Abstract
A wide variety of musculoskeletal, arthritic, connective tissue, and vasculitic diseases fall under the umbrella of “rheumatic diseases”. Ankylosing spondylitis, rheumatoid arthritis, and fibromyalgia syndrome are the three members of this disease group with relatively high prevalence. Pharmacological options are at the center of therapeutic algorithms in treating rheumatic diseases, particularly in reducing inflammation. Despite significant advances in pharmacological treatment in recent years, achieving complete treatment success in a group of patients is impossible. Therefore, patients with rheumatic diseases frequently utilize alternative treatment options, such as complementary and alternative medicine. Complementary and alternative medicine is a broad category of health practices not part of the leading health system. Patients with rheumatic diseases turn to complementary and alternative medicine for various reasons, including restricted access to some treatments due to high prices and rigorous regulations, worries about drug side effects, and symptoms that continue despite pharmacological treatment. In addition, because complementary and alternative medicine options are considered natural, they are frequently accepted as well tolerated and have few harmful effects. Ankylosing spondylitis, rheumatoid arthritis, and fibromyalgia syndrome are the primary foci of this comprehensive review. First, we attempted to summarize the non-traditional physical medicine and complementary and alternative medicine options that can be utilized to manage these diseases. Second, we addressed the link between exercise and inflammation in rheumatic diseases. We briefly discussed the possible benefits of exercise-based approaches. In addition, we highlighted the benefits of cooperation between rheumatology and physical medicine-rehabilitation clinics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rheumatic diseases involve various musculoskeletal, arthritic, connective tissue, and vasculitic diseases [1]. Rheumatic diseases are associated with negative effects on daily living activities, a decrease in productivity and work efficiency, certain levels of disability, and deterioration in the quality of life [2]. In recent years, significant progress has been made in the pharmacological treatment of rheumatic diseases. However, some patients do not respond adequately to the main medical treatments. Therefore, patients with rheumatic diseases often choose different treatment options, such as complementary and alternative medicine (CAM) methods [3, 4].
CAM is defined as a wide range of health practices not integrated into the dominant health system [5]. Alternative medical systems, biologics, manipulative interventions, mind–body and cognitive techniques, and energy-based healing procedures are the major categories of CAM methods [6]. There are several reasons why patients with rheumatic diseases resort to CAM methods, such as limited access to some drugs due to high costs and strict regulations, concerns about drug side effects, and symptoms that persist despite medications. Since CAM methods are considered natural, they are often regarded as well tolerated and have minimal adverse events [7].
Exercise interventions have been suggested as an essential component of routine care for those suffering from diseases covering inflammatory arthritis, osteoarthritis, and fibromyalgia syndrome (FMS) [8]. Therefore, exercise and physical medicine practices are essential in managing rheumatic diseases.
This comprehensive review focused on three major rheumatic diseases: ankylosing spondylitis (AS), rheumatoid arthritis (RA), and FMS. We aimed to summarize the non-traditional physical medicine and CAM methods that can be used to manage these diseases. Additionally, we discussed why physical medicine-rehabilitation and rheumatology clinics should collaborate.
Search strategy
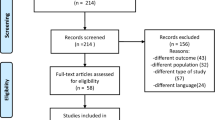
A search procedure was created based on the suggestions of Gasparyan et al. [9]. First, the following term combinations were used to search for articles in Web of Science, Scopus, PubMed/MEDLINE, and DOAJ: ‘Ankylosing Spondylitis and Pilates’ or ‘Ankylosing Spondylitis and Massage’ or ‘Ankylosing Spondylitis and Balneotherapy’ or ‘Ankylosing Spondylitis and Spa Therapy’ or ‘Ankylosing Spondylitis and Yoga’ or ‘Ankylosing Spondylitis and Tai Chi’ or ‘Ankylosing Spondylitis and Acupuncture’ or ‘Ankylosing Spondylitis and Nutritional Therapy’ or ‘Ankylosing Spondylitis and Hypnotherapy’ or ‘Spondyloarthropathy and Pilates’ or ‘Spondyloarthropathy and Massage’ or ‘Spondyloarthropathy and Balneotherapy’ or ‘Spondyloarthropathy and Spa Therapy’ or ‘Spondyloarthropathy and Yoga’ or ‘Spondyloarthropathy and Tai Chi’ or ‘Spondyloarthropathy and Acupuncture’ or ‘Spondyloarthropathy and Nutritional Therapy’ or ‘Spondyloarthropathy and Hypnotherapy’ or ‘Rheumatoid Arthritis and Pilates’ or ‘Rheumatoid Arthritis and Massage’ or ‘Rheumatoid Arthritis and Balneotherapy’ or ‘Rheumatoid Arthritis and Spa Therapy’ or ‘Rheumatoid Arthritis and Yoga’ or ‘Rheumatoid Arthritis and Tai Chi’ or ‘Rheumatoid Arthritis and Acupuncture’ or ‘Rheumatoid Arthritis and Nutritional Therapy’ or ‘Rheumatoid Arthritis and Hypnotherapy’ or ‘Fibromyalgia and Pilates’ or ‘Fibromyalgia and Massage’ or ‘Fibromyalgia and Balneotherapy’ or ‘Fibromyalgia and Spa Therapy’ or ‘Fibromyalgia and Yoga’ or ‘Fibromyalgia and Tai Chi’ or ‘Fibromyalgia and Acupuncture’ or ‘Fibromyalgia and Nutritional Therapy’ or ‘Fibromyalgia and Hypnotherapy'. We only used controlled clinical trials, observational studies, reviews, and English-language papers. Other article types and papers not directly related to the issue were among the exclusion criteria.
Pilates
Pilates is a method of physical training centered on mind–body relaxation, emphasizing regulated movement, posture, and respiration. The main goal is to improve strength and flexibility considerably [10]. Although Pilates programs are primarily aimed at healthy individuals as a component of fitness activities, it has been reported to have beneficial effects on various musculoskeletal system disorders in recent years [11].
A randomized controlled trial in AS patients found that pilates improved physical capacity at a 24-week follow-up [12]. Another randomized controlled trial emphasized the efficacy of pilates as part of a multimodal exercise program in managing AS [13]. Oksuz et al. [14] divided AS patients into two groups and recommended a pilates program combined with aerobic exercise to group 1 and aerobic exercise alone to group 2. It was shown that the combined intervention is more effective regarding functionality and psychosocial status. Although it was revealed that the Pilates program improved respiratory muscle strength in AS patients, it was not superior to conventional exercise [15].
The number of articles evaluating the effectiveness of pilates in RA patients is limited. Yentur et al. [16] divided RA patients into three groups. Pilates was applied to the first group, aerobic exercise to the second group, and a combination of the two to the third group. Participants were followed throughout 8 weeks. In the Pilates group, positive effects were observed on fatigue, quality of life, aerobic capacity, and depression. However, the three groups were not superior to each other. It is difficult to produce precise results due to the short follow-up period and the insufficient sample size.
Altan et al. [17] divided FMS patients into two groups. Pilates was recommended to the first group, and relaxation and stretching exercises were recommended to the second group. Pain and disease activity improved in the Pilates group. In addition, the Pilates group's improvement was superior to the second group. A randomized controlled trial compared mat Pilates with aquatic aerobic exercise. In both groups, alleviation of FMS-related symptoms was detected in the 12-week follow-up. There was no superiority between the two groups [18]. Another randomized controlled trial comparing mat Pilates with aquatic aerobic exercise found that Pilates had a similar effect as aquatic aerobic exercise in FMS patients [19].
Pilates can be considered a different, safe, and potentially effective exercise approach in AS, RA, and FMS management. However, the number of high-quality articles is limited, particularly for RA patients. In addition, the lack of studies on the mechanism of action of Pilates in rheumatic diseases is striking. Therefore, the influences of Pilates on pain mediators, inflammatory indicators, and oxidative stress parameters in patients with AS, RA, and FMS should be evaluated in future studies.
Massage
Massage therapy is one of the oldest methods to reduce pain, relieve muscle spasms and improve quality of life. Massage therapy can be defined as the manipulation and mobilization of soft tissue and joint structures with the help of hands or a hand-held instrument [20]. Various mechanisms have been proposed for the effect of massage on pain, such as gate control theory and increased endorphin levels [21].
The number of articles evaluating the effectiveness of massage in AS patients is limited. In a randomized clinical trial, AS patients were divided into two groups, with one group receiving deep tissue massage and the other receiving therapeutic massage. Both groups reported favorable clinical outcomes [22]. However, the lack of a control group, the small sample size, and the short follow-up period are the article's shortcomings, and the results are difficult to generalize.
A randomized controlled trial evaluated the efficacy of Swedish massage in RA. The patients were divided into two as control and massage groups. After 8 weeks of intervention, the pain level was lower in the massage group, and the need for painkillers was reduced [23]. Another randomized controlled trial separated RA patients into three groups: aromatherapy massage, reflexology, and control. It was stated that massage and reflexology positively affect pain and fatigue [24]. Sevgi Ünal Aslan et al. [25] divided RA patients into Reiki, hand massage, and control groups. The favorable influences of Reiki and hand massage on pain and fatigue were reported.
Toprak Celenay et al. [26] divided FMS patients into two groups. The first group received only exercise, while the second received both exercise and connective tissue massage. Exercise plus connective tissue massage was superior to exercise alone in relieving pain, fatigue, sleep disorder, and role constraints related to physical health. In addition, a meta-analysis of randomized controlled trials demonstrated that more than 5 weeks of massage intervention had beneficial short-term effects on improving pain, anxiety, and depression in FMS patients [27]. A meta-analysis investigating the effectiveness of massage therapy types in FMS stated that most types of massage enhance the quality of life [28].
Massage therapy provides short-term favorable effects, particularly on pain, exhaustion, sleep disturbance, and quality of life indices. However, there has yet to be a consensus on the application technique, duration, and frequency. Furthermore, the methodological shortcomings of existing articles should be considered.
Balneotherapy
Balneotherapy has been employed in treating musculoskeletal disorders and rheumatic diseases since ancient times. Balneotherapy encompasses immersion in baths containing thermal or thermo-mineral water from natural sources and mud and other natural peloid applications [29]. Although the exact mechanism of balneotherapy has not been revealed, possible mechanisms are thermal stimulation, the effect of mineral salt composition in bath applications, and the reflection of mud packs’ physical and chemical properties [30].
A randomized controlled study conducted on AS patients reported that balneotherapy improved disease activity, quality of life, and functionality in the short term. Still, some beneficial effects were lost in mid-term follow-up [31]. Bestaş et al. [32] divided AS patients into three groups and followed up prospectively. Balneotherapy was recommended to the first group, water-based exercises to the second group, and land-based exercises to the third group. It was suggested that all three treatment modalities are effective in disease activity, functionality, quality of life, and mobility and are not superior to each other. In a systematic review, it was emphasized that studies are reporting the beneficial effects of balneotherapy, but studies with large samples and without methodological flaws are needed to provide clear conclusions [33].
The positive effects of balneotherapy on disease activity and functionality were demonstrated in RA patients. On the other hand, it was reported that the effects diminish in long-term follow-up [34, 35]. Spa treatment with saline balneotherapy was found to have an antioxidant effect in RA patients, but the influence on clinical findings is unclear [36]. The beneficial results of balneotherapy sessions were presented by a systematic review analyzing the effects of balneotherapy on the quality of life in RA patients [37]. However, a Cochrane review reported insufficient evidence to reveal balneotherapy's effectiveness in RA patients. In addition, the risk of bias and methodological shortcomings were highlighted [38].
The beneficial effects of balneotherapy on FMS-related symptoms were demonstrated in several studies [39,40,41,42,43]. It was determined that interleukin 1, prostaglandin E2, and leukotriene B4 levels, associated with pain and inflammation, decreased following balneotherapy in FMS patients [44]. In addition, balneotherapy was found to have an antioxidant effect in FMS patients [45]. It was reported that combining balneotherapy with aerobic exercise is more effective than aerobic exercise alone or balneotherapy alone [46]. In a meta-analysis, very low to moderate evidence suggest that balneotherapy can improve pain and quality of life in FMS patients and have a variable effect on tenderness and depression [47].
Yoga
Yoga is a set of practices originating from India and dating back to ancient times, including postural adjustments, breathing exercises techniques, and relaxation approaches. Studies show its positive effects on musculoskeletal disorders [48,49,50]. However, investigations with a high level of evidence evaluating the effectiveness of yoga in AS patients are limited. Combining stretching exercises with proper breathing techniques is part of yoga practice. This condition suggests that yoga may positively affect AS [7]. A randomized controlled trial testing the effectiveness of tele-yoga on AS patients during the COVID-19 era observed improvements in physical function and psychological state [51]. It has been demonstrated that yoga interventions are practicable and acceptable in AS [52].
Badsha et al. [53] assessed the efficiency of an 8-week structured yoga program in RA patients, and significant ameliorations were detected in the patient group (disease activity and global health status) compared to controls. However, there was no similar positive effect on the quality of life. A meta-analysis published in 2020 evaluated yoga's effectiveness in RA patients. The results supported that yoga may positively affect physical function, disease activity, and grip strength. However, there was no improvement in pain level, markers of inflammation, and the number of tender joints [54]. A randomized controlled trial was conducted to assess the efficacy of the Yoga daily life program in RA patients. Although it did not affect the quality of life, fatigue and psychological state benefits were reported [55].
The efficacy of an 8-week structured yoga program on FMS syndrome was investigated in a randomized controlled trial and found improvement in pain, psychological state, and fatigue [56]. In addition, a meta-analysis of the efficacy and safety of meditative treatment options in FMS revealed that yoga was beneficial and a safe practice on the main clinical signs of FMS [57].
Yoga seems to be an effective treatment option for various clinical manifestations of rheumatic diseases. However, inadequacy in sample sizes, methodological flaws, and risk of bias draw attention to yoga studies. Therefore, articles with a higher level of evidence are needed [58].
Tai Chi
Tai Chi is a traditional Chinese meditative practice that dates back to ancient times. It integrates deep diaphragmatic breathing and relaxation techniques with a series of gentle and controlled basic postures. Its goal is to unify the physical, psychological, social, and behavioral components and to increase inner harmony by strengthening and stretching the soft tissues [59]. In a controlled clinical study conducted on AS patients, an 8-week Tai Chi program was reported to impact disease activity and flexibility positively [60]. Patients with AS were divided into two groups in a randomized controlled clinical trial. One group was given a home exercise program, whereas the other group received Tai Chi movements in addition to the home exercise program. Although both groups reported positive outcomes, the Tai Chi group experienced more significant improvements in disease activity and quality of life [61].
Uhlig et al. [62] assessed the efficacy of Tai Chi in RA patients quantitatively and qualitatively. At the end of the 12-week follow-up period, improvements in lower extremity muscle function, physical performance, pain, and balance were observed. Shin et al. [63] evaluated the impact of Tai Chi on endothelial function and arterial stiffness in RA patients. After the program, assessments for endothelial function and arterial stiffness were substantially better in the Tai Chi group. No considerable differences were detected between the intervention and control groups in disease activity and disability parameters. A Cochrane review published in 2019 emphasized that Tai Chi's effect on RA is unclear. Due to the low level of evidence, a critical impact cannot be confirmed or excluded [64].
In a randomized controlled trial investigating the efficacy of a 12-week classical Tai Chi program on FMS patients, the intervention group showed more significant improvement in disease activity and quality of life indicators. In addition, well-being continued at the 24-week evaluation [65]. A randomized controlled study comparing the effects of Tai Chi and aerobic exercise in FMS patients found that Tai Chi had a similar impact with aerobic exercise and was even superior in some parameters [66]. A meta-analysis reported that Tai Chi is more beneficial than standard care in FMS. Furthermore, this meta-analysis emphasized that studies with a higher level of evidence are needed to recommend Tai Chi as an alternative to established treatment options such as aerobic exercise [67]. Another randomized controlled trial suggested that Tai Chi improved sympathovagal balance in FMS [68].
This low-cost and efficient symptom management option is a promising method that can be incorporated into the treatment strategies of patients with AS, RA, and FMS. However, multicenter, large sample and high-evidence studies are required.
Acupuncture
Acupuncture is a treatment modality used for over four thousand years in China and is considered an essential component of traditional Chinese medicine. Thin needles are implanted at certain places on the body for treatment, and a manipulation technique is performed. Acupuncture treatment aims to relieve symptoms and improve well-being by stimulating meridians and acupuncture points and involves many different application techniques [69, 70].
A combination of needling, moxibustion, and other traditional Chinese medicine procedures is frequently used to gain greater efficacy in AS patients. In warm acupuncture, acupuncture and moxibustion are used together [71]. The meta-analysis by Xuan et al. [72] aimed to evaluate the effectiveness of needling alone in AS patients. Although beneficial results were reported in this meta-analysis, which included randomized controlled trials, emphasis was placed on methodological shortcomings and low quality of evidence.
The authors argued in a systematic review that acupuncture, alone or in conjunction with other modalities, is helpful for clinical signs of RA, has no notable adverse effects, and can enhance the functional status and quality of life. It was suggested that there could be several underlying mechanisms, including anti-inflammatory effects, antioxidative alterations, and regulation of immune system function [73]. In their meta-analysis, Lu et al. [74] found that acupuncture improved clinical signs and laboratory parameters in RA patients. However, some articles did not report favorable effects [75, 76]. This condition suggests that the efficacy of acupuncture in RA patients should be confirmed by research with high methodological quality and large samples.
In a meta-analysis evaluating the effectiveness of acupuncture in FMS patients, a considerable favorable effect was found in reducing pain and maintaining well-being [77]. Kim et al. [78] supported these findings in their meta-analysis. Zheng et al. [79] reported moderate evidence of acupuncture's effectiveness on FMS-related pain, but found no effect on fatigue, stiffness, sleep quality, and physical function. A Cochrane review evaluating the efficacy of acupuncture on FMS reported low to moderate evidence that acupuncture improves pain and stiffness compared to standard therapy. Furthermore, moderate evidence was presented that there was no difference between sham acupuncture and therapeutic acupuncture in pain, sleep, stiffness, and well-being [80].
Nutritional therapy
In recent years, there has been a surge of interest in the association between nutrition and gut microbiome, as well as inflammation and oxidative stress in rheumatic diseases. A systematic review emphasized that the evidence for a link between diet and AS was extremely limited due to the poor sample size, bias risk, and inadequate data reporting in most of the enrolled studies [81]. Some articles support the potential relationship between diet and oxidative stress in AS patients and suggest that positive effects can be obtained on disease activity by increasing adherence to the Mediterranean diet [82, 83].
Schonenberger et al. [84] investigated the effectiveness of anti-inflammatory diets (Mediterranean, vegetarian, vegan, ketogenic) in RA patients in a systematic review and reported positive results on pain. However, there was an emphasis on the high risk of bias and low level of evidence. Some studies showed curcumin supplementation improves inflammatory markers in RA patients [85, 86]. Probiotic supplementation may have benefits on CRP and RA activity, according to a meta-analysis assessing the effect of probiotics on RA. However, the level of evidence is low, and heterogeneity is evident [87]. There was insufficient evidence to support collagen supplementation in RA [88].
In a systematic review analyzing the effect of several types of diets on FMS, the results for nutritional therapy were considered to be but contentious promising. The emphasis was on poor methodological quality for articles on this topic [89]. Another systematic review investigating the impact of vegan and vegetarian diets on FMS found positive and promising results on pain, sleep, and quality of life. Still, it noted the low methodological quality [90]. A randomized controlled clinical trial evaluated the efficacy of tryptophan and magnesium-enriched Mediterranean diet and found beneficial effects on anxiety, mood status, and eating disorder. However, no impact on sleep quality was detected [91].
There are promising results that various dietary interventions can be beneficial for AS, RA, and FMS. However, it is challenging to recommend a uniform diet. The methodological quality of the studies in the literature is poor, and the bias risk is remarkable. Studies with higher methodological quality and larger samples are needed in this area.
Hypnotherapy
There is inadequate data to assess the efficacy of hypnotherapy in AS. Horton-Hausknecht et al. [92] evaluated the effectiveness of hypnosis therapy in RA patients. Although hypnosis therapy was observed to positively impact objective and subjective findings, the results should be interpreted with caution. First, the sample size is limited. In the article, three groups were formed hypnotherapy, relaxation, and control. There was a statistically significant difference between the three groups regarding age, education level, and disease duration.
Bernardy et al. [93] conducted a systematic review and meta-analysis evaluating the efficacy of hypnotherapy in FMS. Unfortunately, the evidence for the effectiveness of hypnotherapy in reducing pain at the end of therapy was not robust against methodological bias risks. Furthermore, it was linked with poor methodological research quality. Nevertheless, a randomized controlled trial evaluating hypnosis therapy in FMS patients found improvement in pain, fatigue, and depression [94]. Another systematic review supported using a combination of hypnotherapy and cognitive behavioral therapy to manage FMS core symptoms. However, it was presented with a low level of evidence that hypnotherapy effectively reduces pain and improves psychological state [95].
Physical medicine-rehabilitation and rheumatology clinics collaboration
Pharmacological interventions are at the center of the treatment of rheumatic diseases. Unfortunately, despite the significant advances of recent years, it is still not possible to achieve favorable outcomes for all patients. Therefore, it is preferable not to rely solely on pharmaceutical treatment alternatives. Exercise is essential to preserving and improving general health and quality of life, not only in rheumatic diseases but also in many other diseases and even in healthy people. Furthermore, it is impossible to discontinue exercise practices to treat rheumatic diseases such as AS, FMS, and osteoarthritis. Therefore, it is appropriate to implement individualized exercise programs or recommend home programs in physical medicine and rehabilitation clinics after gathering necessary information about the patient's medical condition from the rheumatology clinic and physician while adhering to the principles of FITT. In addition, some patients with rheumatic diseases may require individualized rehabilitation applications and orthotics–prosthesis recommendations due to contracture, respiratory–cardiac function impairment, and gait disruption. Rheumatologists can obtain views regarding CAM applications from physical medicine and rehabilitation clinics for patients they deem appropriate. Given all of these considerations, it is evident that physical medicine—rehabilitation, and rheumatology clinics should be in constant communication and collaborate as needed. Due to the predominant involvement of the musculoskeletal system, exercise, rehabilitation interventions, and CAM applications should be positioned appropriately within the treatment programs for rheumatic diseases.
Conclusion, limitations, and future suggestions
Physical medicine and CAM methods are safe approaches to managing AS, RA, and FMS. Although favorable results have been reported, the level of evidence for many CAM methods is low. The main reasons for this outcome are methodological flaws such as limited sample size, bias risk, short follow-up periods, and challenges in creating control groups. Another issue is that there is no agreement in CAM approaches on the frequency of interventions and the number of sessions. This situation causes heterogeneity in systematic reviews and meta-analyses. To overcome these obstacles, researchers should focus on studies that reduce methodological flaws. Furthermore, researchers should concentrate on the mechanisms of action of these approaches and attempt to understand the biological basis for their impacts on inflammation and pain. Although pharmacological treatments are at the core of managing AS, RA, and FMS, exercise-based interventions and CAM methods should be placed in appropriate positions within the treatment programs.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Phang JK, Kwan YH, Goh H, Tan VIC, Thumboo J, Østbye T, Fong W (2018) Complementary and alternative medicine for rheumatic diseases: a systematic review of randomized controlled trials. Complement Ther Med 37:143–157. https://doi.org/10.1016/j.ctim.2018.03.003
Sangha O (200) Epidemiology of rheumatic diseases. Rheumatology (Oxford) 39(Suppl 2):3–12. https://doi.org/10.1093/rheumatology/39.suppl_2.3
Klingberg E, Wallerstedt SM, Torstenson T, Håwi G, Forsblad-d’Elia H (2009) The use of complementary and alternative medicine in outpatients with inflammatory rheumatic diseases in Sweden. Scand J Rheumatol 38:472–480. https://doi.org/10.3109/03009740902994280
Breuer GS, Orbach H, Elkayam O, Berkun Y, Paran D, Mates M, Nesher G (2006) Use of complementary and alternative medicine among patients attending rheumatology clinics in Israel. Isr Med Assoc J 8:184–187
James PB, Wardle J, Steel A, Adams J (2018) Traditional, complementary and alternative medicine use in Sub-Saharan Africa: a systematic review. BMJ Glob Health 3:e000895. https://doi.org/10.1136/bmjgh-2018-000895
Barnes PM, Powell-Griner E, McFann K, Nahin RL (2004) Complementary and alternative medicine use among adults: United States, 2002. Adv Data 343:1–19
Danve A, Deodhar AA (2018) Complementary medicine for axial spondyloarthritis: is there any scientific evidence? Curr Opin Rheumatol 30:310–318. https://doi.org/10.1097/BOR.0000000000000513
Kelley GA (2022) Precision exercise medicine in rheumatology: don’t put the cart before the horse. Clin Rheumatol 41:2277–2279. https://doi.org/10.1007/s10067-022-06260-6
Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD (2011) Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int 31:1409–1417. https://doi.org/10.1007/s00296-011-1999-3
Kamioka H, Tsutani K, Katsumata Y, Yoshizaki T, Okuizumi H, Okada S, Park SJ, Kitayuguchi J, Abe T, Mutoh Y (2016) Effectiveness of Pilates exercise: a quality evaluation and summary of systematic reviews based on randomized controlled trials. Complement Ther Med 25:1–19. https://doi.org/10.1016/j.ctim.2015.12.018
Cruz JC, Liberali R, Cruz TMFD, Netto MIA (2016) The Pilates method in the rehabilitation of musculoskeletal disorders: a systematic review. Fisioterapia Movimento 29:609–622. https://doi.org/10.1590/1980-5918.029.003.AO19
Altan L, Korkmaz N, Dizdar M, Yurtkuran M (2012) Effect of Pilates training on people with ankylosing spondylitis. Rheumatol Int 32:2093–2099. https://doi.org/10.1007/s00296-011-1932-9
Roşu MO, Ţopa I, Chirieac R, Ancuta C (2014) Effects of Pilates, McKenzie and Heckscher training on disease activity, spinal motility and pulmonary function in patients with ankylosing spondylitis: a randomized controlled trial. Rheumatol Int 34:367–372. https://doi.org/10.1007/s00296-013-2869-y
Oksüz S, Unal E (2021) Comparison of the effects of aerobic training alone versus aerobic training combined with clinical Pilates exercises on the functional and psychosocial status of patients with ankylosing spondylitis: a randomized controlled trial. Physiother Theory Pract 18:1–11. https://doi.org/10.1080/09593985.2021.2005199
BağlanYentür S, Saraç DC, Sari F, Tore G, Bilici Salman R, AkifÖztürk M, Oskay D (2022) The effects of Pilates training on respiratory muscle strength in patients with ankylosing spondylitis. Physiother Theory Pract 8:1–11. https://doi.org/10.1080/09593985.2022.2109540
Yentür SB, Ataş N, Öztürk MA, Oskay D (2021) Comparison of the effectiveness of pilates exercises, aerobic exercises, and pilates with aerobic exercises in patients with rheumatoid arthritis. Ir J Med Sci 190:1027–1034. https://doi.org/10.1007/s11845-020-02412-2
Altan L, Korkmaz N, Bingol U, Gunay B (2009) Effect of pilates training on people with fibromyalgia syndrome: a pilot study. Arch Phys Med Rehabil 90:1983–1988. https://doi.org/10.1016/j.apmr.2009.06.021
de Medeiros SA, de Almeida Silva HJ, do Nascimento RM, da Silva Maia JB, de Almeida Lins CA, de Souza MC (2020) Mat Pilates is as effective as aquatic aerobic exercise in treating women with fibromyalgia: a clinical, randomized and blind trial. Adv Rheumatol 60:21. https://doi.org/10.1186/s42358-020-0124-2
Silva HJA, Lins CAA, Nobre TTX, de Sousa VPS, Caldas RTJ, de Souza MC (2019) Mat Pilates and aquatic aerobic exercises for women with fibromyalgia: a protocol for a randomised controlled blind study. BMJ Open 9:e022306. https://doi.org/10.1136/bmjopen-2018-022306
Koçyiğit BF, Akyol A, Usgu S (2021) Role of manual therapy and massage in the treatment of fibromyalgia: testing the hypothesis. Cent Asian J Med Hypotheses Ethics 2:182–189. https://doi.org/10.47316/cajmhe.2021.2.4.01
Miake-Lye IM, Mak S, Lee J, Luger T, Taylor SL, Shanman R, Beroes-Severin JM, Shekelle PG (2019) Massage for pain: an evidence map. J Altern Complement Med 25:475–502. https://doi.org/10.1089/acm.2018.0282
Romanowski MW, Špiritović M, Rutkowski R, Dudek A, Samborski W, Straburzyńska-Lupa A (2017) Comparison of deep tissue massage and therapeutic massage for lower back pain, disease activity, and functional capacity of ankylosing spondylitis patients: a randomized clinical pilot study. Evid Based Complement Alternat Med 2017:9894128. https://doi.org/10.1155/2017/9894128
Sahraei F, Rahemi Z, Sadat Z, Zamani B, Ajorpaz NM, Afshar M, Mianehsaz E (2022) The effect of Swedish massage on pain in rheumatoid arthritis patients: a randomized controlled trial. Complement Ther Clin Pract 46:101524. https://doi.org/10.1016/j.ctcp.2021.101524
GokMetin Z, Ozdemir L (2016) The effects of aromatherapy massage and reflexology on pain and fatigue in patients with rheumatoid arthritis: a randomized controlled trial. Pain Manag Nurs 17:140–149. https://doi.org/10.1016/j.pmn.2016.01.004
SevgiÜnal Aslan K, Çetinkaya F (2022) The effects of Reiki and hand massage on pain and fatigue in patients with rheumatoid arthritis. Explore (NY). https://doi.org/10.1016/j.explore.2022.06.006
ToprakCelenay S, AnaforogluKulunkoglu B, Yasa ME, SahbazPirincci C, Un Yildirim N, Kucuksahin O, Ugurlu FG, Akkus S (2017) A comparison of the effects of exercises plus connective tissue massage to exercises alone in women with fibromyalgia syndrome: a randomized controlled trial. Rheumatol Int 37:1799–1806. https://doi.org/10.1007/s00296-017-3805-3
Li YH, Wang FY, Feng CQ, Yang XF, Sun YH (2014) Massage therapy for fibromyalgia: a systematic review and meta-analysis of randomized controlled trials. PLoS ONE 9:e89304. https://doi.org/10.1371/journal.pone.0089304
Yuan SL, Matsutani LA, Marques AP (2015) Effectiveness of different styles of massage therapy in fibromyalgia: a systematic review and meta-analysis. Man Ther 20:257–264. https://doi.org/10.1016/j.math.2014.09.003
Gutenbrunner C, Bender T, Cantista P, Karagülle Z (2010) A proposal for a worldwide definition of health resort medicine, balneology, medical hydrology and climatology. Int J Biometeorol 54:495–507. https://doi.org/10.1007/s00484-010-0321-5
Cozzi F, Ciprian L, Carrara M, Galozzi P, Zanatta E, Scanu A, Sfriso P, Punzi L (2018) Balneotherapy in chronic inflammatory rheumatic diseases-a narrative review. Int J Biometeorol 62:2065–2071. https://doi.org/10.1007/s00484-018-1618-z
Altan L, Bingöl U, Aslan M, Yurtkuran M (2006) The effect of balneotherapy on patients with ankylosing spondylitis. Scand J Rheumatol 35:283–289. https://doi.org/10.1080/03009740500428806
Bestaş E, Dündar Ü, Köken T, Koca B, Yeşil H (2021) The comparison of effects of balneotherapy, water-based and land-based exercises on disease activity, symptoms, sleep quality, quality of life and serum sclerostin level in patients with ankylosing spondylitis: a prospective, randomized study. Arch Rheumatol 37:159–168. https://doi.org/10.46497/ArchRheumatol.2022.9024
Forestier R, Bugnard A, Thomas T (2022) Balneotherapy in spondyloarthropathy: a systematic review. Therapie. https://doi.org/10.1016/j.therap.2022.02.006
Karagülle M, Kardeş S, Dişçi R, Karagülle MZ (2018) Spa therapy adjunct to pharmacotherapy is beneficial in rheumatoid arthritis: a crossover randomized controlled trial. Int J Biometeorol 62:195–205. https://doi.org/10.1007/s00484-017-1441-y
Karagülle M, Kardeş S, Karagülle MZ (2018) Long-term efficacy of spa therapy in patients with rheumatoid arthritis. Rheumatol Int 38:353–362. https://doi.org/10.1007/s00296-017-3926-8
Karagülle M, Kardeş S, Karagülle O, Dişçi R, Avcı A, Durak İ, Karagülle MZ (2017) Effect of spa therapy with saline balneotherapy on oxidant/antioxidant status in patients with rheumatoid arthritis: a single-blind randomized controlled trial. Int J Biometeorol 61:169–180. https://doi.org/10.1007/s00484-016-1201-4
Fernandez-Gonzalez M, Fernandez-Lao C, Martin-Martin L, Gonzalez-Santos A, Lopez-Garzon M, Ortiz-Comino L, Lozano-Lozano M (2021) Therapeutic benefits of balneotherapy on quality of life of patients with rheumatoid arthritis: a systematic review. Int J Environ Res Public Health 18:13216. https://doi.org/10.3390/ijerph182413216
Verhagen AP, Bierma-Zeinstra SM, Boers M, Cardoso JR, Lambeck J, de Bie R, de Vet HC (2015) Balneotherapy (or spa therapy) for rheumatoid arthritis. Cochrane Database Syst Rev 2015:CD000518. https://doi.org/10.1002/14651858.CD000518.pub2
Evcik D, Kizilay B, Gökçen E (2002) The effects of balneotherapy on fibromyalgia patients. Rheumatol Int 22:56–59. https://doi.org/10.1007/s00296-002-0189-8
Buskila D, Abu-Shakra M, Neumann L, Odes L, Shneider E, Flusser D, Sukenik S (2001) Balneotherapy for fibromyalgia at the Dead Sea. Rheumatol Int 20:105–108. https://doi.org/10.1007/s002960000085
Dönmez A, Karagülle MZ, Tercan N, Dinler M, Işsever H, Karagülle M, Turan M (2005) SPA therapy in fibromyalgia: a randomised controlled clinic study. Rheumatol Int 26:168–172. https://doi.org/10.1007/s00296-005-0623-9
Ozkurt S, Dönmez A, ZekiKaragülle M, Uzunoğlu E, Turan M, Erdoğan N (2012) Balneotherapy in fibromyalgia: a single blind randomized controlled clinical study. Rheumatol Int 32:1949–1954. https://doi.org/10.1007/s00296-011-1888-9
Fioravanti A, Manica P, Bortolotti R, Cevenini G, Tenti S, Paolazzi G (2018) Is balneotherapy effective for fibromyalgia? Results from a 6-month double-blind randomized clinical trial. Clin Rheumatol 37:2203–2212. https://doi.org/10.1007/s10067-018-4117-z
Ardiç F, Ozgen M, Aybek H, Rota S, Cubukçu D, Gökgöz A (2007) Effects of balneotherapy on serum IL-1, PGE2 and LTB4 levels in fibromyalgia patients. Rheumatol Int 27:441–446. https://doi.org/10.1007/s00296-006-0237-x
Çetinkaya FN, Koçak FA, Kurt EE, Güçlü K, Tuncay F, Şaş S, Erdem HR (2020) The effects of balneotherapy on oxidant/antioxidant status in patients with fibromyalgia: an observational study. Arch Rheumatol 35:506–514. https://doi.org/10.46497/ArchRheumatol.2020.7857
Kurt EE, Koçak FA, Erdem HR, Tuncay F, Kelez F (2016) Which non-pharmacological treatment is more effective on clinical parameters in patients with fibromyalgia: balneotherapy or aerobic exercise? Arch Rheumatol 31:162–169. https://doi.org/10.5606/ArchRheumatol.2016.5751
Cao CF, Ma KL, Li QL, Luan FJ, Wang QB, Zhang MH, Viswanath O, Myrcik D, Varrassi G, Wang HQ (2021) Balneotherapy for fibromyalgia syndrome: a systematic review and meta-analysis. J Clin Med 10:1493. https://doi.org/10.3390/jcm10071493
Cramer H, Klose P, Brinkhaus B, Michalsen A, Dobos G (2017) Effects of yoga on chronic neck pain: a systematic review and meta-analysis. Clin Rehabil 31:1457–1465. https://doi.org/10.1177/0269215517698735
Tilbrook HE, Cox H, Hewitt CE, Kang’ombe AR, Chuang LH, Jayakody S, Aplin JD, Semlyen A, Trewhela A, Watt I, Torgerson DJ (2011) Yoga for chronic low back pain: a randomized trial. Ann Intern Med 155:569–578. https://doi.org/10.7326/0003-4819-155-9-201111010-00003
Cheung C, Wyman JF, Resnick B, Savik K (2014) Yoga for managing knee osteoarthritis in older women: a pilot randomized controlled trial. BMC Complement Altern Med 14:160. https://doi.org/10.1186/1472-6882-14-160
Singh J, Jha M, Metri K, Mohanty S, Singh A, Tekur P (2021) A study protocol for a randomised controlled trial on the efficacy of yoga as an adjuvant therapy for patients with Ankylosing spondylitis amidst COVID-19 pandemic. Adv Integr Med. https://doi.org/10.1016/j.aimed.2021.11.001
Singh J, Metri K, Tekur P, Mohanty S, Jha M, Singh A, Raghuram N (2022) Designing, validation, and feasibility of a yoga module for patients with ankylosing spondylitis. J Ayurveda Integr Med 13:100479. https://doi.org/10.1016/j.jaim.2021.06.019
Badsha H, Chhabra V, Leibman C, Mofti A, Kong KO (2009) The benefits of yoga for rheumatoid arthritis: results of a preliminary, structured 8-week program. Rheumatol Int 29:1417–1421. https://doi.org/10.1007/s00296-009-0871-1
Ye X, Chen Z, Shen Z, Chen G, Xu X (2020) Yoga for treating rheumatoid arthritis: a systematic review and meta-analysis. Front Med (Lausanne) 7:586665. https://doi.org/10.3389/fmed.2020.586665
Pukšić S, Mitrović J, Čulo MI, Živković M, Orehovec B, Bobek D, Morović-Vergles J (2021) Effects of yoga in daily life program in rheumatoid arthritis: a randomized controlled trial. Complement Ther Med 57:102639. https://doi.org/10.1016/j.ctim.2020.102639.
Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD (2010) A pilot randomized controlled trial of the Yoga of awareness program in the management of fibromyalgia. Pain 151:530–539. https://doi.org/10.1016/j.pain.2010.08.020
Langhorst J, Klose P, Dobos GJ, Bernardy K, Häuser W (2013) Efficacy and safety of meditative movement therapies in fibromyalgia syndrome: a systematic review and meta-analysis of randomized controlled trials. Rheumatol Int 33:193–207. https://doi.org/10.1007/s00296-012-2360-1
de Orleans Casagrande P, Coimbra DR, de Souza LC, Andrade A (2022) Effects of yoga on depressive symptoms, anxiety, sleep quality, and mood in patients with rheumatic diseases: systematic review and meta-analysis. PM R. https://doi.org/10.1002/pmrj.12867
Wang C (2011) Tai chi and rheumatic diseases. Rheum Dis Clin North Am 37:19–32. https://doi.org/10.1016/j.rdc.2010.11.002
Lee EN, Kim YH, Chung WT, Lee MS (2008) Tai chi for disease activity and flexibility in patients with ankylosing spondylitis—a controlled clinical trial. Evid Based Complement Alternat Med 5:457–462. https://doi.org/10.1093/ecam/nem048
Cetin SY, Calik BB, Ayan A, Kabul EG (2020) The effectiveness of 10-Tai Chi movements in patients with ankylosing spondylitis receiving anti-tumor necrosis factor α therapy: a randomized controlled trial. Eur J Integr Med 39:101208. https://doi.org/10.1016/j.eujim.2020.101208
Uhlig T, Fongen C, Steen E, Christie A, Ødegård S (2010) Exploring Tai Chi in rheumatoid arthritis: a quantitative and qualitative study. BMC Musculoskelet Disord 11:43. https://doi.org/10.1186/1471-2474-11-43
Shin JH, Lee Y, Kim SG, Choi BY, Lee HS, Bang SY (2015) The beneficial effects of Tai Chi exercise on endothelial function and arterial stiffness in elderly women with rheumatoid arthritis. Arthritis Res Ther 17:380. https://doi.org/10.1186/s13075-015-0893-x
Mudano AS, Tugwell P, Wells GA, Singh JA (2019) Tai Chi for rheumatoid arthritis. Cochrane Database Syst Rev 9:CD004849. https://doi.org/10.1002/14651858.CD004849.pub2
Wang C, Schmid CH, Rones R, Kalish R, Yinh J, Goldenberg DL, Lee Y, McAlindon T (2010) A randomized trial of tai chi for fibromyalgia. N Engl J Med 363:743–754. https://doi.org/10.1056/NEJMoa0912611
Wang C, Schmid CH, Fielding RA, Harvey WF, Reid KF, Price LL, Driban JB, Kalish R, Rones R, McAlindon T (2018) Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. BMJ 360:k851. https://doi.org/10.1136/bmj.k851
Cheng CA, Chiu YW, Wu D, Kuan YC, Chen SN, Tam KW (2019) Effectiveness of Tai Chi on fibromyalgia patients: a meta-analysis of randomized controlled trials. Complement Ther Med 46:1–8. https://doi.org/10.1016/j.ctim.2019.07.007
Wong A, Figueroa A, Sanchez-Gonzalez MA, Son WM, Chernykh O, Park SY (2018) Effectiveness of Tai Chi on cardiac autonomic function and symptomatology in women with Fibromyalgia: a randomized controlled trial. J Aging Phys Act 26:214–221. https://doi.org/10.1123/japa.2017-0038
Chon TY, Lee MC (2013) Acupuncture. Mayo Clin Proc 88:1141–1146. https://doi.org/10.1016/j.mayocp.2013.06.009
Chang Y, Wu N, Zhang Z, Zhang Z, Ren B, Liu F, Song X, Wu M, Feng X, Yin S (2022) Efficacy of manual acupuncture, electro-acupuncture, and warm acupuncture for knee osteoarthritis: study protocol for a randomized controlled trial. Trials 23:700. https://doi.org/10.1186/s13063-022-06653-7
Dang S, Ren Y, Zhao B, Meng X, Wang C, Han X, Liu Y, Zhang C (2021) Efficacy and safety of warm acupuncture in the treatment of ankylosing spondylitis: a protocol for systematic review and meta-analysis. Medicine (Baltimore) 100:e24116. https://doi.org/10.1097/MD.0000000000024116
Xuan Y, Huang H, Huang Y, Liu D, Hu X, Geng L (2020) The efficacy and safety of simple-needling therapy for treating ankylosing spondylitis: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med 2020:4276380. https://doi.org/10.1155/2020/4276380
Chou PC, Chu HY (2018) Clinical efficacy of acupuncture on rheumatoid arthritis and associated mechanisms: a systemic review. Evid Based Complement Alternat Med 2018:8596918. https://doi.org/10.1155/2018/8596918
Lu HL, Chang CM, Hsieh PC, Wang JC, Kung YY (2022) The effects of acupuncture and related techniques on patients with rheumatoid arthritis: a systematic review and meta-analysis. J Chin Med Assoc 85:388–400. https://doi.org/10.1097/JCMA.0000000000000659
Lee MS, Shin BC, Ernst E (2008) Acupuncture for rheumatoid arthritis: a systematic review. Rheumatology (Oxford) 47:1747–1753. https://doi.org/10.1093/rheumatology/ken330
David J, Townsend S, Sathanathan R, Kriss S, Doré CJ (1999) The effect of acupuncture on patients with rheumatoid arthritis: a randomized, placebo-controlled cross-over study. Rheumatology (Oxford) 38:864–869. https://doi.org/10.1093/rheumatology/38.9.864
Zhang XC, Chen H, Xu WT, Song YY, Gu YH, Ni GX (2019) Acupuncture therapy for fibromyalgia: a systematic review and meta-analysis of randomized controlled trials. J Pain Res 12:527–542. https://doi.org/10.2147/JPR.S186227
Kim J, Kim SR, Lee H, Nam DH (2019) Comparing verum and sham acupuncture in fibromyalgia syndrome: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2019:8757685. https://doi.org/10.1155/2019/8757685
Zheng C, Zhou T (2022) Effect of acupuncture on pain, fatigue, sleep, physical function, stiffness, well-being, and safety in fibromyalgia: a systematic review and meta-analysis. J Pain Res 15:315–329. https://doi.org/10.2147/JPR.S351320
Deare JC, Zheng Z, Xue CC, Liu JP, Shang J, Scott SW, Littlejohn G (2013) Acupuncture for treating fibromyalgia. Cochrane Database Syst Rev 2013:CD007070. https://doi.org/10.1002/14651858
Macfarlane TV, Abbood HM, Pathan E, Gordon K, Hinz J, Macfarlane GJ (2018) Relationship between diet and ankylosing spondylitis: a systematic review. Eur J Rheumatol 5:45–52. https://doi.org/10.5152/eurjrheum.2017.16103
Tel Adıgüzel K, Yurdakul FG, Kürklü NS, Yaşar E, Bodur H (2021) Relationship between diet, oxidative stress, and inflammation in ankylosing spondylitis. Arch Rheumatol 37:1–10. https://doi.org/10.46497/ArchRheumatol.2022.9015
Ometto F, Ortolan A, Farber D, Lorenzin M, Dellamaria G, Cozzi G, Favero M, Valentini R, Doria A, Ramonda R (2021) Mediterranean diet in axial spondyloarthritis: an observational study in an Italian monocentric cohort. Arthritis Res Ther 23:219. https://doi.org/10.1186/s13075-021-02600-0
Schönenberger KA, Schüpfer AC, Gloy VL, Hasler P, Stanga Z, Kaegi-Braun N, Reber E (2021) Effect of anti-inflammatory diets on pain in rheumatoid arthritis: a systematic review and meta-analysis. Nutrients 13:4221. https://doi.org/10.3390/nu13124221
Pourhabibi-Zarandi F, Rafraf M, Zayeni H, Asghari-Jafarabadi M, Ebrahimi AA (2022) Effects of curcumin supplementation on metabolic parameters, inflammatory factors and obesity values in women with rheumatoid arthritis: a randomized, double-blind, placebo-controlled clinical trial. Phytother Res 36:1797–1806. https://doi.org/10.1002/ptr.7422
Bagherniya M, Darand M, Askari G, Guest PC, Sathyapalan T, Sahebkar A (2021) The clinical use of curcumin for the treatment of rheumatoid arthritis: a systematic review of clinical trials. Adv Exp Med Biol 1291:251–263. https://doi.org/10.1007/978-3-030-56153-6_15
Sanchez P, Letarouilly JG, Nguyen Y, Sigaux J, Barnetche T, Czernichow S, Flipo RM, Sellam J, Daïen C (2022) Efficacy of probiotics in rheumatoid arthritis and spondyloarthritis: a systematic review and meta-analysis of randomized controlled trials. Nutrients 14:354. https://doi.org/10.3390/nu14020354
Jabbari M, Barati M, Khodaei M, Babashahi M, Kalhori A, Tahmassian AH, Mosharkesh E, Arzhang P, Eini-Zinab H (2022) Is collagen supplementation friend or foe in rheumatoid arthritis and osteoarthritis? A comprehensive systematic review. Int J Rheum Dis 25:973–981. https://doi.org/10.1111/1756-185X.14382
Silva AR, Bernardo A, Costa J, Cardoso A, Santos P, de Mesquita MF, VazPatto J, Moreira P, Silva ML, Padrão P (2019) Dietary interventions in fibromyalgia: a systematic review. Ann Med 51:2–14. https://doi.org/10.1080/07853890.2018.1564360
Nadal-Nicolás Y, Miralles-Amorós L, Martínez-Olcina M, Sánchez-Ortega M, Mora J, Martínez-Rodríguez A (2021) Vegetarian and vegan diet in fibromyalgia: a systematic review. Int J Environ Res Public Health 18:4955. https://doi.org/10.3390/ijerph18094955
Martínez-Rodríguez A, Rubio-Arias JÁ, Ramos-Campo DJ, Reche-García C, Leyva-Vela B, Nadal-Nicolás Y (2020) Psychological and sleep effects of tryptophan and magnesium-enriched mediterranean diet in women with fibromyalgia. Int J Environ Res Public Health 17:2227. https://doi.org/10.3390/ijerph17072227
Horton-Hausknecht JR, Mitzdorf U, Melchart D (2000) The effect of hypnosis therapy on the symptoms and disease activity in rheumatoid arthritis. Psychol Health 14:1089–1104. https://doi.org/10.1080/08870440008407369
Bernardy K, Füber N, Klose P, Häuser W (2011) Efficacy of hypnosis/guided imagery in fibromyalgia syndrome–a systematic review and meta-analysis of controlled trials. BMC Musculoskelet Disord 12:133. https://doi.org/10.1186/1471-2474-12-133
Aravena V, García FE, Téllez A, Arias PR (2020) Hypnotic intervention in people with fibromyalgia: a randomized controlled trial. Am J Clin Hypn 63:49–61. https://doi.org/10.1080/00029157.2020.1742088
Zech N, Hansen E, Bernardy K, Häuser W (2017) Efficacy, acceptability and safety of guided imagery/hypnosis in fibromyalgia—a systematic review and meta-analysis of randomized controlled trials. Eur J Pain 21:217–227. https://doi.org/10.1002/ejp.933
Funding
None.
Author information
Authors and Affiliations
Contributions
Study design: BFK, ZS, MY, and AA. Data acquisition and review of the literature: BFK and AA. Making interpretations: BFK, ZS, MY, and AA. Drafting of the manuscript: BFK. Critical review of the manuscript: BFK, ZS, MY, and AA. Final approval: BFK, ZS, MY, and AA.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kocyigit, B.F., Sagtaganov, Z., Yessirkepov, M. et al. Assessment of complementary and alternative medicine methods in the management of ankylosing spondylitis, rheumatoid arthritis, and fibromyalgia syndrome. Rheumatol Int 43, 617–625 (2023). https://doi.org/10.1007/s00296-022-05267-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-022-05267-1