Abstract
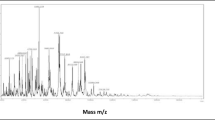
Bacteria causing diabetic foot infections (DFI) are chronic and generally multidrug resistant (MDR), which calls urgently for alternative antibacterials. The present study focused on potential metabolite producing bacteria from a saltpan environment and screened against MDR pathogens isolated from DFI patients. Molecular identification of the DFI pathogens provided Klebsiella quasivariicola, Staphylococcus argenteus, Escherichia coli, Staphylococcus hominis subsp. novobiosepticus, Bacillus australimaris, and Corynebacterium stationis. Among 34 isolated halophilic bacteria, the cell-free supernatant of strain PSH06 provided the largest inhibition zone of 23 mm against K. quasivariicola [D1], 21 mm against. S. argenteus [D2], 19 mm against E. coli [D3], and a minimum inhibition zone was found to be 14 mm against C. stationis [D8]. The potent activity providing stain confirmed as Pseudomonas aeruginosa through molecular identification. On the other hand, ethyl acetate extract of this strain showed excellent growth inhibition in MIC at 64 µg/mL against K. quasivariicola. Distressed cell membranes and vast dead cells were observed at MIC of ethyl acetate extract by SEM and CLSM against K.quasivariicola and E. coli. GC–MS profile of ethyl acetate extract exposed the occurrence of Bis (2-Ethylhexyl) Phthalate and n-Hexadecanoic acid and shows 100% toxic effect at 24 mg/mL by Artemia nauplii. The active extract fraction with above compounds derived from saltpan bacteria provided highest antibacterial efficacy against DFI-associated pathogens depicted with broad spectrum activity compared to standard antibiotics.





Similar content being viewed by others
References
WHO (2016) Global report on Diabetes. (https://www.who.int)
Lipsky BA, Berendt AR, Cornia PB, Pile JC, Peters EJC, Armstrong DG (2012) Infectious Diseases Society of America Clinical Practice Guideline for the Diagnosis and Treatment of Diabetic Foot Infections. Clin Infect Dis 54:e132–e173
Jneid J, Lavigne J, La Scola JP, Cassir B (2007) The diabetic foot microbiota: a review. Hum Microbiome J 5:1–6
Novick RP, Schlievert P, Ruzin A (2001) Pathogenicity and resistance islands of staphylococci. Microbes Infect 3:585–5945
Hernández G, Rico P, Díaz E, Rello J (2004) Nosocomial lung infections in adult intensive careunits. Microbes and Infect 6:1004–1014
Banu A, Noorul Hassan NM, Rajkumar J, Srinivasa S (2015) Spectrum of bacteria associated with diabetic foot ulcer and biofilm formation: A prospective study. Australas Med J 8:280–285
Otta S, Debata NK, Swain B (2019) Bacteriological profile of diabetic foot ulcers. Chrismed J Health Res 6:7–11
Bowler PG, Duerden BI, Armstrong DG (2001) Wound microbiology and associated approaches to wound management. Clin Microbiol Rev 14:244–269
Kapoor G, Saigal S, Elongavan A (2017) Action and resistance mechanisms of antibiotics: A guide for clinicians. J Anaesthesiol Clin Pharmacol 33:300–305
Bessa LJ, Fazii P, Di Giulio M, Cellini L (2013) Bacterial isolates from infected wounds and their antibiotic susceptibility pattern: some remarks about wound infection. Int Wound J 12:47–52
Dzidic S, Bedeković V (2003) Horizontal gene transfer-emerging multidrug resistance in hospital bacteria. Acta Pharmacol Sin 24:519–526
Tong YC, Davis JS, Eichenberger E, Holland TL, Fowler VG (2015) Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. J Clin Microbiol Rev 28:603–661
Sawale A, Kadam TA, Karale MA, Kadam OA (2014) Antimicrobial Activity of Secondary Metabolites from Halophilic Bacillus pumilus sp. Int J Curr Microbiol Appl Sci 3:506–512
Mellado E, Sánchez-Porro C, Ventosa A (2005) Proteases produced by Halophilic Bacteria and Archaea. Mic Enz and Biotrans 17:181–190
Conde Martínez N, Acosta-González A, Díaz LE (2017) Use of a mixed culture strategy to isolate halophilic bacteria with antibacterial and cytotoxic activity from the Manaure solar saltern in Colombia. BMC Mic 17:1–12
Wagner FW (1987) The diabetic foot. Orthopedics 10:163–172
Clinical and Laboratory Standards Institute (2015) CLSI document M100-S25. Performance standards for antimicrobial susceptibility testing; twenty-fifth informational supplements. Wayne: CLSI
Lane DJ (1991) 16S/23S rRNA sequencing. In: Stackebrandt E, Goodfellow M (eds) Nucleic acid techniques in bacterial systematics. John Wiley & Sons, New York, pp 115–175
Kumar S, Stecher G, Li M, Knyaz C, Tamura K (2018) MEGA X: Molecular Evolutionary Genetics Analysis across Computing Platforms. Mol Biol Evol 35:1547–1549
Bassole IHN, Ouattara AS, Nebie R, Ouattara CAT, Kabore ZI, Traore SA (2003) Chemical composition and antibacterial activities of the essential oils of Lippia chevalieri and Lippia multiflora from Burkina Faso. Photochemistry 62:209–212
O’Toole GA, Kolter R (1998) Initiation of biofilm formation in Pseudomonas fluorescens WCS365 proceeds via multiple, convergent signalling pathways: A genetic analysis. Mol Microbiol 28:449–461
Hisem D, Hrouzek P, Tomek P (2011) Cyanobacterial cytotoxicity versus toxicity to brine shrimp Artemiasalina. Toxicon 57:76–83
Richard JL, Lavigne JP, Sotto A (2012) Diabetes and foot infection: more than double trouble. Diabetes Metab Res Rev 28:46–53
Olender A (2013) Antibiotic Resistance and Detection of the Most Common Mechanism of Resistance (MLSB) of Opportunistic Corynebacterium. Chemotherapy 59:294–306
Olender A, Łetowska I (2010) Wound infections due to opportunistic Corynebacterium species. Med Dosw Microbial 62:135–140
Ferreira RL, Silva BCM, Rezende GS (2019) High Prevalence of Multidrug-Resistant Klebsiella pneumoniae Harboring Several Virulence and β-Lactamase Encoding Genes in a Brazilian Intensive Care Unit. Front Microbiol 9:1–15
Garza-Ramos U, Barrios-Camacho H, Moreno-Domínguez S (2018) Phenotypic and molecular characterization of Klebsiella spp. isolates causing community-acquired infections. New Microbes New Infect 23:17–27
Wesley Long S, Linson SE, Saavedra MO (2017) Whole-genome sequencing of a human clinical isolate of the novel species Klebsiella quasivariicola sp. nov. Genome Announc 5:1–2
Ogba OM, Nsan E, Eyam ES (2019) Aerobic bacteria associated with diabetic foot ulcers and their susceptibility pattern. Biomed Dermatolog 3:1–6
Calina D, Docea AO, Rosu L (2016) Antimicrobial resistance development following surgical site infections. Mol Med Rep 15:681–688
Alharbi NS, Khaled JM, Kadaikunnan S (2019) Prevalence of Escherichia coli strains resistance to antibiotics in wound infections and raw milk. Saudi J Biol Sci 26:1557–1562
Ragbetli C, Parlak M, Bayram Y, Guducuoglu H, Ceylan N (2016) Evaluation of Antimicrobial Resistance in Staphylococcus aureus Isolates by Years. Interdiscip Perspect Infect 2016:1–4
Indrawattana N, Pumipuntu N, Suriyakhun N, Jangsangthong A, Kulpeanprasit S, Chantratita N, Sookrung N, Chaicumpa W, Buranasinsup S (2019) Staphylococcus argenteus from rabbits in Thailand. Microbiology open 8:1–8
Potter RF, Lainhart W, Twentyman J (2018) Population Structure, Antibiotic Resistance, and Uropathogenicity of Klebsiella variicola. mBio 9:02481–2518
Hesselberg M, Vreeland RH (1995) Utilization of protein profiles for the characterization of halophilic bacteria. Curr Microbiol 31:158–162
Baati H, Amdouni R, Gharsallah N (2010) Isolation and Characterization of Moderately Halophilic Bacteria from Tunisian Solar Saltern. Curr Microbiol 60:157–161
Irshad A, Irshad K, Bum S (2014) Culturable diversity of halophilic bacteria in foreshore soils. Braz J Microbiol 45:563–571
Deepalaxmi RK, Gayathri C (2018) Screening of bioactive compound, antimicrobial activity producing halophilic isolates from the saltpans of Thoothukudi district. Afr J Mic Res 12:338–344
Altaee N, Jawad M, Hameed I (2016) Detection of volatile compounds produced by Pseudomonas aeruginosa isolated from UTI patients by gas chromatography-mass spectrometry. Int J Toxicol Pharmacol Res 8:462–470
Munhoz LD, Fonteque JP, Santos IMO (2017) Control of bacterial stem rot on tomato by extracellular bioactive compounds produced by Pseudomonas aeruginosa LV strain. Cogent Food Agric 3:1–16
Arul D, Balasubramani G, Balasubramanian V (2017) Antibacterial efficacy of silver nanoparticles and ethyl acetate metabolites of the potent halophilic (marine) bacterium, Bacillus cereus A30 on multidrug resistant bacteria. Patho and Glob Health 111:367–382
Matsuda M, Shigeta S, Okutani K (1999) Antiviral Activities of Marine Pseudomonas Polysaccharides and Their Oversulfated Derivatives. Mar Biotechnol 1:68–73
Lee DS, Eom SH, Jeong SY (2013) Anti-methicillin-resistant Staphylococcus aureus (MRSA) substance from the marine bacterium Pseudomonas sp. UJ-6. Environ Toxicol Pharmacol 35:171–177
Al-Bari MAA, Bhuiyan MSA, Flores ME (2005) Streptomyces bangladeshensis sp. nov., isolated from soil, which produces bis-(2-ethylhexyl) phthalate. Int J Syst Evol Microbiol 55:1973–1977
Lotfy MM, Hassan HM, Hetta MH (2018) Di-(2-ethylhexyl) Phthalate, a major bioactive metabolite with antimicrobial and cytotoxic activity isolated from River Nile derived fungus Aspergillus awamori. Beni-Suef Univ J Basic Appl Sci 7:263–269
Habib MR, Karim MR (2009) Antimicrobial and Cytotoxic Activity of Di-(2-ethylhexyl) Phthalate and Anhydrosophoradiol-3-acetate Isolated from Calotropisgigantea (Linn) Flower. Mycobiology 37:31–36
Tyagi T, Agarwal M (2017) phytochemical screening and GC-MS analysis of bioactive constituents in the ethanolic extract of Pistia stratiotes L. and Eichhorniacrassipes (Mart.) Solms. J Pharmacogn Phytochem 6:195–206
Anand Gideon V (2015) GC-MS analysis of phytochemical components of Pseudoglochidionanam alayanum Gamble: An endangered medicinal tree. Pelagia Res Libr Asian J Plant Sci Res 5:36–41
Ganesh M, Mohankumar M (2017) Extraction and identification of bioactive components in Sidacordata (Burm. f.) using gas chromatography–mass spectrometry. J Food Sci Technol 54:3082–3091
Shaeen M, Mominur Rahman M (2019) Assessment of Cytotoxic Activity Using Artemiasalina (Brine Shrimp Nauplii) of Citrus limon L (Lemon) Seed Extract. Ann Clin Toxicol 2(3):1023
Acknowledgements
The authors are thankful to DST-PURSE-DST Sanction Order No-SR/FT/LS-113/2009, (Bharathidasan University, Tiruchirapalli-24) for providing instrumentation facility during research period.A grant from MOST to Tan Han Shih (Hans-Uwe Dahms) is gratefully acknowledged (MOST 108-2621-M-037-001 and 109-2621-M-037-001 to T.H. Shih). This work was financially supported by the Research Center for Environmental Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan, from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan. NSYSU/KMU collaboration is acknowledged (108-PO25).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interests
The authors declare that they have no conflicts of interest.
Ethical Approval
The Collection of pus samples from the wound infected diabetic patients has been approved by the Institutional Ethics committee (IEC) for human research with the patient’s consents (Proposal S. No of IEC Management office: DM/2016/101/64) Bharathidasan University, Tiruchirappalli—620024). The information of patients was kept confidential.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.


284_2020_2190_MOESM4_ESM.docx
Table S3: Antibacterial activity of culture supernatants (SH1, SH3 and SH6), crude extract of various solvents of the PSH-06 strain against diabetic foot infection causing bacteria Additional file4 (DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Henciya, S., Vengateshwaran, T.D., Gokul, M.S. et al. Antibacterial Activity of Halophilic Bacteria Against Drug-Resistant Microbes Associated with Diabetic Foot Infections. Curr Microbiol 77, 3711–3723 (2020). https://doi.org/10.1007/s00284-020-02190-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00284-020-02190-1