Abstract
Sports-related shoulder pain and injuries represent a common problem. In this context, glenohumeral instability is currently believed to play a central role either as a recognized or as an unrecognized condition. Shoulder instabilities can roughly be divided into traumatic, atraumatic, and microtraumatic glenohumeral instabilities. In athletes, atraumatic and microtraumatic instabilities can lead to secondary impingement syndromes and chronic damage to intraarticular structures. Magnetic resonance (MR) arthrography is superior to conventional MR imaging in the diagnosis of labro-ligamentous injuries, intrinsic impingement, and SLAP (superior labral anteroposterior) lesions, and thus represents the most informative imaging modality in the overall assessment of glenohumeral instability. This article reviews the imaging criteria for the detection and classification of instability-related injuries in athletes with special emphasis on the influence of MR findings on therapeutic decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decade, understanding of the biomechanics and pathophysiology of the athletic shoulder has significantly improved. Especially in overhead athletes and throwers several pathologic mechanisms have been identified which could not be explained by the traditional concepts of instability and impingement. With an expanded definition, glenohumeral instability is now believed to play the crucial role in the etiology of the painful athletic shoulder. Instability related to sports is not infrequently unrecognized and initiates a vicious circle of secondary impingement, muscular dysfunction, and damage to intraarticular structures that can be devastating and may end the athlete’s career [1–5].
The term “instability” constitutes a spectrum of disorders which includes hyperlaxity, subluxation, and dislocation. Principally, glenohumeral instability can be classified according to its etiology, degree, frequency, and direction. The classic categorization of affected individuals into two groups with traumatic and atraumatic instability represented by the mnemonics TUBS and AMBRII has been supplemented by a further grouping that is mainly comprised of overhead athletes with so-called “microinstability” (microtraumatic instability) and that has been labelled with the acronym AIOS (Table 1). However, it should be emphasized that congenital or acquired hyperlaxity, microinstability, and traumatic instability can overlap particularly in athletes engaged in overhead sports [2, 6].
With reference to the complex relationships beween instability and impingement in overhead athletes, Jobe and co-workers developed a classification system (Table 2) with four groups of pathologic conditions [1]. Whereas groups 1 and 4 represent clearly defined entities with either impingement or instability, groups 2 and 3 include pathologies in which both mechanisms coexist. Group 1 corresponds to classic subacromial impingement, which appears to be relatively rare in athletes, especially in younger individuals. Group 2 refers to microinstability caused by repetitive microtraumatization of the capsulo-labral structures as the main pathologic process, leading to secondary impingement syndromes such as posterosuperior impingement. Group 3 equals the AMBRII group, with athletes that have congenital hyperlaxity of both shoulders as well as of other joints. Group 4 finally includes pure traumatic instabilities without secondary impingement as seen in the TUBS group. In the majority of athletes, traumatic instability occurs in an anterior direction; sports-related posterior “macroinstability” is very rare [1, 2, 4, 7, 8].
Magnetic resonance (MR) imaging plays an important role in the diagnostic work-up of the painful athletic shoulder and with advanced techniques has in many instances already replaced diagnostic arthroscopy. This article discusses the role of MR imaging and MR arthrography in the context of the most common forms of sports-related glenohumeral instability and presents the typical MR arthrographic appearance of their corresponding intraarticular lesions and patterns of injury.
Technical considerations
Particularly in athletes, MR arthrography has been advocated for accurate depiction of labro-ligamentous injuries as well as rotator cuff pathology [5, 7–11]. With the exception of examinations following acute shoulder dislocation, where joint effusion or hemorrhage serve as “natural” contrast media, at our institution MR arthrography is performed on a routine basis in individuals with clinical evidence of shoulder instability and in athletes with unclear shoulder pain. For intraarticular injection of contrast media, several different techniques have been described that can all successfully be employed in MR arthrography [9]. We inject 12–20 ml of a 2.5 mmol/l solution of a gadolinium chelate following fluoroscopically guided puncture of the glenohumeral joint via a classic anterior approach and verification of the intraarticular position of the needle tip by application of a small amount of iodinated contrast media. With the use of a dedicated shoulder coil transverse, coronal oblique, and sagittal oblique T1-weighted spin-echo (SE) sequences are then obtained. Fat-suppression is routinely applied in the coronal oblique plane, but not necessarily in the transverse and sagittal oblique planes. The examination is supplemented by acquisition of a coronal oblique intermediate weighted (echo time=33–45 ms) turbo spin-echo (TSE) sequence with spectral fat-saturation. In patients with anterior instability or suspected posterosuperior glenoid impingement we generally add a T1-weighted SE and/or an intermediate weighted TSE sequence in the ABER (abduction and external rotation) position, achieved by transverse oblique orientation of the images along the long axis of the humerus after flexing the elbow and placing the patient’s hand behind his head or neck (Fig. 1) [5, 9, 12]. Geometric parameters are identical for all pulse sequences with a section thickness of 3 mm and an in plane resolution of 0.4×0.3–0.5 mm.
ABER position: normal findings. a Coronal localizer image of the shoulder obtained in abduction and external rotation shows correct orientation of transverse oblique sections aligned with the humeral shaft. b Resulting transverse oblique T1-weighted MR arthrogram demonstrates normal appearance of anteroinferior labrum (white arrow) with taut IGHL (arrowheads), posterosuperior labrum (black arrow), and supraspinatus tendon (**) (T greater tuberosity of humeral head)
The non-enhanced MR imaging protocol performed after acute shoulder dislocation includes a coronal oblique T1-weighted SE sequence, coronal oblique and transverse intermediate weighted TSE sequences with fat-saturation, and a sagittal oblique T2-weighted TSE sequence with the same geometric parameters as mentioned above.
Traumatic glenohumeral instability
Traumatic glenohumeral instability is typically initiated by a specific traumatic event, followed by other episodes of dislocation or subluxation with a unidirectional pattern [2, 7]. In the vast majority of athletes traumatic instability occurs in an anteroinferior direction when a sudden force overwhelms the anterior capsular structures while the athlete’s arm is in an abducted, externally rotated, and extended position [13]. The resulting combination of injuries represents the source of chronic instability, particularly those involving the inferior glenohumeral ligament (IGHL), which, according to the current opinion, is the most important passive stabilizer of the shoulder joint. The IGHL is formed by an anterior and a posterior band, which represent condensations of the capsule running from the inferior labrum to the humeral neck. The anteroinferior labrum and the anterior band of the IGHL together form the anteroinferior labro-ligamentous complex. The labrum is thought to serve more as an insertion site for the IGHL than to provide stability to the glenohumeral joint by deepening the glenoid fossa [13–15]. Although generally common in sports, this type of instability is rarely observed in throwers or overhead athletes, but, if present, can cause secondary damage to the rotator cuff and the superior and posterior labrum [2].
Labro-ligamentous injuries
The high diagnostic accuracy of MR arthrography in the detection of labro-ligamentous lesions has been demonstrated in several studies. MR arthrography identifies labral tears with a sensitivity of 88–96% and a specificity of 91–98% [14, 16–19]. For the detection of lesions of the superior, middle, and inferior glenohumeral ligaments, Chandnani and co-workers reported sensitivities and specificities of 88–100% [20]. The sensitivities and specificities of unenhanced MR imaging for the diagnosis of labro-ligamentous injuries vary widely in the literature. Although a direct comparison with MR arthrography has not yet been performed in a larger series, we regard the role of standard MR imaging in the diagnostic work-up of shoulder instability as questionable, particularly with a view to chronic cases and the depiction of associated pathology [7, 9, 14, 21, 22]. The advantages of MR arthrography are obvious and result from capsular distension with separation of anatomic structures and improved delineation of tears following entrance of contrast media [8, 9]. MR arthrography thereby allows more confident distinction of pathologic conditions from the common anatomic variations of labral morphology as well as from congenital variants of the glenohumeral ligaments and the labro-ligamentous unit, such as the Buford complex [7, 9, 14, 23–26]. Furthermore, the imaging appearance of Bankart variant lesions has been described only with MR arthrography [7, 14, 27, 28].
Few studies have directly compared MR arthrography and computed tomography (CT) arthrography in the diagnosis of labro-ligamentous injuries. The results suggest that, with the exception of bony changes, CT arthrography is less sensitive than MR arthrography [5, 16]. However, CT arthrography with the use of new multidetector techniques has not yet been fully evaluated in the shoulder. First results indicate that due to its capability of isotropic data acquisition it will probably perform equivalent to MR arthrography [8, 26].
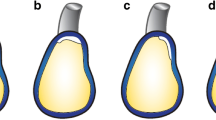
Since modern surgical stabilization procedures aim at restoration of normal anatomy, a more differentiated view at labro-ligamentous injuries has developed in the recent years, and several variants of traumatic lesions of the anteroinferior labrum and/or capsular structures have been described. The following types of lesions should be distinguished (Fig. 2).
Classification of Bankart and Bankart variant lesions. a Bankart lesion, b bony Bankart lesion, c Perthes lesion, d ALPSA (anterior labro-ligamentous periosteal sleeve avulsion) lesion, e GLAD (glenolabral articular disruption) lesion, f HAGL (humeral avulsion of glenohumeral ligaments) lesion. (LLC anteroinferior labro-ligamentous complex, P scapular periosteum, HH humeral head, AC articular cartilage of glenoid, IGHL inferior glenohumeral ligament)
Bankart lesion
The classic labral injury described by Bankart (Fig. 2a) is a complete detachment of the anteroinferior labro-ligamentous complex from the glenoid associated with a rupture of the scapular periosteum [29, 30]. The Bankart lesion represents the most common form of labro-ligamentous injury in patients with first-time traumatic dislocations of the shoulder [31, 32]. Due to the lost contact with the periosteum the lesion shows no tendency to heal. Surgical treatment is by reattachment of the labro-ligamentous complex to the glenoid either arthroscopically or during an open procedure (Bankart repair) [31, 32]. MR arthrography (Fig. 3) typically shows a deformed anteroinferior labrum which is completely separated from the glenoid and therefore is “floating” in the anterior capsular recess adherent to the anterior band of the IGHL [7]. In many cases the torn periosteum can be visualized by transverse MR arthrograms.
Bankart lesion. a Transverse and b coronal oblique T1-weighted MR arthrograms show complete detachment of the anteroinferior labrum (arrows) which “floats” within the anterior capsular recess but remains attached to the IGHL (arrowheads). c Fat-suppressed T1-weighted MR arthrogram obtained in ABER position reveals separation of the anteroinferior labrum from the glenoid edge as well as disruption of the periosteum (arrow). Note taut IGHL adherent to the labrum (arrowhead)
Bony Bankart lesion
In a bony Bankart lesion (Fig. 2b) an osseous fragment of variable size is avulsed from the anteroinferior glenoid together with the labro-ligamentous complex. The size of the fragment influences the therapeutic concept, since larger glenoidal defects can give rise to recurrent instability after stabilizing soft tissue procedures such as the Bankart procedure, particularly in contact athletes [33, 34]. In a study with cadaveric specimens and experimentally created defects of the glenoid rim the critical fragment size was >7 mm in average width [34]. Burkhardt and De Beer coined the term “inverted peer” to describe the visual impression of a significant bone defect of the glenoid at arthroscopy. The “inverted peer” geometry is the reverse of the normal peer-shaped glenoid, which means that its anteroposterior diameter below the midglenoid notch is smaller than that above it [33]. This configuration usually precludes arthroscopic repair and represents an indication for fragment refixation or bone grafting. MR arthrography is less accurate in depiction of bony Bankart lesions compared with CT or CT arthrography [35]. Smaller osseous fragments can easily be overlooked, particularly if fat suppression is used, whereas glenoid fractures with larger fragments can usually be diagnosed with sufficient confidence. Sagittal oblique images are useful to estimate the geometry of the glenoid (Fig. 4).
Bony Bankart lesion. a Coronal oblique and b transverse T1-weighted MR arthrograms show avulsion of a large osseous fragment (arrowheads) from the glenoid together with the attaching anteroinferior labrum and IGHL (arrow). c Sagittal oblique T1-weighted MR arthrogram demonstrates “inverted peer” geometry of glenoid in presence of a “relevant” bony Bankart lesion (arrowhead). Note smaller anteroposterior diameter of glenoid below (**) midglenoid notch than above (++) it. For comparison, normal peer-shaped configuration of glenoid is shown on d sagittal oblique T1-weighted MR arthrogram from individual with stable shoulder (C coracoid process)
Perthes lesion
The Perthes lesion (Fig. 2c) is a variant of the Bankart lesion, which also occurs in patients with acute anterior instability. In the Perthes lesion the anteroinferior labro-ligamentous complex is detached from the glenoid, but unlike in the injury described by Bankart, the periosteum remains intact and is stripped anteromedially [27, 31, 36]. Therefore, unless only loosely attached, the labrum may remain in its normal anatomic position. The integrity of the periosteum allows partial “healing” of the labrum, which might also become resynovialized and thus, although incompetent, can look normal on arthroscopic inspection. Because scar tissue may prevent contrast media from entering the labral tear, nondisplaced Perthes lesions can be difficult to detect on MR arthrography as well [14, 27]. MR arthrograms obtained in the ABER position have been reported to be more sensitive in the diagnosis of Perthes lesions compared with conventional transverse MR arthrograms, although these results are based on a relatively small series of patients [12, 27]. In our experience, the ABER position can at times help to visualize nondisplaced Perthes lesions by separating the base of the anteroinferior labrum from the glenoid and consecutively allowing the entrance of contrast media. On the other hand, displaced or slightly displaced lesions can be realigned with the glenoid and therefore be less conspicuous on ABER images than on transverse images obtained in neutral position (Fig. 5).
Perthes lesion. a Transverse fat-suppressed T1-weighted MR arthrogram shows detachment and slight displacement of the anteroinferior labro-ligamentous complex (arrow) and stripping of the intact scapular periosteum (arrowhead). On b corresponding T1-weighted MR arthrogram obtained in ABER position the anteroinferior labrum is realigned with the glenoid edge by the taut IGHL (arrowhead). Although the tear is still demarcated by contrast media (arrow), it is less conspicuous than on the conventional transverse section in this case. (M middle glenohumeral ligament
ALPSA lesion
The ALPSA (anterior labro-ligamentous periosteal sleeve avulsion) lesion (Fig. 2d) has also been termed “medialized Bankart lesion” and is more common in patients with recurrent than with first-time traumatic dislocations of the shoulder [14, 30]. It represents an anteroinferior labral avulsion that leads to medial displacement and inferior rotation of the labro-ligamentous complex together with the intact periosteum in a sleeve-like fashion, thereby causing incompetence of the IGHL and consecutively anterior instability. The labrum may eventually heal and be resynovialized in this abnormal position [7, 30]. Transformation of the ALPSA lesion into a Bankart lesion by dissection of the complex from the glenoid followed by anatomic refixation (Bankart repair) has been recommended as the treatment of choice [30]. MR arthrography (Fig. 6) shows the typical medial and inferior displacement of the deformed labro-ligamentous complex which is best seen on transverse and coronal oblique images. Contrast medium often outlines a crease or cleft between the glenoid and the nodular shaped fibrous tissue on the glenoid neck, whereas the glenoid edge typically lacks a normal labral structure [7, 14, 30]. Familiarity with these signs can prevent misinterpretation of the ALPSA lesion as an anatomic variant in cases with only slight displacement of the labrum.
GLAD lesion
The GLAD (glenolabral articular disruption) lesion (Fig. 2e), as described by Neviaser is a superficial tear of the anteroinferior labrum in combination with an articular cartilage lesion of the anterior inferior quadrant of the glenoid. The injury is thought to result from glenohumeral impaction while the arm is abducted and externally rotated. Persistent anterior shoulder pain after a fall onto an outstretched arm is the most common clinical presentation, and arthroscopic debridement has been proposed as the treatment of choice [37].
The labral component of the abnormality typically represents an inferior based flap tear without evidence of capsulo-periosteal stripping. Since the anterior fibers of the IGHL remain strongly attached to the labrum and glenoid, the GLAD lesion is usually not associated with anterior instability. The degree of articular cartilage damage is variable and ranges from softening and fibrillation to deep surface defects with loose fragments of cartilage which might remain attached to the anterior labrum and can be undermined by contrast media on MR arthrography (Fig. 7) [7, 14, 28, 37]. Particularly if the chondral lesion is small and therefore hardly visible on MR imaging, the GLAD lesion can look similar to instability-related labral injuries. It is therefore important to note that the labrum is nondisplaced and both the IGHL as well as the periosteum are intact.
HAGL lesion
In contrast to the Bankart lesion and its variants, the HAGL (humeral avulsion of glenohumeral ligaments) lesion (Fig. 2f) does not involve the labro-ligamentous complex at the glenoid, but represents an isolated tear of the IGHL at its humeral insertion following vigorous shoulder dislocation [38, 39]. The injury is associated with anterior instability and represents a pitfall at arthroscopy as well as open shoulder surgery, since it can be overlooked if the area of the humeral neck is not specifically searched for this finding [39, 40]. The majority of patients in whom a HAGL lesion is detected are male and are involved in contact sports, such as rugby, (American) football, or ice hockey [33, 40]. The injury therefore is thought to be relatively rare in countries where these kinds of sport are unpopular. Treatment is by surgical reattachment of the IGHL to its humeral insertion [38, 40]. Particularly in subacute cases with absence of joint effusion, the HAGL lesion can only be diagnosed with confidence if MR arthrography is used. As a sequel of humeral avulsion the IGHL is seen as a J-shaped rather than a U-shaped structure on coronal oblique arthrograms, and contrast extravasation can occur at its insertion site (Fig. 8). Acute injuries are usually associated with edematous changes of the soft tissues anterior to the humeral neck [39]. Approximately 20% of HAGL lesions occur with avulsion of a bony fragment from the humerus (bony HAGL=BHAGL) [41]. On rare occasions the HAGL lesion can be associated with a classic Bankart lesion. Due to the complete isolation of the anterior band of the IGHL which results from this combination of injuries, the lesion has been described as the “floating AIGHL” [42]. Other associated injuries include subscapularis tears and Hill-Sachs defects as well as other osteochondral lesions [38, 40].
HAGL lesion. a Coronal oblique fat-suppressed T1-weighted MR arthrogram and b corresponding intermediate weighted TSE image demonstrate avulsion of the IGHL at its humeral insertion causing a J-shaped configuration of the axillary recess (arrowheads). Contrast extravasation can be seen at the site of the tear (arrows). Bone marrow edema within humeral head (*) was caused by acute Hill-Sachs defect (not shown)
Particularly in athletes, the decision whether an arthroscopic or an open procedure should be performed to achieve the most favourable outcome, can be very difficult and is subject to a controverse discussion. Criteria in favour of open rather than arthroscopic surgery include engagement in contact sports, presence of a relevant glenoid defect and/or Hill-Sachs defect, a HAGL lesion, and poor quality of the labro-ligamentous complex [14, 33, 38, 43]. A recent study could demonstrate the potential of MR arthrography in classification of anteroinferior labro-ligamentous injuries with a view to therapeutic decisions [14]. With arthroscopy as the “gold standard,” Bankart and Bankart variant lesions could be correctly classified with a sensitivity of 77%, a specificity of 91%, and an accuracy of 84%. Furthermore, MR arthrography was capable of identification of injuries with poor quality of the anterior labrum and IGHL, which in high concordance with arthroscopy could not be assigned to one of the specific types of lesions mentioned above. All of these “nonclassifiable” lesions with degenerative changes and scar tissue formation were observed in patients with chronic anterior instability. On MR arthrography (Fig. 9) these injuries are characterized by a swollen inferior glenohumeral ligament complex without distinct depiction of the labrum, IGHL, and scapular periosteum [14].
Hill-Sachs defect
The Hill-Sachs defect represents a compression injury of the posterolateral humeral head which develops during anteroinferior dislocation as the relatively large and soft humeral head impacts against the comparatively small and hard bony glenoid [13]. The incidence of the lesion at arthroscopy varies considerably from 47 to 100% among different series of patients with first-time traumatic dislocations [31, 32, 44]. The depth and size of a Hill-Sachs lesion, ranging from shallow chondral defects to deep osteochondral impaction fractures, is thought to reflect the tightness of the joint capsule [44]. In athletes with hyperlaxity at the time of the first shoulder dislocation, the humeral injury therefore typically is small or absent. Osteochondral Hill-Sachs defects that involve less than one third of the circumference of the humeral head are usually regarded as prognostically irrelevant. Larger lesions, especially if oriented with their long axis parallel to the glenoid, can engage the anterior corner of the glenoid in abduction and external rotation and thus lead to repeated subluxations or redislocations (“engaging” Hill-Sachs defect) [33].
On transverse MR images, the Hill-Sachs defect is typically seen at or slightly above the level of the coracoid process (Fig. 10). False positive diagnoses can occur due to misinterpretation of a normal anatomic groove at the posterolateral humerus, which can often be found caudad to that position [45]. In acute or subacute cases with edema of adjacent bone marrow, the impaction injury can easily be detected on fat-suppressed intermediate/T2-weighted or STIR images. Chronic lesions, particularly if small, are often better visualized by CT [35]. However, clinically significant osteochondral defects are sufficiently demonstrable by MR and rarely necessitate further imaging.
Hill-Sachs defect: MR appearance. a Acute lesion: transverse fat-suppressed intermediate weighted TSE image shows impaction of the posterolateral humeral head (arrowhead) with adjacent bone marrow edema following acute anteroinferior dislocation. b, c Chronic lesions: b transverse fat-suppressed T1-weighted and c transverse T1-weighted MR arthrograms obtained in two different patients several months after anteroinferior dislocation depict circumscribed (b) and extensive (c) osteochondral defects (arrowheads) of the humeral head (C tip of coracoid process)
Atraumatic glenohumeral instability
Atraumatic glenohumeral instability is typically multidirectional and usually evident in individuals with congenital hypermobility syndrome. The diagnosis is predominantly based on the clinical examination, which uncovers bilateral affection of the shoulders in association with generalized hyperlaxity of ligaments and joints [1, 2, 35, 46]. The increased baseline laxity of the shoulder seen in athletes with generalized hypermobility is advantageous for several types of sports, but at the same time harbors a high risk of long-term injury with damage of intra- and periarticular structures [1, 2]. If conservative management fails, multidirectional instability is usually treated surgically by inferior capsular shift and closure of the rotator interval [6].
There are no specific findings to diagnose atraumatic glenohumeral instability by MR imaging or MR arthrography [46]. In most non-athletic AMBRII patients, MR arthrography shows an increased capsular volume but no or little substantial alterations of the intraarticular structures. In athletes, laxity of the capsule is frequently associated with secondary damage to the labrum and the rotator cuff [2]. The labrum may be hypoplastic or torn, but can as well appear swollen and increased in signal intensity due to more or less extensive degenerative change (Fig. 11). Further morphologic alterations can involve the biceps anchor and the articular surface of the rotator cuff [2]. MR arthrography can help with therapeutic decisions by identification or exclusion of significant intraarticular pathology that might represent an indication for surgical repair in addition to capsular reduction.
Atraumatic glenohumeral instability: labral degeneration. a Transverse fat-suppressed T1-weighted and b corresponding sagittal oblique T1-weighted MR arthrograms reveal markedly swollen and enhanced but nondisplaced anterior glenoid labrum in an athlete with multidirectional shoulder instability. Extensive labral degeneration was verified by arthroscopy (not shown)
Microtraumatic glenohumeral instability
Microtraumatic glenohumeral instability is thought to result from chronic traumatization of the capsular structures in throwers and overhead athletes, such as tennis players, swimmers, and handball players. In contrast to atraumatic glenohumeral instability, microinstability is typically seen unilaterally only in the dominant shoulder of the athlete. Whereas repetitive abduction and external rotation cause microtrauma of the anterior capsule and thus can provoke anterior instability, repetitive overhead activity with abduction, flexion, and internal rotation might give rise to posterior microinstability as a result of injury to the posterior labro-ligamentous elements [4, 7, 9, 35, 46].
Structural abnormalities consecutive to microtraumatic glenohumeral instability can be depicted by MR arthrography and include laxity of the anterior or posterior capsule, labral injuries ranging from degeneration and fraying to tearing and detachment, SLAP (superior labral anteroposterior) lesions, and tears of the rotator cuff caused by secondary impingement [2].
Posterosuperior glenoid impingement (PSI)
PSI is a form of internal impingement which represents a common problem in throwers and overhead athletes, presenting with acute or chronic posterior shoulder pain [4, 5, 47, 48]. The basic observation was reported by Walch, who described impingement between the articular side of the supraspinatus tendon and the posterosuperior edge of the glenoid evident in abduction and external rotation [49]. In throwers and overhead athletes, PSI can lead to a typical pattern of injuries, the so-called “kissing lesions”, which includes corresponding lesions of the undersurface of the rotator cuff, the posterosuperior labrum, the greater tuberosity, and the superior bony glenoid [47, 48, 50–52]. The development of PSI has been attributed to chronic injury (repetitive stretching) of the anterior capsular structures, particularly the IGHL, with consecutive anterior microinstability, which causes anterior subluxation of the humeral head in abduction and external rotation during overhead movements, and thus allows excessive contact between the rotator cuff and the posterosuperior glenoid [47, 48]. However, this theory is not generally accepted. Other authors described a contracture of the posteroinferior capsule and a posterior SLAP lesion as the essential lesions for the development of PSI in throwers [3]. Although the basic mechanism is still subject to discussion, the high coincidence of PSI and SLAP lesions is undoubted. Furthermore, there is apparently a huge overlap of clinical symptoms in athletes with SLAP lesions, PSI, or both. It is important to stress that contact between the undersurface of the rotator cuff and the posterosuperior glenoid, as seen on arthroscopy, is not pathologic per se. Posterosuperior glenoid impingement should only be diagnosed if this contact is associated with clinical symptoms and corresponding lesions of the involved anatomic structures [2, 13, 51, 52]. Conservative treatment is usually suited in athletes with minor structural abnormalities, whereas surgical debridement and repair (eventually in combination with capsular plication) are indicated in the presence of relevant rotator cuff and labral lesions.
MR imaging can be used to confirm the diagnosis of PSI and to help with therapeutic decisions by demonstrating the extent of articular damage. Since MR arthrography has been shown to be more accurate than conventional MR imaging in the detection of partial rotator cuff tears, labral tears, and SLAP lesions, it is also regarded as the method of choice in athletes with suspected PSI, which is accompanied by a combination of these abnormalities [50, 53–55]. MR arthrograms (Fig. 12) typically show articular-sided partial tearing of the supraspinatus and/or infraspinatus tendons. The supraspinatus lesion, unlike in patients with subacromial impingement, usually involves the posterior part of the tendon. Damage to the posterosuperior labrum ranges from degenerative change and fraying to tears and detachment and might be associated with ganglia and SLAP lesions. Alterations of bone at the greater tuberosity and the superior glenoid are best demonstrated by fat-suppressed intermediate or T2-weighted images and include erosions, bone marrow edema, cyst formation, and sclerosis [50–52]. MR arthrograms obtained in the ABER position (Fig. 12d,e) usually show contact between the lesions of the rotator cuff and the superior labrum/glenoid and might even reveal interposition of the supraspinatus tendon pinched between the glenoid and the greater tuberosity. Furthermore, the ABER position is useful in demonstration of subluxation of the humeral head and depiction of abnormalities of the anterior capsule. The anterior band of the IGHL can appear attenuated and elongated or might even be torn [50].
PSI: spectrum of findings on MR arthrography. a Transverse fat-suppressed T1-weighted MR arthrogram and b, c corresponding coronal oblique images obtained in a tennis player with posterior shoulder pain show a posterosuperior labral tear (arrow in a) associated with an articular-sided partial tear of the posterior aspect of the supraspinatus tendon (arrowhead in b) and a SLAP type 2 lesion (arrow in c). Note large volume of anterior capsule (* in a). d, e T1-weighted MR arthrograms obtained in ABER position from two athletes with PSI: d Arthrogram demonstrates the “kissing lesion” pattern with corresponding tears of the posterosuperior labrum (white arrow) and the undersurface of the supraspinatus tendon (black arrowhead) accompanied by sclerosis of the greater tuberosity of the humeral head at the contact zone with the glenoid (black arrow). Note elongation of the IGHL (white arrowhead). e Arthrogram shows interposition of the supraspinatus tendon (*) between the greater tuberosity and the superior glenoid as well as a tear of the IGHL (arrowhead) with consecutive contrast extravasation
SLAP lesions
SLAP lesions of the shoulder are common injuries in athletes which represent tears of the superior glenoid labrum that extend in an anterior to posterior direction [55, 56]. Four different types of SLAP lesions have been described in the original classification by Snyder:
-
Type 1:
degenerative fraying of the superior labrum;
-
Type 2:
avulsion of the superior labrum and biceps anchor from the glenoid;
-
Type 3:
bucket-handle tear of the superior labrum with preserved biceps anchor;
-
Type 4:
bucket-handle tear of the superior labrum involving the long head of biceps tendon [56].
This classification has been expanded with several further types of lesions, which mainly represent combinations of the most common form, the SLAP type 2 lesion, with other injuries of the labrum, medial glenohumeral ligament, or rotator cuff. However, only the Snyder classifications have found wide acceptance, and most institutions categorize these injuries as type 1–4 with or without asscociated lesions. Whereas type 1 and 2 lesions are typically caused by repetitive torsion of the biceps anchor (the so-called “peelback mechanism”) in throwers and overhead athletes, types 3 and 4 lesions are thought to occurr more often after a fall onto an outstretched arm or onto a flexed elbow [3, 55, 56]. Furthermore, type 2 lesions are frequently observed in athletes with traumatic anterior shoulder instability, where they develop in association with lesions of the anteroinferior labro-ligamentous complex (most often a classic Bankart lesion). In these cases, the labro-ligamentous avulsion can be considered as the main lesion, with the SLAP lesion being an associated injury [55]. Surgical treatment is indicated in all types of SLAP lesions except type 1 lesions which are usually of no clinical relevance. Since type 2 and 4 lesions impair the stabilizing function of the biceps insertion and therefore can provoke glenohumeral instability, secondary impingement, and rotator cuff lesions, they are commonly treated by refixation. Type 3 bucket-handle tears are usually not surgically reattached but treated by simple debridement [55, 56].
MR arthrography has proved to be superior to conventional MR imaging with regard to the identification of SLAP lesions and has been shown to be reliable in assessment of the stability of the biceps anchor and the detection of associated injuries [55, 57–59]. However, its ability to correctly classify the different types of lesions is limited [55].
Most SLAP lesions are best depicted on MR arthrograms oriented in the coronal oblique plane (Fig. 13). Increased signal intensity and/or surface irregularity of the superior labrum can be seen in type 1 lesions which, however, can only infrequently be diagnosed by MR imaging. Type 2 lesions are characterized by linear extension of contrast media into the superior labrum and the biceps anchor. This most common type of SLAP lesion also represents the most problematic in terms of differential diagnosis. False positive and false negative diagnoses of a SLAP type 2 lesion can be caused by misinterpretation of a sublabral recess as a tear and vice versa [55]. The sublabral recess (Fig. 14) is a very common anatomic variant with an incidence of >70% in cadaveric studies [26, 60]. It represents a variably sized synovialized cleft between the superior labrum and the bony glenoid which is typically oriented medially and points at the supraglenoidal tubercule [26, 55, 60]. The most important criterion for the presence of a SLAP type 2 lesion rather than a sublabral recess therefore is lateral or superior extension of the tear. If the tear extends medially (like a sublabral recess) it often shows irregular margins and/or a relatively wide separation between the labrum and the glenoid. In individuals with traumatic anterior instability the type 2 lesion often originates from an anteroinferior tear of the labro-ligamentous complex that extends cranially up into the superior labrum and the biceps anchor (Fig. 15) [55]. Type 3 lesions are characterized by a vertical and an additional horizontal contrast interface which separate the avulsed superior labrum as a triangular-shaped fragment from the intact biceps tendon. In Type 4 lesions the horizontal component of the tear additionally extends into the long head of biceps tendon. The bucket-handle fragment therefore is composed of the superior labrum as well as a portion of the tendon and might be more or less displaced from the superior glenoid [55, 59].
Sublabral recess. Coronal oblique T1-weighted MR arthrogram demonstrates medially oriented cleft (arrowhead) between the superior labrum and the glenoid outlined by contrast media which was also diagnosed as a sublabral recess with a stable biceps insertion on arthroscopy (not shown). Note meniscoid shape of superior labrum (*) and integrity of the biceps anchor (arrow)
SLAP type 2 lesion in association with a Bankart lesion in traumatic anterior glenohumeral instability. a Coronal oblique fat-suppressed T1-weighted MR arthrogram shows superior extension of contrast media into the superior labrum and biceps anchor (arrowhead). b Corresponding sagittal oblique MR arthrogram reveals tearing of the entire anterior labrum (arrowheads) extending from inferior to superior. c, d Corresponding transverse MR arthrograms demonstrate detachment of the anterior labrum that continues as a classic Bankart lesion anteroinferiorly (arrows)
Conclusion
Sports-related glenohumeral instability is a complex and in many aspects still controversial subject. MR imaging can play an important role in evaluation of the athlete’s shoulder if it aims at providing essential information for therapeutic decisions at eye level with diagnostic arthroscopy. Therefore, the radiologist should be familiar with the mechanisms and classification of injuries as well as the advantages and limitations of his examination techniques. At present, MR arthrography represents the best evaluated and most informative imaging technique for the assessment of shoulder pathology in many aspects and thus, appears to be most valuable for the diagnostic work-up of glenohumeral instability and unclear shoulder pain in athletes.
References
Jobe FW, Kvitne RS, Giangarra CE (1989) Shoulder pain in the overhand or throwing athlete. The relationship of anterior instability and rotator cuff impingement. Orthop Rev 18:963–975
Meister K (2000) Injuries to the shoulder in the throwing athlete. Part one: biomechanics, pathophysiology, classification of injury. Am J Sports Med 28:265–275
Burkhart SS, Craig DM, Kibler WB (2003) The disabled throwing shoulder: spectrum of pathology. Part I: pathoanatomy and biomechanics. Arthroscopy 19:404–420
Belling Sorensen AK, Jorgensen U (2000) Secondary impingement in the shoulder: an improved terminology in impingement. Scand J Sci Sports 10:266–278
Roger B, Skaf A, Hooper AW, Lektrakul N, Yeh L, Resnick D (1999) Imaging findings in the dominant shoulder of throwing athletes: comparison of radiography, arthrography, CT arthrography, and MR arthrography with arthroscopic correlation. Am J Roentgenol 172:1371–1380
Matsen FA, Lippit SB, Sidles JA, Harryman DT (1994) Practical evaluation and management of the shoulder. Saunders, Philadelphia, pp 59–109
Beltran J, Rosenberg ZS, Chandnani VP, Cuomo F, Beltran S, Rokito A (1997) Glenohumeral instability: evaluation with MR arthrography. Radiographics 17:657–673
Farber JM, Buckwalter KA (2002) Sports related injuries of the shoulder: instability. Radiol Clin N Am 40:235–249
Elentuck D, Palmer WE (2004) Direct magnetic resonance arthrography. Eur Radiol 14:1956–1967
Shankman S, Bencardino J, Beltran J (1999) Glenohumeral instability: evaluation using MR arthrography of the shoulder. Skeletal Radiol 28:365–382
Tirman PF, Smith ED, Stoller DW, Fritz RC (2004) Shoulder imaging in athletes. Semin Musculoskelet Radiol 8:29–40
Cvitanic O, Tirman PF, Feller JF, Bost FW, Minter J, Carrol KW (1997) Using abduction and external rotation of the shoulder to increase the sensitivity of MR arthrography in revealing tears of the anterior glenoid labrum. Am J Roentgenol 169:837–844
Armfield DR, Stickle RL, Robertson DD, Towers JD, Debski RE (2003) Biomechanical basis of common shoulder problems. Semin Musculoskelet Radiol 7:5–18
Waldt S, Burkart A, Imhoff AB, Bruegel M, Rummeny EJ, Woertler K (2005) Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology 237:578–583
O’Connell PW, Nuber GW, Mileski RA, Lautenschalger E (1990) The contribution of glenohumeral ligaments to anterior stability of the shoulder joint. Am J Sports Med 18:579–584
Chandnani VP, Yeager TD, Bencardino T, Christensen K, Galgliardi JA, Heitz DR, Baird DE, Hansen MF (1993) Glenoid labral tears: prospective evaluation with MR imaging, MR arthrography, and CT arthrography. Am J Roentgenol 161:1229–1235
Tirman PF, Stauffer AE, Crues JV et al (1993) Saline magnetic resonance arthrography in the evaluation of glenohumeral instability. Arthroscopy 9:550–559
Palmer WE, Brown JH, Rosentahl DI (1994) Labral-ligamentous complex of the shoulder: evaluation with MR arthrography. Radiology 190:645–651
Palmer WE, Caslowitz PL (1995) Anterior shoulder instability: diagnostic criteria determined from prospective analysis of 121 MR arthrograms. Radiology 197:819–825
Chandnani VP, Gagliardi JA, Murnane TG et al (1995) Glenohumeral ligaments and shoulder capsular mechanism: evaluation with MR arthrography. Radiology 196:27–32
Garneau RA, Renfrew DL, Moore TE, El-Khoury GY, Nepola JV, Lemke JH (1991) Glenoid labrum: evaluation with MR imaging. Radiology 179:519–522
Gusmer PB, Potter HG, Schatz JA et al (1996) Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology 200:519–524
Zanetti M, Carstensen T, Weishaupt D, Jost B, Hodler J (2001) MR arthrographic variability of the arthroscopically normal glenoid labrum: qualitative and quantitative assessment. Eur Radiol 11:559–566
Beltran J, Bencardino J, Padron M, Shankman S, Beltran L, Ozkarahan G (2002) The middle glenohumeral ligament: normal anatomy, variants and pathology. Skeletal Radiol 31:253–262
Park YH, Lee JY, Moon SH, Mo JH, Yang BK, Hahn SH, Resnick D (2000) MR arthrography of the labral capsular ligamentous complex in the shoulder: imaging variations and pitfalls. Am J Roentgenol 175:667–672
Waldt S, Metz S, Burkart A, Mueller D, Bruegel M, Rummeny EJ, Woertler K (2006) Variants of the superior labrum and labor-bicipital complex: a comparative study in shoulder specimen using MR arthrography, multi-slice CT arthrography, and anatomic dissection. Eur Radiol 16:451–458
Wischer TK, Bredella MA, Genant HK, Stoller DW, Bost FW, Tirman PF (2002) Perthes lesion (a variant of the Bankart lesion): MR imaging and MR arthrographic findings with surgical correlation. Am J Roentgenol 178:233–237
Sanders TG, Tirmann PF, Linares R, Feller JF, Richardson R (1999) The glenolabral articular disruption lesion: MR arthrography with arthroscopic correlation. Am J Roentgenol 172:171–175
Bankart ASB (1938) The pathology and treatment of recurrent dislocation of the shoulder. Br J Surg 26:23–39
Neviaser TJ (1993) The anterior labroligamentous periosteal sleeve avulsion lesion: a cause of anterior instability of the shoulder. Arthroscopy 9:17–21
Taylor DC, Arciero RA (1997) Pathologic changes associated with shoulder dislocations: arthroscopic and physical examination findings in first-time traumatic anterior dislocations. Am J Sports Med 25:306–311
Norlin R (1993) Intraarticular pathology in acute, first-time shoulder dislocation: an arthroscopic study. Arthroscopy 9:546–549
Burkhart SS, De Beer JF (2000) Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 16:677–694
Itoi E, Lee SB, Berglund LJ, Berge LL, An KN (2000) The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 82:35–46
Blum A, Coudane H, Molé D (2000) Gleno-humeral instabilities. Eur Radiol 10:63–82
Perthes G (1906) Über Operationen mit habitueller Schulterluxation. Deutsch Z Chir 85:199–227, [Article in German]
Neviaser TJ (1993) The GLAD lesion: another cause of anterior shoulder pain. Arthroscopy 9:22–23
Wolf EM, Cheng JC, Dickson K (1995) Humeral avulsion of glenohumeral ligaments as a cause of anterior shoulder instability. Arthroscopy 11:600–607
Bui-Mansfield LT, Taylor DC, Uhorchak JM, Tenuta JJ (2002) Humeral avulsion of the glenohumeral ligament: imaging features and a review of the literature. Am J Roentgenol 179:649–655
Bokor DJ, Conboy VB, Olson C (1999) Anterior instability of the glenohumeral joint with humeral avulsion of the glenohumeral ligament: a review of 41 cases. J Bone Joint Surg Br 81:93–96
Oberlander MA, Morgan BE, Visotsky JL (1996) The BHAGL lesion: a new variant of anterior shoulder instability. Arthroscopy 12:627–633
Warner JJ, Beim JM (1997) Combined Bankart and HAGL lesion associated with anterior shoulder instability. Arthroscopy 13:749–752
Lintner SA, Speer KP (1997) Traumatic anterior glenohumeral instability: the role of arthroscopy. J Acad Orthop Surg 5:233–239
Calandra JJ, Baker CL, Uribe J (1989) The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. Arthroscopy 5:254–257
Richards RD, Sartoris DJ, Pathria MN, Resnick D (1994) Hill-Sachs lesion and normal humeral groove: MR imaging features allowing their differentiation. Radiology 190:665–668
Sanders TG, Morrison WB, Miller MD (2000) Imaging techniques for the evaluation of glenohumeral instability. Am J Sports Med 28:414–434
Jobe CM (1995) Posterior superior glenoid impingement: expanded spectrum. Arthroscopy 11:530–536
Jobe CM (1996) Superior glenoid impingement. Current concepts. Clin Orthop Rel Res 330:98–107
Walch G, Liotard JP, Boileau P, Noel E (1991) Postero-superior glenoid impingement. Another impingement of the shoulder. Rev Chir Orthop Reparatrice Appar Mot 77:571–574 [Article in French]
Tirman PF, Bost FW, Gravin GJ, Peterfy CG, Mall JC, Steinbach LS, Feller JF, Crues JV 3rd (1994) Posterosuperior glenoid impingement of the shoulder: findings at MR imaging and MR arthrography with arthroscopic correlation. Radiology 193:431–436
Kaplan LD, McMahon PJ, Towers J, Irrgang JJ, Rodowsky MW (2004) Internal impingement on magnetic resonance imaging and arthroscopic evaluation. Arthroscopy 7:701–704
Giaroli EL, Major NM, Higgins LD (2005) MRI of internal impingement of the shoulder. Am J Roentgenol 185:925–929
Palmer WE, Brown JH, Rosenthal DI (1993) Rotator cuff: evaluation with fat-suppressed MR arthrography. Radiology 188:683–687
Ferrari FS, Governi S, Burresi F, Vigni F, Stefani P (2002) Supraspinatus tendon tears: comparison of US and MR arthrography with surgical correlation. Eur Radiol 12:1211–1217
Waldt S, Burkart A, Lange P, Imhoff AB, Rummeny EJ, Woertler K (2004) Diagnostic performance of MR arthrography in the assessment of superior labral anteroposterior lesions of the shoulder. Am J Roentgenol 182:1271–1278
Snyder SJ, Karzel RP, Del-Pizzo W, Ferkel RD, Friedmann MJ (1990) SLAP lesions of the shoulder. Arthroscopy 6:274–279
Tuite MJ, Cirillo RL, De Smet AA, Orwin JF (2000) Superior labrum anterior-posterior (SLAP) tears: evaluation of three MR signs on T2-weighted images. Radiology 215:841–845
Yoneda M, Izawa K, Hirooka A, Hayashida K, Wakitani S (1998) Indicators of superior glenoid labral detachment on magnetic resonance imaging and computed tomography arthrography. J Shoulder Elbow Surg 7:2–12
Jee WH, McCauley TR, Katz LD, Matheny JM, Ruwe PA, Daigneault JP (2001) Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: reliability and accuracy of MR arthrography for diagnosis. Radiology 218:127–132
Kreitner KF, Botchen K, Rude J, Bittinger F, Krummenauer F, Thelen M (1998) Superior labrum and labral-bicipital complex: MR imaging with pathologic-anatomic and histologic correlation. Am J Roentgenol 170:599–605
Acknowledgement
We thank Darko Leko for assistance in preparation of schematic drawings.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 2.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by-nc/2.0/.
About this article
Cite this article
Woertler, K., Waldt, S. MR imaging in sports-related glenohumeral instability. Eur Radiol 16, 2622–2636 (2006). https://doi.org/10.1007/s00330-006-0258-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-006-0258-6