Abstract
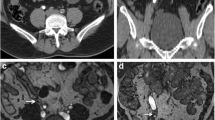
The aim of this study was to determine the prevalence of filling defect artefacts (FDA) in magnetic resonance urography (MRU). Retrospectively, we assessed MRU examinations of 45 patients with neurogenic bladder dysfunction (21 men, 24 women; mean age 35 years, age range 18–71 years). The MRU was performed 30 min after intramuscular injection of 20 mg frusemide using heavily T2-weighted fast-spin-echo techniques [axial, thick coronal slab, coronal maximum intensity projection (MIP) images] with fat saturation. The images were reviewed by two observers to determine the presence of filling defects and dilatation of pelvicalyceal system and ureters. The filling defects were classified into central, eccentric and complete. Clinical course and plain films were reviewed to determine significance of the detected filling defects. True filling defects were observed in 5 patients (11%) and all due to stones seen on the plain radiograph of the abdomen. Filling defects artefacts (FDAs) were seen in 23 patients (51%; 17 pelvicalyceal system, 17 upper third of ureters, 7 mid ureters and 1 distal ureter). No stones were seen on the plain radiograph of these patients and they had a favourable clinical course for over 24 months. The true filling defects were large in size, eccentric in position and seen in more than one sequence of the MRU examination (axial, n=5; slab, n=5; and MIP, n=4). Four (80%) of the patients with true defects and 21 (91%) of those with FDAs had dilatation of the pelvicalyceal system and ureters. The FDAs were small in size, centrally placed (74%) and always seen in axial images, rarely in slab images (2 cases) and not seen in MIP images. Artefactual filling defects can be seen in MRU examinations. The cause of the FDAs is not fully explained and could be secondary to turbulent and fast flow of the urine. Some of the FDAs seen in the calyces could be due to the tips of the papillae. Awareness of such defects obviates misinterpretation and prevents unnecessary further investigations or interventions.





Similar content being viewed by others
References
Rothpearl A, Frager D, Subramanian A et al. (1995) MR urography technique and application. Radiology 194:125–130
Tang Y, Yamashita Y, Namimoto et al. (1996) The value of MR urography that uses HASTE sequences to reveal urinary tract disorders. AJR 167:1497–1502
Regan F, Bohlman ME, Khazan R, Rodriguez R, Schultze-Haakh H (1996) MR urography using HASTE imaging in the assessment of ureteric obstruction. AJR 167:1115–1120
Malloy M, Soto J, Yucel EK, Hussain (1997) MR urography: evaluation of a three-dimensional fast spin-echo technique in patients with hydronephrosis. AJR 168:387–392
Roy C, Saussine C, Guth S et al. (1998) MR urography in the evaluation of urinary tract obstruction. Abdom Imaging 23:27–34
Bakker J, de Kort GAP, Lo R et al. (2002) MR urography for the preoperative evaluation of living renal donors. Eur Radiol 12:2021–2029
Louca G, Liberopoulos K, Fidas A, Nikolakopoulou Z, Lykourinas M, Strigaris K (1999) MR urography in the diagnosis of urinary tract obstruction. Eur Urol 35:102–108
Fradin JM, Regan F, Rodriquez R, Moore R (1999) Hydronephrosis in pregnancy: simultaneous depiction of fetal and maternal hydronephrosis by magnetic resonance urography. Urology 53:825–827
Grenier N, Pariente L, Trillaud H, Soussotte C, Douws C (2000) Dilatation of the collecting system during pregnancy: physiologic vs obstructive dilatation. Eur Radiol 10:271–279
Borthne A, Pierre-Jerome C, Nordshus T, Reiseter T (2000) MR urography in children: current status and future development. Eur Radiol 10:503–511
Engine G, Esen T, Rozanes I (2000) MR urography findings of a duplicated ectopic ureter in an adult man. Eur Radiol 10:1253–1256
Maher MM, Prasad TA, Fitzpatrick JM et al. (2000) Spinal dysraphism at MR urography: initial experience. Radiology 216:237–241
Nolte-Ernsting CCA, Adam GB, Gunther RW (2001) MR urography: examination techniques and clinical principles. Eur Radiol 11:335–372
Shipstone DP, Thomas DG, Darwent G, Morcos SK (2002) MR urography in patients with neurogenic bladder dysfunction and spinal dysraphism. Br J Urol 89:658–654
Sudah M, Vanninen R, Partanen K, Heino A, Vainio P, Ala-Opas M (2001) MR urography in evaluation of acute left flank pain: T2-weighted sequences and gadolinium-enhanced three-dimensional FLASH compared with urography. AJR 76:105–112
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Girish, G., Chooi, W.K. & Morcos, S.K. Filling defect artefacts in magnetic resonance urography. Eur Radiol 14, 145–150 (2004). https://doi.org/10.1007/s00330-003-1986-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-003-1986-5