Abstract
This study aimed to study the impact of the COVID-19 pandemic on patients living with systemic vasculitis in Kazakhstan. A single-centre retrospective study of the medical histories of 82 patients was carried out based on the regional clinical hospital of the city for all admissions with systemic vasculitis in the period from January 2019 to December 2021. The following qualitative (gender, disability, concomitant diseases) and quantitative (age, disease experience, laboratory data, etc.) variables were studied. To conduct the study, the criteria for the inclusion and exclusion of patients in the study were determined. According to the results of the study, there is a decrease in the number of hospitalized patients with vasculitis in the rheumatology department of the regional clinical hospital. Compared to 2019, in 2021, the number of hospitalized patients decreased by almost half (Table 1). Out of 82 cases, the most common was Takayasu disease (nonspecific aortoarteritis) (43.9%), IgA-vasculitis (Schenlein-Genoch disease) (31.71%), and they are typical mainly for females of rural origin, who were admitted to the hospital in a comorbid state (p < 0.001). 41.6% of patients have disabilities, and the majority of patients have a II disability group. The average body mass index is 24.2; 27 patients out of the total number of patients suffer from obesity. The most common clinical symptoms of patients with systemic vasculitis were injuries of the musculoskeletal system (75.6%). A negative average correlation was found between the indicators of the level of ESR and haemoglobin, the correlation coefficient is -0.535. The patients had concomitant diseases, such as diabetes mellitus, iron deficiency anaemia, coronary heart disease, hypertension, gastrointestinal tract diseases and hepatitis. Women of reproductive age from rural areas are often diagnosed with systemic vasculitis. A high rate of disability revealed among the patients can be explained by two main factors, the first is that the patients consulted the doctors untimely and the second is that the medical community are insufficiently informed about the management of autoimmune rheumatic diseases, in particular about systemic vasculitis, which hinders timely diagnosis and treatment, respectively. Patients, included in this survey, were mostly suffering from diseases of the musculoskeletal system, but depending on the type of vasculitis, other organs and systems may be affected.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vasculitis is a group of diseases that can lead to various complex disorders of different organs and systems [1]. Systemic vasculitis has complicated, so it is problematic to identify its main causes. A lot of cases are classified as idiopathic vasculitis as the disease could occur due to unknown reasons. Arterial blood vessels could also suffer from vasculitis as well as venous blood vessels, thus affecting not only separate organs but a system or even several systems as well. We could say that in the case of vasculitis, it is necessary to study several different pathophysiological mechanisms and a wide clinical spectrum.
But before studying this illness, it is better to consider some classification issues. A lot of authors are talking about the calibre of blood vessels, classifying them as small, medium or large vessels. However, this classification does not consider the diversity of neighbours of the same calibre, and their specific role in several anatomical areas in response to irritants, stress and recovery, which, in its turn, determine the characteristics of diseases [2, 3]. Vasculitis can be classified based on various indicators, such as the size of the affected vessels, causes, pathogenesis, and their types, as well as clinical signs [4].
The prevalence of systemic vasculitis varies widely depending on geographical areas and different population groups [5]. These changes can be caused by various factors, for example, genetic factors, which manifest themselves in the form of gene polymorphism and changes in the environment (various infections, chemical exposure, ultraviolet radiation, as well as factors related to the seasons) [6,7,8].
The research on systemic vasculitis was carried out using data banks of individual centres in some regions. However, it is not enough to determine the epidemiology of such a widespread group of diseases as vasculitis. High-quality epidemiological studies require a long period, or they could be conducted after analyzing much more cases, but such approach will negatively affect the quality of research [9].
The pathogenesis of systemic vasculitis is still completely unclear, even though a lot of research is being conducted in this area. At the present stage, there are no uniform tests and specific diagnostic criteria for many types of systemic vasculitis, so vasculitis is diagnosed only by the exclusion approach when other cases are excluded. Nevertheless, fast and reliable diagnosis is incredibly important in these conditions, as it allows to start of timely treatment and avoids the progression of insufficiency of various organs and systems with irreversible damage, which often leads to disability [1].
Advances in the field of medical treatment of vasculitis have led to the fact that patients began to live longer, and they have also influenced positively the prognosis of patients' lives [10]. Although in this field, healthcare system has achieved success in the treatment of that nosology, its treatment remains a difficult task, taking into account the delicate balance between the risks of relapse of the disease and the negative consequences of immunosuppressive therapy, primarily serious infections. As a result, the expansion of the use of targeted therapy aimed at reducing dependence on corticosteroids and other nonspecific immunosuppressants has come to the fore [11].
Regretfully, relapses of the disorder occur quite often and chronic circulatory complications are a source of considerable morbidity [12].
Since the beginning of the COVID-19 pandemic, vasculitis-like symptoms and full-blown vasculitis syndromes have been mainly documented in children and adolescents cases [13]. The risk of COVID-19 infection and related complications increases for patients with pre-existing diseases. Patients with chronic rheumatological diseases and vasculitis are at high risk of infection due to underlying immune disorders and the effects of glucocorticosteroids, as well as other immunosuppressive drugs [14]. COVID-19 is a syndrome of SARS-CoV-2, which has the character of a multi-organ lesion and also leads to a violation of the circulatory system. Inflammation of endothelial cells occurs in blood vessels and contributes to some disorders, such as tissue hypoperfusion, damage, thrombosis and vascular disorders at different stages of the disease (acute, subacute and possibly chronic) [15].
Some features of the visualization of lung lesions of such patients may imitate COVID-19. CT images of major background diseases may obscure or erase the signs of COVID-19, especially in the early stages of infection. Therefore, it will be difficult to differentiate superimposed SARS-CoV-2 infection from the main autoimmune lung disease, and interpretation should be based on serological data and clinical conditions.
Nowadays, it is vital to use the patient-oriented treatment approach since it is important to involve patients in joint decision-making to assess short- and long-term risks of the disease, as well as treatment methods. This would help to increase the overall efficiency of medical professionals’ work [11].
Materials and methods
A single-centre retrospective study of the medical histories of 82 patients was carried out based on the data from the city regional clinical hospital. Taking all admissions with systemic vasculitis in the period from January 2019 to December 2021, there were 18 males (22%) and 64 females (78%), p < 0,001. The following qualitative (gender, disability, concomitant diseases) and quantitative (age, disease experience, laboratory data, etc.) variables were considered during the research.
The following criteria were determined to include or exclude the patients in the study:
Inclusion criteria: patients with systemic vasculitis over the age of 18.
Exclusion criteria: patients under the age of 18, with pregnancy, cancer, patients with neurological diseases, mental disorders, intoxication with psychotropic drugs and alcoholism.
The patients were divided into 2 groups, where the first group was on steroid therapy (41 patients) at the time of hospitalization, and the second group of patients did not take steroid drugs (41 patients).
Statistical data processing was carried out using the IBM SPSS Statistics statistical package, version 20. To describe quantitative data, we used the mean (M) ± standard deviation (SD) if the normal distribution was subjected, as well as median (Me) and interquartile range (IQR) were used if the normal distribution was not subjected; nominal qualitative data were described by absolute and relative frequencies (%). The reliability of the differences in values of nominal qualitative data was performed using the Pearson X2 test. The Student t test was used when the data had two independent groups with normal distributions. An analogue of the Student's t test is the Mann–Whitney U Test (Me; IQR). Pearson correlation was used to find the strength and direction of the relationship between two quantitative variables. Regression analysis was carried out to determine linear relationships between two variables.
Results
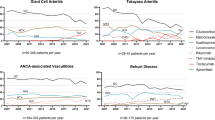
According to the results of the study, there is a decrease in the number of in-door patients with vasculitis in the rheumatology department of the regional clinical hospital: 2019–42 patients (51.2%), 2020–23 (28%), 2021–17 (20.7%) p = 0.002 (Table 1).
Taking 82 cases, Takayasu disease (nonspecific aortoarteritis) is common with patients—36 cases (43.9%), IgA-vasculitis (Schenlein-Genoch disease)–26 cases (31.71%), mainly for females of rural origin who were admitted to hospital in a comorbid state (p < 0.001) (Table 2).
The time from the onset of the disease to the diagnosis of Takayasu's disease (non-specific aorthoarteritis) n = 36 is M = 16.31 (95% CI: 5.15–27.46); IgA-vasculitis (Schenlein-Genoch disease) n = 26—M = 8.96 (95% CI:− 4.02–21.94); Still's disease (systematic necrotic vasculitis) n = 6—M = 5.17 (95%CI:− 0.032–10.66) (Table 3).
Portrait of patients with vasculitis treated in the rheumatology department of the regional clinical hospital: gender—18 male (22%), 64 female (78%) (p < 0.001); place of residence—rural area 55 (67.1%), city 27 (32.9%) (p < 0.001); disability–3 people disabled people, the first group (3.66%), 21 patients with the second disability group (25.61%), 10 patients with the third group (12.2%), 48 patients have no disability (58.4%) and all 82 patients can move independently (Table 4); obesity—the average body mass index is 24.2 (24;6), min = 17, max (37), 19 patients with pre-obesity, 7 patients with the I class and 1 patient with the II class of obesity (Table 5). Their main clinical symptoms were: musculoskeletal system damage (75.6%), gastrointestinal tract damage (57.3%), skin damage (48.8%), peripheral vascular damage (37.8%), cardiovascular system damage (31.7%), arthralgia (50.6%), myalgia (48.2%), lung damage (9.8%), nervous system damage (8.5%), ENT organ damage (7.3%), visual organ damage (4.9%) and endocrine system damage (2.4%) (Table 6).
At the time of admission, 45 patients had elevated ESR (54,9%) p = 0.377, with leukocytosis—15 (18,3%) p < 0,001, with CRP more than 5 mg/l–38 (46.3%) p = 0.508, patients with positive ANA (6 cases), ANCA (5), ASO (7), rheumatoid factor (1), anti-CCP (1), anti-ds DNA (11) and the presence of LE cells (2) p < 0,001.
The average age of patients at the onset of the disease was 30 years, while the average age of patients at the time of examination was 36 years. Therefore, the majority of patients were of reproductive age.
41 patients were on steroid therapy. In the 1 group, the average ESR level was 18.17 (15;20), in the 2 – 23.07 (20;26); the average level of CRP (C-reactive protein) group 1 - 16.07 (5;18), group 2 - 17.76 (7;15); the average haemoglobin level group 1 - 119.54 (121;31), group 2 - 116.90 (23.624) (Table 7).
A negative average correlation was found between the indicators of the level of ESR and haemoglobin, the correlation coefficient is − 0.535 (Table 8).
Concomitant diseases have been reported, including diabetes mellitus, iron deficiency anaemia, coronary heart disease, hypertension, gastrointestinal tract diseases, hepatitis, etc.
Discussion
Takayasu disease is an uncommon inflammatory state that affects the largest blood vessels and involves mostly young patients under the age of 40. The overall epidemiology of the disease is still unidentified [16]. Non-specific systemic symptoms, which are conjugated by no pulse and different types of ischaemic symptoms, should be considered along with deep diagnostic imaging. Timely correct diagnosis and necessary therapy can prevent the patient from risky complications [17].
Takayasu disease was first described in Japan. Although this disease is widespread throughout the world, it was believed by scientists that this disease is more common for people of Asian origin since their cases are mostly reported by those countries. However, this report has not yet been confirmed by high-quality epidemiological studies [16].
Based on data from the 1980s in Japan, the incidence rate in Japan is equal to the incidence rate of the European population, that is, 1–2 per million people per year [18]. Besides, a study, conducted in Norway among representatives of different ethnic backgrounds, revealed a predominance of small groups of people of African (108 per million) and Asian (71 per million) [19].
The best option for determining the origin is to determine the place of birth of all four grandparents of a person, however, this determination is usually impossible, which, in its turn, leads to dependence on the self-assessment of the genealogy. The above-mentioned factors have significantly affected the accuracy of epidemiological studies of systemic vasculitis and must be taken into account when evaluating epidemiological data on these diseases [1].
According to the study, the most common type of systemic vasculitis diagnosed in patients is Takayasu arteritis (43.9%).
The treatment of many autoimmune diseases, in particular systemic vasculitis, is a polysyllabic process. Informing patients about the starting manifestations of this disease and tracking possible side effects plays an important role, since specialists, who follow such an approach, improve the prognosis of the disease thus minimizing the risks of disability and mortality. In the case of systemic vasculitis, multiple organ damage needs a multidisciplinary approach to the course of patients’ treatment [10]. The prognosis of Takayasu disease is most likely getting better with lower lethality rates registered in the last few years, perhaps due to the use of more effective medical therapy in addition to the use of endovascular interventions when required and accessible [20].
There was a high percentage of disability among the patients. Advances in the field of drug treatment of systemic vasculitis have led to much longer life of patients. Nevertheless, a significant proportion of patients with vasculitis continue to be disabled or less productive, secondary to their diagnosis, while indicators of disability and loss of income have barely changed over the past 35 years. Identifying the factors associated with illness and work, which are considered the riskiest as they could lead to work restriction, can help in the development of policies and programs to optimize beneficial working conditions and improve support for patients with vasculitis [10].
Systemic vasculitis is a multisystem disease, which often affects vital organs. And this study proved that vasculitis is a multisystem disease. Depending on the type of vasculitis, various organs and systems were involved in the process. Most often, one of the first manifestations of the disease was a lesion of the musculoskeletal system. There was also a lesion of the gastrointestinal tract, which has a possible connection with the use of long-term Glucocorticosteroids therapy. Depending on the specific type of vasculitis, there were other manifestations of the disease.
The use of immunosuppressive drugs remains the basis for the treatment of systemic vasculitis, although, as in rheumatology in general, the role of genetically engineered biological drugs is increasing in the treatment of systemic vasculitis. More scientific research is necessary to better understand the disease's pathomechanisms and implement new medications and therapy regimens so that disease periods of remission are more prolonged, and treatments more successful, resulting in better life quality for patients [17].
The treatment of autoimmune diseases, in particular systemic vasculitis, is a complex process. By informing patients about the early signs and symptoms of this disease, as well as monitoring possible side effects, specialists increase the likelihood of a favourable outcome, minimizing the risks of disability and mortality. It is quite significant to consider the fact that it is extremely important to start immediate treatment of patients with aggressive diseases. Damage of several organs in the case of systemic vasculitis requires a multidisciplinary approach to the treatment of patients.
According to the results of the study, there is a decrease in the number of admitted patients with vasculitis in the rheumatology department of the regional clinical hospital: 2019–42 patients (51.2%), 2020–23 (28%), 2021–17 (20.7%) p = 0.002. A possible reason for the decrease in the number of patients is the COVID-19 pandemic, which could also affect the quality of life of patients. A survey of a research network focused on patients with vasculitis revealed a high level of concern about COVID-19 in patients with vasculitis. The use of immunosuppression, old age, female gender and concomitant lung diseases affected the level of anxiety. These concerns had a direct impact on avoiding visiting a doctor and conducting laboratory and other tests. An alarming number of patients (10.5%) stopped immunosuppression without consulting their doctor. In addition, temporary discontinuation of rituximab (7.5%) or refusal (13.3%) of further rituximab administration was reported [24].
The incidence of metabolic syndrome (MetS) tends to be increased among patients with rheumatic diseases, and it ranges from 14 to 62.8%. [21] Metabolic syndrome is described by a compound of several cardiovascular risk factors (age, sex, smoking, arterial hypertension, and dyslipidemia) that assume additional cardiovascular morbidity that is more important than the sum of the risk factors related to each component [22]. Scientific studies have presented that atherosclerosis is accelerated in patients with rheumatic diseases, particularly in systemic vasculitis, while the causal reasons have not yet been completely clarified [23].
According to our study, of 82 patients, 27 patients were found to be obese in different forms (pre-obesity, obesity of 1 and 2 classes). There was observed a gain of weight, probably as a side effect of medications such as Glucocorticosteroids. Some studies have shown that patients with ANCA-associated vasculitis often gain weight, especially during the first year after diagnosis. In the cohort of patients included in the study on Wegener's granulomatosis Etanercept (WGET), the authors showed that 22.3% of the total number of patients with granulomatosis with polyangiitis gained at least 10 kg during the first year after diagnosis [25].
Early access of patients to the doctor and awareness of doctors are key factors in verifying the diagnosis. As shown by the results of an international survey that was developed to study the knowledge and perceptions of medical professionals about the diagnosis and treatment of ANCA-associated vasculitis, the perception of systemic vasculitis differs in different countries. This study also revealed the need to update knowledge and awareness of small vessel vasculitis among the entire medical community since its inception [26]. To increase the level of knowledge about systemic vasculitis, which doctors of outpatient services and hospitals of various profiles may encounter in practice, it is necessary to develop educational programs and resources for continuing professional education for doctors with an emphasis on rare autoimmune pathologies, and in particular systemic vasculitis.
Limitations
The study has limitations as it was a retrospective study of a small cohort in one centre, and therefore, our results cannot be generalized without further investigation. However, conducting prospective studies of this rare disease is a difficult task.
Conclusion
Thus, it can be concluded that systemic vasculitis is most often found in women of reproductive age living in rural areas. A high level of disability was observed among patients, and this could be explained by two main factors, the first is the late treatment of patients, and the second is that the medical community is insufficiently informed about the management of systemic vasculitis, which prevents timely diagnosis and treatment, respectively. Although, as a result of our study, the immunological parameters of patients with vasculitis during the pandemic did not differ from the pre-pandemic period, the COVID-19 pandemic had a significant indirect effect on patients with systemic vasculitis. According to our study, patients' access to medical care has almost halved compared to the pre-pandemic period.
The high frequency of systemic vasculitis among rural patients may be due to the significant remoteness of large areas from specialized medical institutions. To eliminate this problem, a comprehensive approach is needed, which includes increasing the level of education of rural residents and raising awareness of primary health care doctors in rural areas about autoimmune rheumatic diseases, in particular systemic vasculitis, telemedicine, etc. The most common case in this study was diseases of the musculoskeletal system, but depending on the type of vasculitis, other organs and systems may be affected, in this regard, the diagnosis and treatment of systemic vasculitis should be interdisciplinary.
High awareness of doctors about autoimmune diseases, early and immediate diagnosis, referral to a rheumatologist and timely treatment are the key to good outcomes in patients and a successful prognosis. Many clinical questions need to be solved in the future, but to answer them, prospective multicenter studies are needed.
Timely detection and proper treatment of vasculitis (newly diagnosed or recurrent disease) remain a priority, and the question of whether or not to change the treatment protocols for systemic vasculitis during COVID-19 remains open.
Data availability
The data that support the finding of this study are available on a reasonable request from the corresponding author.
References
Ralli M, Campo F, Angeletti D, Minni A, Artico M, Greco A, Polimeni A, de Vincentiis M (2020) Pathophysiology and therapy of systemic vasculitides. EXCLI J 18(19):817–854. https://doi.org/10.17179/excli2020-1512
Sunderkötter CH, Zelger B, Chen KR, Requena L, Piette W, Carlson JA, Dutz J, Lamprecht P, Mahr A, Aberer E, Werth VP, Wetter DA, Kawana S, Luqmani R, Frances C, Jorizzo J, Watts JR, Metze D, Caproni M, Alpsoy E, Callen JP, Fiorentino D, Merkel PA, Falk RJ, Jennette JC (2018) Nomenclature of Cutaneous vasculitis: dermatologic addendum to the 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheumatol 70(2):171–184. https://doi.org/10.1002/art.40375
Hoffman GS, Calabrese LH (2014) Vasculitis: determinants of disease patterns. Nat Rev Rheumatol 10(8):454–462. https://doi.org/10.1038/nrrheum.2014.89
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS, Jayne DR, Kallenberg CG, Lamprecht P, Langford CA, Luqmani RA, Mahr AD, Matteson EL, Merkel PA, Ozen S, Pusey CD, Rasmussen N, Rees AJ, Scott DG, Specks U, Stone JH, Takahashi K, Watts RA (2013) 2012 revised international chapel hill consensus conference nomenclature of vasculitides. Arthritis Rheum 65(1):1–11. https://doi.org/10.1002/art.37715
Scott DGI, Watts RA (2013) Epidemiology and clinical features of systemic vasculitis. Clin Exp Nephrol 17(5):607–610. https://doi.org/10.1007/s10157-013-0830-8
Berti A, Dejaco C (2018) Update on the epidemiology, risk factors, and outcomes of systemic vasculitides. Best Pract Res Clin Rheumatol 32(2):271–294. https://doi.org/10.1016/j.berh.2018.09.001
Rubin DI, Schomberg PJ, Shepherd RF, Panneton JM (2001) Arteritis and brachial plexus neuropathy as delayed complications of radiation therapy. Mayo Clin Proc 76(8):849–852. https://doi.org/10.1016/S0025-6196(11)63232-1
Draibe J, Rodó X, Fulladosa X, Martínez-Valenzuela L, Diaz-Encarnación M, Santos L, Marco H, Quintana L, Rodriguez E, Barros X, Garcia R, Balius A, Cruzado JM, Torras J (2018) Seasonal variations in the onset of positive and negative renal ANCA-associated vasculitis in Spain. Clin Kidney J 11(4):468–473. https://doi.org/10.1093/ckj/sfx127
Watts RA, Robson J (2018) Introduction, epidemiology and classification of vasculitis. Best Pract Res Clin Rheumatol 32(1):3–20. https://doi.org/10.1016/j.berh.2018.10.003
Barra L, Borchin RL, Burroughs C, Casey GC, McAlear CA, Sreih AG, Young K, Merkel PA, Pagnoux C (2018) Vasculitis clinical research consortium and the vasculitis patient-powered research network. Impact of vasculitis on employment and income. Clin Exp Rheumatol 111(2):58–64
Almaani S, Fussner LA, Brodsky S, Meara AS, Jayne D (2021) ANCA-associated vasculitis: an update. J Clin Med 10(7):1446. https://doi.org/10.3390/jcm10071446
Pugh D, Karabayas M, Basu N, Cid MC, Goel R, Goodyear CS, Grayson PC, McAdoo SP, Mason JC, Owen C, Weyand CM, Youngstein T, Dhaun N (2022) Large-vessel vasculitis. Nat Rev Dis Primers 7(1):93. https://doi.org/10.1038/s41572-021-00327-5
Colmenero I, Santonja C, Alonso-Riaño M, Noguera-Morel L, Hernández-Martín A, Andina D, Wiesner T, Rodríguez-Peralto JL, Requena L, Torrelo A (2020) SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br J Dermatol 183(4):729–737. https://doi.org/10.1111/bjd.19327
Eslambolchi A, Aghaghazvini L, Gholamrezanezhad A, Kavosi H, Radmard AR (2021) Coronavirus disease 2019 (COVID-19) in patients with systemic autoimmune diseases or vasculitis: radiologic presentation. J Thromb Thrombolysis 51(2):339–348. https://doi.org/10.1007/s11239-020-02289-z
Becker RC (2020) COVID-19-associated vasculitis and vasculopathy. J Thromb Thrombolysis 50(3):499–511. https://doi.org/10.1007/s11239-020-02230-4
Onen F, Akkoc N (2017) Epidemiology of Takayasu arteritis. Presse Med 46(7–8 Pt 2):197–203. https://doi.org/10.1016/j.lpm.2017.05.034
Podgorska D, Podgorski R, Aebisher D, Dabrowski P (2019) Takayasu arteritis - epidemiology, pathogenesis, diagnosis and treatment. J Appl Biomed 17(1):20. https://doi.org/10.32725/jab.2018.005
Koide K (1992) Takayasu arteritis in Japan. Heart Vessels Suppl 7:48–54. https://doi.org/10.1007/BF01744544
Gudbrandsson B, Molberg Ø, Garen T, Palm Ø (2017) Prevalence, incidence, and disease characteristics of takayasu arteritis by ethnic background: data from a large, population-based cohort resident in Southern Norway. Arthritis Care Res (Hoboken) 69(2):278–285. https://doi.org/10.1002/acr.22931
Keser G, Aksu K, Direskeneli H (2018) Takayasu arteritis: an update. Turk J Med Sci 48(4):681–697. https://doi.org/10.3906/sag-1804-136
da Silva TF, Levy-Neto M, Bonfá E, Pereira RM (2013) High prevalence of metabolic syndrome in Takayasu arteritis: increased cardiovascular risk and lower adiponectin serum levels. J Rheumatol 40(11):1897–1904. https://doi.org/10.3899/jrheum.130162
Pereira RM, de Carvalho JF, Bonfá E (2009) Metabolic syndrome in rheumatological diseases. Autoimmun Rev 8(5):415–419. https://doi.org/10.1016/j.autrev.2009.01.001
Tervaert JWC (2013) Cardiovascular disease due to accelerated atherosclerosis in systemic vasculitides. Best Pract Res Clin Rheumatol 27(1):33–44
Banerjee S, George M, Young K, Venkatachalam S, Gordon J, Burroughs C, Curtis D, Ferrada M, Gavigan K, Grayson PC, Kullman J, Danila MI, Curtis JR, Shaw DG, Benjamin Nowell W, Merkel PA (2021) Vasculitis patient-powered research network. Effects of the COVID-19 pandemic on patients living with vasculitis. ACR Open Rheumatol 3(1):17–24. https://doi.org/10.1002/acr2.11204
Wung PK, Anderson T, Fontaine KR, Hoffman GS, Specks U, Merkel PA, Spiera R, Davis JC, St Clair EW, McCune WJ, Stone JH (2008) Effects of glucocorticoids on weight change during the treatment of Wegener’s granulomatosis. Arthritis Rheum 59(5):746–753. https://doi.org/10.1002/art.23561
Auanassova A, Yessirkepov M, Zimba O, Gasparyan AY, Joshi M, Agarwal V, Kitas GD, Ahmed S (2022) Physicians’ perceptions about antineutrophil cytoplasmic antibody-associated vasculitis: an online survey report in the time of the COVID-19 pandemic. Clin Rheumatol 21:1–7. https://doi.org/10.1007/s10067-022-06452-0
Author information
Authors and Affiliations
Contributions
All co-authors contributed substantially to the concept, formulation, searches of relevant articles, and revisions. They approve the final version of the manuscript and take full responsibility for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have stated that there are no conflicts of interest in connection with this article.
Ethical approval
This study was approved by the Local Ethics Committee at South Kazakhstan Medical Academy, protocol N1, 2020.
Informed consent
The requirement for additional written informed consent was waived because of the retrospective design of this study and the use of anonymous patient data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Auanassova, A., Yessirkepov, M. & Zimba, O. The impact of the COVID-19 pandemic on patients with systemic vasculitis: a single-centre retrospective study. Rheumatol Int 43, 459–466 (2023). https://doi.org/10.1007/s00296-023-05276-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-023-05276-8