Abstract
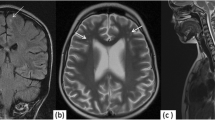
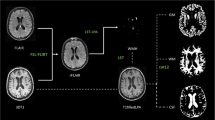
The purpose of this study was to identify the characteristic magnetic resonance imaging (MRI) findings in neuropsychiatric systemic lupus erythematosus (NPSLE) and to investigate the association between MRI findings and neuropsychiatric manifestations in SLE. Brain MRIs with a diagnosis of SLE from 2002 to 2013 from three tertiary university hospitals were screened. All clinical manifestations evaluated by brain MRI were retrospectively reviewed. If the clinical manifestations were compatible with the 1999 NPSLE American College of Rheumatology (ACR) nomenclature and case definitions, the brain MRIs were assessed for the presence of white matter hyperintensities, gray matter hyperintensities, parenchymal defects, atrophy, enhancement, and abnormalities in diffusion-weighted images (DWI). The number, size, and location of each lesion were evaluated. The neuropsychiatric manifestation of each brain MRI was classified according to the 1999 ACR NPSLE case definitions. The associations between MRI findings and NPSLE manifestations were examined. In total, 219 brain MRIs with a diagnosis of SLE were screened, and 133 brain MRIs met the inclusion criteria for NPSLE. The most common MRI abnormality was white matter hyperintensities, which were observed in 76 MRIs (57.1 %). Gray matter hyperintensities were observed in 41 MRIs (30.8 %). Parenchymal defects were found in 31 MRIs (23.3 %), and atrophy was detected in 20 MRIs (15.0 %). Patients who had seizures were more associated with gray matter hyperintensities than patients with other neuropsychiatric manifestations. Patients with cerebrovascular disease were more associated with gray matter hyperintensity, parenchymal defects, and abnormal DWI than patients with other neuropsychiatric manifestations. In addition to white matter hyperintensities, which were previously known as SLE findings, we also noted the presence of gray matter hyperintensities, parenchymal defects, and abnormal DWI in a substantial portion of SLE patients, particularly in those with cerebrovascular disease or seizures.


Similar content being viewed by others
References
Hanly JG (2005) Neuropsychiatric lupus. Rheum Dis Clin North Am 31(2):273–298
ACR ad hoc committee on neuropsychiatric lupus nomenclature (1999) The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum 42(4):599–608
Peterson PL, Axford JS, Isenberg D (2005) Imaging in CNS lupus. Best Pract Res Clin Rheumatol 19(5):727–739
Lee SP, Wu CS, Hsieh LC, Cheung WK, Chou MC (2014) Efficacy of magnetic resonance diffusion tensor imaging and three-dimensional fiber tractography in the detection of clinical manifestations of central nervous system lupus. Magn Reson Imaging 32(5):598–603
Zimny A, Szmyrka-Kaczmarek M, Szewczyk P, Bladowska J, Pokryszko-Dragan A, Gruszka E et al (2014) In vivo evaluation of brain damage in the course of systemic lupus erythematosus using magnetic resonance spectroscopy, perfusion-weighted and diffusion-tensor imaging. Lupus 23(1):10–19
Luyendijk J, Steens SC, Ouwendijk WJ, Steup-Beekman GM, Bollen EL, van der Grond J et al (2011) Neuropsychiatric systemic lupus erythematosus: lessons learned from magnetic resonance imaging. Arthritis Rheum 63(3):722–732
Ainiala H, Dastidar P, Loukkola J, Lehtimaki T, Korpela M, Peltola J, Hietaharju A (2005) Cerebral MRI abnormalities and their association with neuropsychiatric manifestations in SLE: a population-based study. Scand J Rheumatol 34(5):376–382
Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF et al (1982) The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 25(11):1271–1277
Appendix A: case definitions for neuropsychiatric syndromes in systemic lupus erythematosus. American College of Rheumatology. http://www.rheumatology.org/publications/ar/1999/aprilappendix.asp?aud=mem. Accessed 6 Aug 2014
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH (1992) Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 35(6):630–640
Systemic lupus erythematosus disease activity index SELENA modification. American College of Rheumatology. https://www.rheumatology.org/Practice/Clinical/Indexes/Systemic_Lupus_Erythematosus_Disease_Activity_Index_SELENA_Modification/. Accessed 6 Aug 2014
Ainiala H, Hietaharju A, Loukkola J, Peltola J, Korpela M, Metsanoja R, Auvinen A (2001) Validity of the new American College of Rheumatology criteria for neuropsychiatric lupus syndromes: a population-based evaluation. Arthritis Rheum 45(5):419–423
Hanly JG, Urowitz MB, Sanchez-Guerrero J, Bae SC, Gordon C, Wallace DJ et al (2007) Neuropsychiatric events at the time of diagnosis of systemic lupus erythematosus: an international inception cohort study. Arthritis Rheum 56(1):265–273
Jennings JE, Sundgren PC, Attwood J, McCune J, Maly P (2004) Value of MRI of the brain in patients with systemic lupus erythematosus and neurologic disturbance. Neuroradiology 46(1):15–21
Steup-Beekman GM, Zirkzee EJ, Cohen D, Gahrmann BM, Emmer BJ, Steens SC et al (2013) Neuropsychiatric manifestations in patients with systemic lupus erythematosus: epidemiology and radiology pointing to an immune-mediated cause. Ann Rheum Dis 72(Suppl 2):II76–II79
Hanly JG, Urowitz MB, Su L, Bae SC, Gordon C, Wallace DJ et al (2010) Prospective analysis of neuropsychiatric events in an international disease inception cohort of patients with systemic lupus erythematosus. Ann Rheum Dis 69(3):529–535
Appenzeller S, Pike GB, Clarke AE (2008) Magnetic resonance imaging in the evaluation of central nervous system manifestations in systemic lupus erythematosus. Clin Rev Allergy Immunol 34(3):361–366
Graham JW, Jan W (2003) MRI and the brain in systemic lupus erythematosus. Lupus 12(12):891–896
Abda EA, Selim ZI, Radwan ME, Mahmoud NM, Herdan OM, Mohamad KA, Hamed SA (2013) Markers of acute neuropsychiatric systemic lupus erythematosus: a multidisciplinary evaluation. Rheumatol Int 33(5):1243–1253
Sibbitt WL Jr, Sibbitt RR, Brooks WM (1999) Neuroimaging in neuropsychiatric systemic lupus erythematosus. Arthritis Rheum 42(10):2026–2038
Sanna G, Piga M, Terryberry JW, Peltz MT, Giagheddu S, Satta L et al (2000) Central nervous system involvement in systemic lupus erythematosus: cerebral imaging and serological profile in patients with and without overt neuropsychiatric manifestations. Lupus 9(8):573–583
Toledano P, Sarbu N, Espinosa G, Bargallo N, Cervera R (2013) Neuropsychiatric systemic lupus erythematosus: magnetic resonance imaging findings and correlation with clinical and immunological features. Autoimmun Rev 12(12):1166–1170
Kozora E, West SG, Kotzin BL, Julian L, Porter S, Bigler E (1998) Magnetic resonance imaging abnormalities and cognitive deficits in systemic lupus erythematosus patients without overt central nervous system disease. Arthritis Rheum 41(1):41–47
Jung RE, Segall JM, Grazioplene RG, Qualls C, Sibbitt WL, Roldan CA (2010) Cortical thickness and subcortical gray matter reductions in neuropsychiatric systemic lupus erythematosus. PLoS ONE 5(3):e9302
Katsumata Y, Harigai M, Kawaguchi Y, Fukasawa C, Soejima M, Kanno T et al (2010) Diagnostic reliability of magnetic resonance imaging for central nervous system syndromes in systemic lupus erythematosus: a prospective cohort study. BMC Musculoskelet Disord 11:13
Beauchamp NJ Jr, Ulug AM, Passe TJ, van Zijl PC (1998) MR diffusion imaging in stroke: review and controversies. Radiographics 18(5):1269–1283 discussion 1283-1265
Ebisu T, Naruse S, Horikawa Y, Ueda S, Tanaka C, Uto M et al (1993) Discrimination between different types of white matter edema with diffusion-weighted MR imaging. J Magn Reson Imaging 3(6):863–868
Moritani T, Hiwatashi A, Shrier DA, Wang HZ, Numaguchi Y, Westesson PL (2004) CNS vasculitis and vasculopathy: efficacy and usefulness of diffusion-weighted echoplanar MR imaging. Clin Imaging 28(4):261–270
Moritani T, Shrier DA, Numaguchi Y, Takahashi C, Yano T, Nakai K et al (2001) Diffusion-weighted echo-planar MR imaging of CNS involvement in systemic lupus erythematosus. Acad Radiol 8(8):741–753
Acknowledgments
This work was supported by a 2013 Inje University research grant (M. Her).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Hae Woong Jeong and Minyoung Her have equally contributed to this study as first authors.
Rights and permissions
About this article
Cite this article
Jeong, H.W., Her, M., Bae, J.S. et al. Brain MRI in neuropsychiatric lupus: associations with the 1999 ACR case definitions. Rheumatol Int 35, 861–869 (2015). https://doi.org/10.1007/s00296-014-3150-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-014-3150-8