Abstract
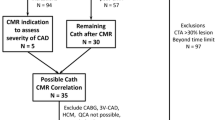
To implement a high-resolution first-pass myocardial perfusion imaging protocol (HRPI) at 3 T, and to evaluate the feasibility, image quality and accuracy of this approach prospectively in patients with suspected CAD. We hypothesized that utilizing the gain in SNR at 3 T to increase spatial resolution would reduce partial volume effects and subendocardial dark rim artifacts in comparison to 1.5 T. HRPI studies were performed on 60 patients using a segmented k-space gradient echo sequence (in plane resolution 1.97 × 1.94 mm2). Semiquantitative assessment of dark rim artifacts was performed for the stress studies on a slice-by-slice basis. Qualitative visual analysis was compared to quantitative coronary angiography (QCA) results; hemodynamically significant CAD was defined as stenosis ≥70% at QCA. Dark rim artifacts appeared in 108 of 180 slices (average extent 1.3 ± 1.2 mm representing 11.8 ± 10.8% of the transmural myocardial thickness). Sensitivity, specifity, and test accuracy for the detection of significant CAD were 89%,79%, and 85%. HRPI studies at 3 T are feasible in a clinical setting, providing good image quality and high accuracy for detection of significant CAD. The presence of dark rim artifacts does not appear to represent a diagnostic problem when using a HRPI approach.




Similar content being viewed by others
References
Hinton DP, Wald LL, Pitts J, Schmitt F (2003) Comparison of cardiac MRI on 1.5 and 3.0 tesla clinical whole body systems. Invest Radiol 38:436–442
Greenman RL, Shirosky JE, Mulkern RV, Rofsky NM (2003) Double inversion black-blood fast spin-echo imaging of the human heart: a comparison between 1.5 T and 3.0 T. J Magn Reson Imaging 17:648–655
Noeske R, Seifert F, Rhein KH, Rinneberg H (2000) Human cardiac imaging at 3 T using phased array coils. Magn Reson Med 44:978–982
Sommer T, Hackenbroch M, Hofer U, Schmiedel A, Willinek WA, Flacke S et al (2005) Coronary MR angiography at 3.0 T versus that at 1.5 T: initial results in patients suspected of having coronary artery disease. Radiology 234:718–725
Wen H, Denison TJ, Singerman RW, Balaban RS (1997) The intrinsic signal-to-noise ratio in human cardiac imaging at 1.5, 3, and 4 T. J Magn Reson 125:65–71
Araoz PA, Glockner JF, McGee KP, Potter DD Jr, Valeti VU, Stanley DW et al (2005) 3 Tesla MR imaging provides improved contrast in first-pass myocardial perfusion imaging over a range of gadolinium doses. J Cardiovasc Magn Reson 7:559–564
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the cardiac imaging committee of the council on clinical cardiology of the American heart association. Int J Cardiovasc Imaging 18:539–542
al-Saadi N, Gross M, Bornstedt A, Schnackenburg B, Klein C, Fleck E et al (2001) [Comparison of various parameters for determining an index of myocardial perfusion reserve in detecting coronary stenosis with cardiovascular magnetic resonance tomography]. Z Kardiol 90:824–834
Barkhausen J, Hunold P, Jochims M, Debatin JF (2004) Imaging of myocardial perfusion with magnetic resonance. J Magn Reson Imaging 19:750–757
Storey P, Chen Q, Li W, Edelman RR, Prasad PV (2002) Band artifacts due to bulk motion. Magn Reson Med 48:1028–1036
Salerno M, Rehwald WG, Judd RM, Kim RJ (2007) Simulation of banding artifacts resulting from realistic cardiac motion during single shot myocardial perfusion. J Cardiovasc Magn Res 9:246–247
Di Bella EV, Parker DL, Sinusas AJ (2005) On the dark rim artifact in dynamic contrast-enhanced MRI myocardial perfusion studies. Magn Reson Med 54:1295–1299
Strach K, Meyer C, Thomas D, Naehle CP, Schmitz C, Litt H et al (2007) High-resolution myocardial perfusion imaging at 3 T: comparison to 1.5 T in healthy volunteers. Eur Radiol 17(7):1829–1835
Hunold P, Schlosser T, Barkhausen J (2006) Magnetic resonance cardiac perfusion imaging-a clinical perspective. Eur Radiol 16:1779–1788
Panting JR, Gatehouse PD, Yang GZ, Grothues F, Firmin DN, Collins P et al (2002) Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med 346:1948–1953
Nagel E, Klein C, Paetsch I, Hettwer S, Schnackenburg B, Wegscheider K et al (2003) Magnetic resonance perfusion measurements for the noninvasive detection of coronary artery disease. Circulation 108:432–437
Paetsch I, Foll D, Langreck H, Herkommer B, Klein C, Schalla S et al (2004) Myocardial perfusion imaging using OMNISCAN: a dose finding study for visual assessment of stress-induced regional perfusion abnormalities. J Cardiovasc Magn Reson 6:803–809
Paetsch I, Jahnke C, Wahl A, Gebker R, Neuss M, Fleck E et al (2004) Comparison of dobutamine stress magnetic resonance, adenosine stress magnetic resonance, and adenosine stress magnetic resonance perfusion. Circulation 110:835–842
Sensky PR, Samani NJ, Reek C, Cherryman GR (2002) Magnetic resonance perfusion imaging in patients with coronary artery disease: a qualitative approach. Int J Cardiovasc Imaging 18:373–383; discussion 85–6
Wolff SD, Schwitter J, Coulden R, Friedrich MG, Bluemke DA, Biederman RW et al (2004) Myocardial first-pass perfusion magnetic resonance imaging: a multicenter dose-ranging study. Circulation 110:732–737
Elkington AG, Gatehouse PD, Cannell TM, Moon JC, Prasad SK, Firmin DN et al (2005) Comparison of hybrid echo-planar imaging and FLASH myocardial perfusion cardiovascular MR imaging. Radiology 235:237–243
Hunold P, Maderwald S, Eggebrecht H, Vogt FM, Barkhausen J (2004) Steady-state free precession sequences in myocardial first-pass perfusion MR imaging: comparison with TurboFLASH imaging. Eur Radiol 14:409–416
Plein S, Radjenovic A, Ridgway JP, Barmby D, Greenwood JP, Ball SG et al (2005) Coronary artery disease: myocardial perfusion MR imaging with sensitivity encoding versus conventional angiography. Radiology 235:423–430
Schwitter J, Nanz D, Kneifel S, Bertschinger K, Buchi M, Knusel PR et al (2001) Assessment of myocardial perfusion in coronary artery disease by magnetic resonance: a comparison with positron emission tomography and coronary angiography. Circulation 103:2230–2235
Stanisz GJ, Odrobina EE, Pun J, Escaravage M, Graham SJ, Bronskill MJ et al (2005) T1, T2 relaxation and magnetization transfer in tissue at 3 T. Magn Reson Med 54:507–512
Kim D, Axel L (2006) Multislice, dual-imaging sequence for increasing the dynamic range of the contrast-enhanced blood signal and CNR of myocardial enhancement at 3 T. J Magn Reson Imaging 23:81–86
Lin W, An H, Chen Y, Nicholas P, Zhai G, Gerig G et al (2003) Practical consideration for 3-T imaging. Magn Reson Imaging Clin N Am 11:615–639, vi
Pattany PM (2004) 3-T MR imaging: the pros and cons. AJNR Am J Neuroradiol 25:1455–1456
Carr JC, Simonetti O, Bundy J, Li D, Pereles S, Finn JP (2001) Cine MR angiography of the heart with segmented true fast imaging with steady-state precession. Radiology 219:828–834
Wang Y, Moin K, Akinboboye O, Reichek N (2005) Myocardial first pass perfusion: steady-state free precession versus spoiled gradient echo and segmented echo planar imaging. Magn Reson Med 54:1123–1129
Schar M, Kozerke S, Fischer SE, Boesiger P (2004) Cardiac SSFP imaging at 3 tesla. Magn Reson Med 51:799–806
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meyer, C., Strach, K., Thomas, D. et al. High-resolution myocardial stress perfusion at 3 T in patients with suspected coronary artery disease. Eur Radiol 18, 226–233 (2008). https://doi.org/10.1007/s00330-007-0746-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-007-0746-3