Abstract
Background
Everolimus is a mTOR inhibitor used for the treatment of different solid malignancies. Many patients treated with the registered fixed 10 mg dose once daily are in need of dose interruptions, reductions or treatment discontinuation due to severe adverse events. This study determined the correlation between systemic everolimus exposure and toxicity. Additionally, the effect of different covariates on everolimus pharmacokinetics (PK) was explored.
Methods
Forty-two patients with advanced thyroid carcinoma were treated with 10 mg everolimus once daily. Serial pharmacokinetic sampling was performed on days 1 and 15. Subsequently, a population PK model was developed using NONMEM to estimate individual PK values used for analysis of an exposure–toxicity relationship. Furthermore, this model was used to investigate the influence of patient characteristics and genetic polymorphisms in genes coding for enzymes relevant in everolimus PK.
Results
Patients who required a dose reduction (n = 18) due to toxicity at any time during treatment had significant higher everolimus exposures [mean AUC0–24 (SD) 600 (274) vs. 395 (129) µg h/L, P = 0.008] than patients without a dose reduction (n = 22). A significant association between everolimus exposure and stomatitis was found in the four-level ordered logistic regression analysis (P = 0.047). The presence of at least one TTT haplotype in the ABCB1 gene was associated with a 21 % decrease in everolimus exposure.
Conclusion
The current study showed that dose reductions and everolimus-induced stomatitis were strongly associated with systemic everolimus drug exposure in patients with cancer. Our findings confirm observations from another study in patients with cancer and show us that everolimus is a good candidate for individualized dosing in patients with cancer.
ClinicalTrial.gov number
NCT01118065.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Everolimus is an orally administered rapamycin derivative inhibiting the mammalian target of rapamycin (mTOR) [1]. This is a key signaling molecule in the phosphatidylinositol 3-kinase (PI3K)/Akt pathway which is involved in the regulation of growth, proliferation, metabolism, survival and angiogenesis of cells and often dysregulated in cancer [1]. Currently, everolimus is registered for the treatment of advanced hormone receptor positive (HR+), human epidermal growth factor-2 negative (HER2−) breast cancer in postmenopausal women in combination with exemestane, for metastatic renal cell carcinoma (mRCC), and for irresectable or metastatic pancreatic neuroendocrine tumors (pNET) and subependymal giant cell astrocytoma (SEGA) [2–4].
Despite its proven efficacy, everolimus is also associated with a number of serious side effects. Most common toxicities associated with everolimus therapy include stomatitis, rash, fatigue, diarrhea, infections, nausea, loss of appetite, hematologic toxicities, dyspnea, noninfectious pneumonitis and metabolic abnormalities such as hypercholesterolemia and hyperglycemia [5]. While it is reported that the majority of these adverse events are manageable and of mild-to-moderate severity, many patients are in need of dose interruptions, reductions or treatment discontinuation due to toxicity [6]. Indeed, in the pivotal breast cancer, mRCC and pNET phase III trials, 10–35 % of the patients discontinued everolimus treatment due to adverse events [2–4]. In addition, ~62 % of the patients needed dose interruptions or reductions compared to 12–29 % in the placebo arms [2, 4].
The large number of dose reductions and treatment discontinuation make toxicity currently one of the main challenges in the optimal use of everolimus for the treatment of cancer. In oncology, everolimus is registered as a fixed oral dose of 10 mg once daily. However, in transplantation medicine therapeutic drug monitoring (TDM) with individualized dosing is routinely applied due to everolimus’ narrow therapeutic window and high inter-patient variability in pharmacokinetics (PK) [7]. In transplantation medicine, everolimus is used as an immunosuppressant to prevent rejections. Dose individualization is not only applied to prevent toxicity, but also to optimize treatment efficacy. In oncology, the same high inter-patient variability in PK is seen (AUC; 45 CV%, C trough; 60 CV%) [8]. This substantial variability, in combination with the fixed 10 mg dosing, results in large differences in everolimus exposure between patients. This could result in either supra-therapeutic drug exposure with an increased incidence of toxicity, but also in subtherapeutic drug exposure leading to decreased anticancer effects.
The primary objective of this study was to assess the correlation between everolimus exposure and toxicity in patients with advanced thyroid cancer. Additionally, we explored the influence of different covariates on everolimus PK, including genetic polymorphisms in genes encoding enzymes involved in the absorption and metabolism of everolimus.
Materials and methods
Patients
Forty-two patients were enrolled in this phase II study investigating the efficacy and PK of everolimus for the treatment of progressive or recurrent, unresectable or metastatic thyroid cancer. The efficacy data of this study will be reported separately. Participating medical centers were the Leiden University Medical Center and the University Medical Center Groningen. Patients were treated continuously with everolimus at an once-daily oral dose of 10 mg until tumor progression, unacceptable toxicity, death or discontinuation from the study for other reasons. Toxicities were assessed at baseline, days 1, 14 and 28 of therapy and monthly thereafter according to the National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTC-AE) version 4.0. Dose adjustments were permitted for adverse events suspected to be related to everolimus. The first dose reduction was to 5 mg once daily. If another dose reduction was needed, everolimus was dosed as 5 mg every other day. The study was approved by the institutional ethics committees (Leiden University Medical Center and University Medical Center Groningen, the Netherlands), and all patients gave written informed consent before entering the study.
Pharmacokinetic sample collection and analysis
For everolimus PK assessment, whole blood samples were obtained at days 1 and 15 of therapy. Samples were collected into EDTA tubes at predose and 1, 2 and 3 h after everolimus intake (sparse schedule). More extensive PK sampling at 4, 5, 6, 7 and 8 h after everolimus intake was optional for patients (extensive schedule). Samples were stored at −20 °C until the day of analysis.
Everolimus concentrations in whole blood were measured using a validated ultra performance liquid chromatography-tandem mass spectrometric (UPLC-MS/MS) assay. Validation of the assay was performed according to the EMA guidelines of bioanalytical method development [9]. The calibration line was linear over the range from 2 to 160 µg/L, and the lower limit of quantification (LLOQ) was 0.6 µg/L. Assay performance was in agreement with guidelines for bioanalytical method development and validation.
Pharmacogenetic analysis
Single-nucleotide polymorphisms and haplotype selection
Everolimus is metabolized by the cytochrome P450 (CYP) enzymes CYP3A4, CYP3A5 and CYP2C8 and is also a substrate for the efflux pump P-glycoprotein (P-gp) encoded by the ABCB1 gene [10]. The nuclear pregnane X receptor (PXR; NR1I2) regulates the expression of CYP3A4 and could therefore also influence everolimus PK [11]. Eleven single-nucleotide polymorphisms (SNPs) in these genes were selected based upon a candidate gene approach (Supplementary Data S1, online). For the ABCB1 and CYP2C8 gene, selected SNPs were used for haplotype analysis performed in gPLINK (Supplementary Data S2, online). Haplotypes were set at a certainty >0.97. For the ABCB1 and CYP2C8 genes, only haplotypes and no individual SNPs were tested.
Genotyping assays
Germline DNA was isolated from 400 µl EDTA blood using MagNa Pure Compact (Roche, Almere, the Netherlands). DNA concentrations were thereafter measured using Nanodrop (Isogen, De Meern, the Netherlands). Genotyping was performed using predesigned genotyping assays (Supplementary Data S1, online). Samples were analyzed on a Viia7 real-time PCR system according to the manufacturers’ instruction (Life Technologies, Bleiswijk, the Netherlands). Call rates of all assays were >98 %. As a quality control, at least 5 % of the samples were genotyped in duplicate. No inconsistencies were observed. Minor allele frequencies (MAF) of all 11 SNPs were calculated and compared with reported MAF for European Populations (HAPMAP). No significant deviations were observed, and derived allele frequencies were all in Hardy–Weinberg equilibrium (P ≥ 0.05) (Supplementary Data S1, online).
Pharmacokinetic modeling
Base model
Thirty patients completed the extensive PK sampling and ten patients the sparse PK sampling schedule. After PK sampling, nonlinear mixed-effects modeling (NONMEM) was used to describe the population PK of everolimus. Subsequently, the developed population PK model was used to estimate individual everolimus exposure both in terms of AUC0–24 by using clearance and with use of the model predicted C trough levels. NONMEM version 7.2 (Icon Development Solutions, Ellicott City, MD, USA) was used with Piranã (version 2.9.0) as the modeling environment. Statistical software package R (version 2.15.1) was used for handling of data and plot generation. We also used NONMEM to explore the influence of different covariates on everolimus PK.
A first-order conditional estimation method with interaction (FOCE-I) was used to fit models throughout the building process. One- and two-compartment models with first-order elimination were explored. It was also assessed whether there was a change in clearance from day 1 to day 15 of treatment. Model selection was based on goodness of fit and statistical significance. An adjusted model was chosen over the original model if the drop in the objective function value (OFVs) was >3.84 [P < 0.05 with one degree of freedom (df), assuming χ 2-distribution].
Since the bioavailability (F) of everolimus is unknown, F was fixed at 1 and PK parameter estimates reported are proportional to F except K a. In addition, both clearance (Cl/F) and the volume of distribution (V d/F) were allometrically scaled [12].
Covariate analysis
After the base model was determined, covariates were tested to explore the influence of bilirubin, aspartate aminotransferase (ASAT), alanine aminotransferase (ALAT), creatinine, body surface area (BSA) and hematocrit on Cl/F. Individual effect sizes were estimated with the formula \({\text{Cl}}/F_{{{\text{typical}}\,{\text{value}}}} = \theta_{1} \times ({\text{COV}}/{\text{COV}}_{\text{median}} )^{{\theta_{2} }}\), whereby θ 1 is the population estimate for Cl/F, COV the tested covariate and θ 2 the covariant effect size estimate.
The influence of SNPs and haplotypes was all tested as a covariate on Cl/F, except for ABCB1 haplotypes which were tested for an effect on F as this is physiologically more plausible. Effect sizes were estimated with the formula Cl/F typical value (or F) = \(\theta_{1} \times \theta_{2}^{{{\text{pg}}1}} \times \theta_{3}^{{{\text{pg}}2}} ,\) whereby θ 1 is the population Cl/F or F estimate in wild-type patients, θ 2 the covariate effect size of the heterozygote mutation status and θ 3 the effect size of the homozygote mutation status. The heterozygote (pg1) and homozygote (pg2) mutation status was scored as 1 if present or 0 if not present. If the genotype frequency was <0.1, homozygote mutant and heterozygote mutant genotypes were combined (Supplementary Data S1 and S2, online).
All covariates were first tested for statistical significance with univariate forward inclusion into the base model (drop in OFV >3.84, df = 1, P < 0.05). After inclusion of significant covariates in the intermediate model, a stepwise backward elimination procedure was performed. Covariates were remained in the final model if the threshold for statistical significance of backward elimination was reached (increase in OFV >6.64, df = 1, P < 0.01).
Evaluation of model fit
Next to goodness-of-fit plots, a visual predictive check (VPC) was used to assess the performance of the final model by comparing the 10th and 90th percentiles of the simulated concentrations with those of the observed concentrations. In addition, a bootstrap analysis was performed to evaluate the precision of parameter estimation. Shrinkage in inter-individual variability and residual errors were automatically calculated by NONMEM.
Assessment of systemic exposure toxicity relationship
Selection of toxicities
In this study, all experienced toxicities were scored according to CTC-AE version 4.0. However, due to the number of patients included, only a limited number of toxicities were selected to be tested for an association with everolimus exposure in order to prevent false-positive findings.
We choose dose reductions as the first outcome of toxicity as this is the sum of all different toxicities experienced by patients and these are also the toxicities that lead to clinical action by the treating physician. In addition, we selected stomatitis and pneumonitis as toxicity outcomes. The rationale for selection of these toxicities was based on their prevalence and the fact that these toxicities are (1) objectively measurable, (2) clinically relevant and (3) untreatable and therefore leading to dose reductions or discontinuation of therapy. Toxicities were scored as the highest grade experienced until dose reduction and if no reduction occurred until the end of study.
Statistical analysis
The difference in day 15 steady-state everolimus exposure (AUC0–24 and Ctrough) between patients with and without dose reductions was tested with an unpaired t test. The relationships between day 15 everolimus exposure (AUC0–24 and C trough) and stomatitis and pneumonitis were evaluated using a four-level ordered logistic regression in SPSS version 20.0 (IBM).
Results
Patient characteristics
Forty-two adult patients with thyroid carcinoma, 22 men and 20 women were included in the phase II trial that investigated everolimus for the treatment of thyroid cancer. Of these patients, 28 (66.7 %) had differentiated, 7 (16.7 %) had undifferentiated (anaplastic) and 7 (16.7 %) had medullary advanced thyroid carcinoma. Two patients were excluded for PK analysis; in one patient, no PK samples were collected, and in the other patient, no measurable everolimus levels could be detected. Patient baseline characteristics are shown in Table 1.
Pharmacokinetics
A total of 669 samples from 40 patients were used to build the population PK model. The pharmacokinetic data for everolimus were best described by a two-compartmental model with first-order absorption and first-order elimination from the central compartment (Supplementary Data S3, online). No difference in clearance over time between day 1 and day 15 of treatment was found.
Forward inclusion of BSA, creatinine, ASAT, ALAT, bilirubin and hematocrit did not improve the PK model, and no association between these covariates and clearance was found. With forward inclusion of the ABCB1 TTT and CCG haplotype, the base model significantly improved (ΔOFV = −7.2 and −6.4, respectively, P < 0.05). The other SNPs and the CYP2C8 haplotype did not improve the model. With multivariate backward elimination, only the presence of at least one ABCB1 TTT haplotype remained significant (ΔOFV = 9.6, P < 0.01). A 21 % decrease in F was observed in the presence of at least one ABCB1 TTT haplotype. Inclusion of this covariate in the final PK model reduced the inter-patient variability in Cl/F from 38.1 to 35.1 CV%. Parameter estimates of the base and final model are shown in Table 2.
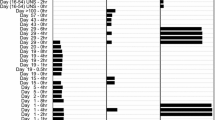
Evaluation of the final model was, next to inspection of the goodness-of-fit plots, done with VPC and a bootstrap procedure. Results of the VPC show that predicted and observed concentration intervals are almost identical, indicating accuracy and good predictive performance of the final model (Fig. 1). There is a small tendency for a difference between predicted and observed concentrations in the absorption part of the curve due to limited number of samples during this phase. Since we mainly used the model to estimate individual values for Cl/F, the modest under-prediction of the absorption did not affect our analysis. The successful bootstrap procedure with 1000 runs is shown in Table 2. The median values for PK parameters found were within 10 % of those estimated with the final model, indicating that the model is precise and reliable in its parameter estimation.
Exposure–toxicity relationship
The relationships between everolimus exposure and dose reductions as well as stomatitis and pneumonitis were examined. In total, 45 % of the patients had their everolimus 10 mg dose reduced to a lower dose due to toxicity (Table 3). In general, toxicity developed within 3 months after the start of everolimus therapy. Toxicities leading to dose reduction included stomatitis, pneumonitis, fatigue, loss of appetite, diarrhea, liver and kidney toxicity and edema. Considering stomatitis, 42.5 % of the patients experienced any grade stomatitis and 7.5 % experienced grade 3 stomatitis. In addition, 10 % of the patients had a noninfectious pneumonitis.
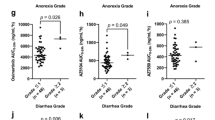
Figure 2 shows boxplots of everolimus AUC and Ctrough in patients with and without dose reduction. Mean AUC0–24(SD) and C trough were 600 (274) and 395 (129) µg h/L and 14.9 (9.0) and 8.4 (3.8) µg/L for patients with and without dose reductions, respectively. The exposure to everolimus was significantly different between the two groups (mean difference in AUC −204 µg h/L (95 % CI −340 to −69 µg h/L, P = 0.008 and mean difference in C trough −6.5 µg/L (95 % CI −11.2 to −1.8 P = 0.009). Figure 3 shows boxplots of AUCs and C trough in patients experiencing different grades of stomatitis. A positive association between everolimus exposure and stomatitis was identified (P = 0.047). The odd ratio for stomatitis was 1.16 (95 % CI; 1.06–1.26) for every 50 µg h/L increase in AUC0–24. Patients with grade 3 stomatitis had an everolimus exposure that was two times that of patients with ≤2 stomatitis (AUC0–24 896 vs. 456 µg h/L, P > 0.05 and C trough 24.9 vs. 10.3 µg/L, P > 0.05). No association of everolimus exposure with pneumonitis was found.
Discussion
This study was primarily performed to assess the correlation between everolimus exposure and toxicity. Results show that patients who had their everolimus dose reduced due to toxicity had significantly higher drug exposures than patients without the need for dose reductions. Moreover, everolimus exposure was associated with the probability for stomatitis and patients with grade 3 stomatitis had an everolimus exposure two times that of patients with ≤2 stomatitis. Additionally, we found that the presence of at least one TTT allele in the ABCB1 gene was associated with lower everolimus exposure due to decreased absorption.
The present findings of a clear relationship between everolimus exposure and dose reductions due to toxicity and stomatitis are in line with results from other studies in patients with cancer treated with everolimus. Previously, it has been shown that a twofold increase in everolimus exposure increased the risk of ≥grade 3 pulmonary events, ≥grade 3 stomatitis and ≥grade 3 metabolic events with 1.9-fold, 1.5-fold and 1.3-fold, respectively, in patients with advanced solid tumors [13]. The present analysis could not confirm the earlier identified association of everolimus exposure with pneumonitis, but this may be due to the limited number of patients with pneumonitis in our study cohort.
The fixed 10-mg dosing regimen of everolimus is based on its safety profile together with its pharmacodynamic effects on the mTOR-dependent pathway in tumor and skin biopsies [14, 15]. These studies suggested a dose of ≥5 or ≥10 mg daily, based on complete inhibition of serine/threonine kinase p70S6 kinase (S6K1) or phosphorylated eIF-4G (peIF-4G) which are both downstream targets of mTOR. Since inhibition of peIF-4G was only complete at the 10-mg dose level, it was advised to use the 10-mg once-daily schedule for future clinical studies. The clinical relevance of this difference in inhibition of eIF-4G is, however, unknown and should be further investigated as higher dosing introduces also more toxicity.
The present study underscores the high inter-patient variability in everolimus PK which is in line with previous observations [8]. This is also analog to the variability in PK seen for other oral targeted therapies for the treatment of cancer such as tyrosine kinase inhibitors (TKIs). For TKIs, the evidence for relationships between systemic drug exposure and efficacy or toxicity endpoints is growing [16, 17]. The currently available data suggest that an individualized dosing approach seems justified in certain circumstances and different studies support the feasibility of an individualized dosing approach for TKIs [18, 19].
In the exploration of covariates of influence on everolimus PK, the presence of at least one TTT haplotype was responsible for a decrease in everolimus exposure due to decreased absorption. Previously, the TTT haplotype has been demonstrated to be associated with enhanced function of the P-glycoprotein transporter and indeed reduced exposure or efficacy of treatment [20–22]. However, decreased function of the transporter and thus increased exposure have also been reported, as well as studies that could not show an effect [7, 23, 24]. The association we found should be regarded as preliminary and needs further validation. If this association is confirmed, it might be argued whether a decrease in exposure of 21 % can be considered as clinically relevant when taking into account the inter-patient variability in everolimus PK.
To the best of our knowledge, we are the first to describe the population PK of everolimus 10 mg once daily in patient with cancer. Previously, population PK models have been described, but only within the field of transplantation medicine where everolimus is used in a much lower dose. Taking this and differences in modeling into account, pharmacokinetic parameter estimates were in agreement with those previously found [7].
Everolimus exposures were assessed at day 15 of therapy and not necessarily at the time when adverse events occurred. This may be considered as a limitation, and future studies should preferably measure everolimus exposure at the time that toxicity occurs. However, the variability in everolimus PK within a patient (intra-patient) is reported to be much smaller than the variability between patients [25, 26]. In addition, we observed a constant clearance of everolimus over time. While treated at the same dose (10 mg once daily), this restricts the probability for large differences between the exposures that we have measured and the actual exposures that would have been measured at the moment that toxicity occurred. In addition, the study that previously described a correlation between everolimus exposure and toxicity found similar results with the use of C trough at the time of toxicity or when C trough averaged over a given time period was used [13].
The present results both underscore the correlation between everolimus exposure and dose reductions due to toxicity as well as the high inter-patient variability in everolimus PK. These observations should be taken into account in the use of everolimus for the treatment of solid tumors. Preventing high drug exposures by dose individualization may have the potential to reduce the side effects of everolimus therapy while remaining its efficacy. However, prospective validation within oncology patients in necessary. Moreover, it has been shown that high early everolimus exposure (C trough >14.1 µg/L) is associated with longer progression-free survival (PFS) and overall survival (OS) (13.3 and 26.2 vs. 3.9 and 9.9 months for PFS and OS, respectively) in patients with mRCC [27]. Hence, an individualized dosing approach may also be of value for some patients with treatment inefficacy due to subtherapeutic exposures. On the other hand, in this present analysis there were also patients in need of dose reductions in whom the exposure to everolimus was not elevated. This finding suggests that a subpopulation may not benefit from dose individualization but maybe more from treatment switch if available. In summary, future studies are required to define the therapeutic window of everolimus for the treatment of different malignancies and these studies should aim to optimize both treatment toxicity and efficacy outcomes possibly by using everolimus in a more individualized way.
Conclusion
In conclusion, this study shows a clear association between everolimus exposure and dose reductions due to toxicity as well as stomatitis in patients with cancer using a newly developed population PK model. Our findings confirm observations from another study in patients with cancer and show us that everolimus is a good candidate for individualized dosing in patients with cancer.
References
Meric-Bernstam F, Gonzalez-Angulo AM (2009) Targeting the mTOR signaling network for cancer therapy. J Clin Oncol 27:2278–2287
Baselga J, Campone M, Piccart M et al (2012) Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med 366:520–529
Motzer RJ, Escudier B, Oudard S et al (2008) Efficacy of everolimus in advanced renal cell carcinoma: a double-blind, randomised, placebo-controlled phase III trial. Lancet 372:449–456
Yao JC, Shah MH, Ito T et al (2011) Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med 364:514–523
European Medicine Agency (EMA) (2010) Afinitor® (everolimus): European Public Assessment Report (EPAR). http://www.ema.europa.eu/. Accessed 1 Mar 2015
Aapro M, Andre F, Blackwell K et al (2014) Adverse event management in patients with advanced cancer receiving oral everolimus: focus on breast cancer. Ann Oncol 25:763–773
Moes DJ, Press RR, den Hartigh J et al (2012) Population pharmacokinetics and pharmacogenetics of everolimus in renal transplant patients. Clin Pharmacokinet 51:467–480
O’Donnell A, Faivre S, Burris HA III et al (2008) Phase I pharmacokinetic and pharmacodynamic study of the oral mammalian target of rapamycin inhibitor everolimus in patients with advanced solid tumors. J Clin Oncol 26:1588–1595
European Medicine Agency (EMA) (2011) Guideline on bioanalytical method validation
Kirchner GI, Meier-Wiedenbach I, Manns MP (2004) Clinical pharmacokinetics of everolimus. Clin Pharmacokinet 43:83–95
Istrate MA, Nussler AK, Eichelbaum M et al (2010) Regulation of CYP3A4 by pregnane X receptor: the role of nuclear receptors competing for response element binding. Biochem Biophys Res Commun 393:688–693
Anderson BJ, Holford NH (2009) Mechanistic basis of using body size and maturation to predict clearance in humans. Drug Metab Pharmacokinet 24:25–36
Ravaud A, Urva SR, Grosch K et al (2014) Relationship between everolimus exposure and safety and efficacy: meta-analysis of clinical trials in oncology. Eur J Cancer 50:486–495
Tanaka C, O’Reilly T, Kovarik JM et al (2008) Identifying optimal biologic doses of everolimus (RAD001) in patients with cancer based on the modeling of preclinical and clinical pharmacokinetic and pharmacodynamic data. J Clin Oncol 26:1596–1602
Tabernero J, Rojo F, Calvo E et al (2008) Dose- and schedule-dependent inhibition of the mammalian target of rapamycin pathway with everolimus: a phase I tumor pharmacodynamic study in patients with advanced solid tumors. J Clin Oncol 26:1603–1610
de Wit D, Guchelaar HJ, den Hartigh J et al (2015) Individualized dosing of tyrosine kinase inhibitors: are we there yet? Drug Discov Today 20:18–36
Yu H, Steeghs N, Nijenhuis CM et al (2014) Practical guidelines for therapeutic drug monitoring of anticancer tyrosine kinase inhibitors: focus on the pharmacokinetic targets. Clin Pharmacokinet 53:305–325
Lankheet NA, Kloth JS, Gadellaa-van Hooijdonk CG et al (2014) Pharmacokinetically guided sunitinib dosing: a feasibility study in patients with advanced solid tumours. Br J Cancer 110:2441–2449
Verheijen R, Bins S, Gadellaa-van Hooijdonk CG et al (2014) Individualized pharmacokinetically-guided dosing of pazopanib: a feasibility study in cancer patients. In: ESMO meeting 2014; abstract no. 7651
Kim RB, Leake BF, Choo EF et al (2001) Identification of functionally variant MDR1 alleles among European Americans and African Americans. Clin Pharmacol Ther 70:189–199
Hung CC, Tai JJ, Lin CJ et al (2005) Complex haplotypic effects of the ABCB1 gene on epilepsy treatment response. Pharmacogenomics 6:411–417
Wasilewska A, Zalewski G, Chyczewski L et al (2007) MDR-1 gene polymorphisms and clinical course of steroid-responsive nephrotic syndrome in children. Pediatr Nephrol 22:44–51
van Erp NP, Eechoute K, van der Veldt AAM et al (2009) Pharmacogenetic pathway analysis for determination of sunitinib-induced toxicity. J Clin Oncol 27:4406–4412
Aarnoudse AJ, Dieleman JP, Visser LE et al (2008) Common ATP-binding cassette B1 variants are associated with increased digoxin serum concentration. Pharmacogenet Genomics 18:299–305
Budde K, Fritsche L, Waiser J et al (2005) Pharmacokinetics of the immunosuppressant everolimus in maintenance renal transplant patients. Eur J Med Res 10:169–174
U.S. Food and Drug Administration (2009) Afinitor® (everolimus): drug approval report. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/. Accessed 5 May 2015
Thiery-Vuillemin A, Mouillet G, Nguyen Tan HT et al (2014) Impact of everolimus blood concentration on its anti-cancer activity in patients with metastatic renal cell carcinoma. Cancer Chemother Pharmacol 73:999–1007
Acknowledgments
We would like to thank Lammie Stoffer for her assistance with sample collection. We would also like to thank Trees Hessing, Jacqueline König-Quartel and Tahar van der Straaten for their assistance with sample analysis.
Authors’ contributions
E. Kapiteijn and N.P. van Erp involved in conception and design. D. de Wit, T.C Schneider, D.J.A.R. Moes, C.F.M. Roozen, J. den Hartigh, T.P Links, E. Kapiteijn and N.P. van Erp involved in acquisition of data. D. de Wit, T.C. Schneider, D.J.A.R. Moes, C.F.M. Roozen, J. den Hartigh, H. Gelderblom, H.J. Guchelaar, J.J. van der Hoeven, T.P Links, E. Kapiteijn and N.P. van Erp involved in analysis and interpretation of data. D. de Wit, T.C. Schneider, D.J.A.R. Moes, C.F.M. Roozen, J. den Hartigh, H. Gelderblom, H.J. Guchelaar, J.J. van der Hoeven, T.P Links, E. Kapiteijn and N.P van Erp involved in writing, review and/or revision of the manuscript. E. Kapiteijn involved in study supervision.
Funding
We would like to thank Novartis for funding this investigator initiated study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
D. de Wit and T.C. Schneider contributed equally to this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary data 3.
Schematic presentation of PK model (TIFF 502 kb)
Supplementary data 4.
Goodness-of-fit (GOF) plot of individual predicted vs. observed everolimus concentrations (PDF 31 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
de Wit, D., Schneider, T.C., Moes, D.J.A.R. et al. Everolimus pharmacokinetics and its exposure–toxicity relationship in patients with thyroid cancer. Cancer Chemother Pharmacol 78, 63–71 (2016). https://doi.org/10.1007/s00280-016-3050-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-016-3050-6