E, Fox KA, Julian D, Lengyel M, Neumann FJ, Ruzyllo W, Thygesen C, Underwood SR, Vahanian A, Verheugt FW, Wijns W (2003) Management of acute myocardial infarction in patients presenting with ST-segment elevation. The task force on the management of acute myocardial infarction of the european society of cardiology. Eur Heart J 24:28–66
Bertrand ME, Simoons ML, Fox KA, Wallentin LC, Hamm CW, McFadden E, De Feyter PJ, Specchia G, Ruzyllo W (2002) Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 23:1809–1840
Silber S, Albertsson P, Aviles FF, Camici PG, Colombo A, Hamm C, Jorgensen E, Marco J, Nordrehaug JE, Ruzyllo W, Urban P, Stone GW, Wijns W (2005) Guidelines for percutaneous coronary interventions: the task force for percutaneous coronary interventions of the European society of cardiology. Eur Heart J 26:804–847
Meijler AP, Rigter H, Bernstein SJ, Scholma JK, McDonnell J, Breeman A, Kosecoff JB, Brook RH (1997) The appropriateness of intention to treat decisions for invasive therapy in coronary artery disease in The Netherlands. Heart 77:219–224
Rigter H, Meijler AP, McDonnell J, Scholma JK, Bernstein SJ (1997) Indications for coronary revascularisation: a Dutch perspective. Heart 77:211–218
Eagle KA, Guyton RA, Davidoff R, Edwards FH, Ewy GA, Gardner TJ, Hart JC, Herrmann HC, Hillis LD, Hutter AM Jr, Lytle BW, Marlow RA, Nugent WC, Orszulak TA (2004) ACC/AHA 2004 guideline update for coronary artery bypass graft surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1999 Guidelines for Coronary Artery Bypass Graft Surgery). Circulation 110:e340–e437
Smith SC Jr, Dove JT, Jacobs AK, Kennedy JW, Kereiakes D, Kern MJ, Kuntz RE, Popma JJ, Schaff HV, Williams DO, Gibbons RJ, Alpert JP, Eagle KA, Faxon DP, Fuster V, Gardner TJ, Gregoratos G, Russell RO, Smith SC Jr (2001) ACC/AHA guidelines of percutaneous coronary interventions (revision of the 1993 PTCA guidelines)—executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty). J Am Coll Cardiol 37:2215–2239
Detrano RC, Anderson M, Nelson J, Wong ND, Carr JJ, Nitt-Gray M, Bild DE (2005) Coronary calcium measurements: effect of CT scanner type and calcium measure on rescan reproducibility—MESA study. Radiology 236:477–484
Becker CR, Jakobs TF, Aydemir S, Becker A, Knez A, Schoepf UJ, Bruening R, Haberl R, Reiser MF (2000) Helical and single-slice conventional CT versus electron beam CT for the quantification of coronary artery calcification. AJR Am J Roentgenol 174:543–547
Knez A, Becker C, Becker A, Leber A, White C, Reiser M, Steinbeck G (2002) Determination of coronary calcium with multi-slice spiral computed tomography: a comparative study with electron-beam CT. Int J Cardiovasc Imaging 18:295–303
Daniell AL, Wong ND, Friedman JD, Ben-Yosef N, Miranda-Peats R, Hayes SW, Kang X, Sciammarella MG, de YL, Germano G, Berman DS (2005) Concordance of coronary artery calcium estimates between MDCT and electron beam tomography. AJR Am J Roentgenol 185:1542–1545
Horiguchi J, Shen Y, Akiyama Y, Hirai N, Sasaki K, Ishifuro M, Ito K (2006) Electron beam CT versus 16-slice spiral CT: how accurately can we measure coronary artery calcium volume? Eur Radiol 16:374–380
Horiguchi J, Fukuda H, Yamamoto H, Hirai N, Alam F, Kakizawa H, Hieda M, Tachikake T, Marukawa K, Ito K (2007) The impact of motion artifacts on the reproducibility of repeated coronary artery calcium measurements. Eur Radiol 17:81–86
Mahnken AH, Muhlenbruch G, Koos R, Das M, Pohl S, Stanzel S, Gunther RW, Wildberger JE (2006) Influence of a small field-of-view size on the detection of coronary artery calcifications with MSCT: in vitro and in vivo study. Eur Radiol 16:358–364
Muhlenbruch G, Klotz E, Wildberger JE, Koos R, Das M, Niethammer M, Hohl C, Honnef D, Thomas C, Gunther RW, Mahnken AH (2007) The accuracy of 1- and 3-mm slices in coronary calcium scoring using multi-slice CT in vitro and in vivo. Eur Radiol 17:321–329
van Ooijen PM, Vliegenthart R, Witteman JC, Oudkerk M (2005) Influence of scoring parameter settings on Agatston and volume scores for coronary calcification. Eur Radiol 15:102–110
Sandstede JJ, Stoffels J, Wendel F, Ritter C, Beer M, Hahn D (2006) Different reconstruction intervals for exclusion of coronary artery calcifications by retrospectively gated MDCT. AJR Am J Roentgenol 186:193–197
Hoffmann U, Siebert U, Bull-Stewart A, Achenbach S, Ferencik M, Moselewski F, Brady TJ, Massaro JM, O’Donnell CJ (2006) Evidence for lower variability of coronary artery calcium mineral mass measurements by multi-detector computed tomography in a community-based cohort-consequences for progression studies. Eur J Radiol 57:396–402
Bax JJ, van der Wall EE (2006) Assessment of coronary artery disease in patients with (a)symptomatic diabetes. Eur Heart J 27:631–632
Janssen CH, Kuijpers D, Vliegenthart R, Overbosch J, van Dijkman PR, Zijlstra F, Oudkerk M (2005) Coronary artery calcification score by multislice computed tomography predicts the outcome of dobutamine cardiovascular magnetic resonance imaging. Eur Radiol 15:1128–1134
Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JA, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE (2006) Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation 114:1761–1791
Muhlenbruch G, Seyfarth T, Soo CS, Pregalathan N, Mahnken AH (2007) Diagnostic value of 64-slice multi-detector row cardiac CTA in symptomatic patients. Eur Radiol 17:603–609
Goldstein JA, Gallagher MJ, O’Neill WW, Ross MA, O’Neil BJ, Raff GL (2007) A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol 49:863–871
Dewey M, Dubel HP, Schink T, Baumann G, Hamm B (2006) Head-to-head comparison of multislice computed tomography and exercise electrocardiography for diagnosis of coronary artery disease. Eur Heart J DOI 10.1093/eurheartj/ehl148
Dewey M, Hamm B (2007) Cost effectiveness of coronary angiography and calcium scoring using CT and stress MRI for diagnosis of coronary artery disease. Eur Radiol 17:1301–1309
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 2.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc/2.0/.
About this article
Cite this article
Geluk, C.A., Dikkers, R., Perik, P.J. et al. Measurement of coronary calcium scores by electron beam computed tomography or exercise testing as initial diagnostic tool in low-risk patients with suspected coronary artery disease. Eur Radiol 18, 244–252 (2008). https://doi.org/10.1007/s00330-007-0755-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-007-0755-2