Abstract
Purpose
Defective expression of the mismatch repair protein MSH3 is frequently detected in colon cancer, and down-regulation of its expression was found to decrease sensitivity to platinum compounds or poly(ADP-ribose) polymerase inhibitors (PARPi) monotherapy. We have investigated whether MSH3 transfection in MSH3-deficient colon cancer cells confers resistance to oxaliplatin or PARPi and whether their combination restores chemosensitivity.
Methods
MSH3-deficient/MLH1-proficient colon cancer HCT116MLH1 cells were transfected with the MSH3 cDNA cloned into the pcDNA3.1(−) vector. MSH3/MLH1-deficient HCT116, carrying MLH1 and MSH3 mutations on chromosome 3 and 5, respectively, and HCT116 in which wild-type MLH1 (HCT116+3), MSH3 (HCT116+5) or both genes (HCT116+3+5) were introduced by chromosome transfer were also tested. Sensitivity to oxaliplatin and to PARPi was evaluated by analysis of clonogenic survival, cell proliferation, apoptosis and cell cycle.
Results
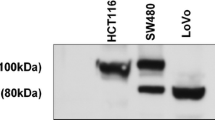
MSH3 transfection in HCT116 cells did not confer resistance to oxaliplatin or PARPi monotherapy. MSH3-proficient HCT116+5 or HCT116+3+5 cells, which were more resistant to oxaliplatin and PARPi in comparison with their MSH3-deficient counterparts, expressed higher levels of the nucleotide excision repair ERCC1 and XPF proteins, involved in the resistance to platinum compounds, and lower PARP-1 levels. In all cases, PARPi increased sensitivity to oxaliplatin.
Conclusions
Restoring of MSH3 expression by cDNA transfection, rather than by chromosome transfer, did not affect colon cancer sensitivity to oxaliplatin or PARPi monotherapy; PARP-1 levels seemed to be more crucial for the outcome of PARPi monotherapy.




Similar content being viewed by others
References
Fink D, Nebel S, Aebi S, Zheng H, Cenni B, Nehmé A, Christen RD, Howell SB (1996) The role of DNA mismatch repair in platinum drug resistance. Cancer Res 56:4881–4886
Vaisman A, Varchenko M, Umar A, Kunkel TA, Risinger JI, Barrett JC, Hamilton TC, Chaney SG (1998) The role of hMLH1, hMSH3, and hMSH6 defects in cisplatin and oxaliplatin resistance: correlation with replicative bypass of platinum-DNA adducts. Cancer Res 58:3579–3585
Martin LP, Hamilton TC, Schilder RJ (2008) Platinum resistance: the role of DNA repair pathways. Clin Cancer Res 14:1291–1295. doi:10.1158/1078-0432.CCR-07-2238
Carethers JM, Chauhan DP, Fink D, Nebel S, Bresalier RS, Howell SB, Boland CR (1999) Mismatch repair proficiency and in vitro response to 5-fluorouracil. Gastroenterology 117:123–131
Meyers M, Wagner MW, Hwang HS, Kinsella TJ, Boothman DA (2001) Role of the hMLH1 DNA mismatch repair protein in fluoropyrimidine-mediated cell death and cell cycle responses. Cancer Res 61:5193–5201
Sinicrope FA, Foster NR, Thibodeau SN, Marsoni S, Monges G, Labianca R, Kim GP, Yothers G, Allegra C, Moore MJ, Gallinger S, Sargent DJ (2011) DNA mismatch repair status and colon cancer recurrence and survival in clinical trials of 5-fluorouracil-based adjuvant therapy. J Natl Cancer Inst 103:863–875. doi:10.1093/jnci/djr153
Plaschke J, Krüger S, Jeske B, Theissig F, Kreuz FR, Pistorius S, Saeger HD, Iaccarino I, Marra G, Schackert HK (2004) Loss of MSH3 protein expression is frequent in MLH1-deficient colorectal cancer and is associated with disease progression. Cancer Res 64:864–870. doi:10.1158/0008-5472.CAN-03-2807
Plaschke J, Preußler M, Ziegler A, Schackert HK (2012) Aberrant protein expression and frequent allelic loss of MSH3 in colorectal cancer with low-level microsatellite instability. Int J Colorectal Dis 27:911–919
Wang Q, Zhang H, Guerrette S, Chen J, Mazurek A, Wilson T, Slupianek A, Skorski T, Fishel R, Greene MI (2001) Adenosine nucleotide modulates the physical interaction between hMSH2 and BRCA1. Oncogene 20:4640–4649
Fong PC, Yap TA, Boss DS, Carden CP, Mergui-Roelvink M, Gourley C, De Greve J, Lubinski J, Shanley S, Messiou C, A’Hern R, Tutt A, Ashworth A, Stone J, Carmichael J, Schellens JH, de Bono JS, Kaye SB (2010) Poly(ADP)-ribose polymerase inhibition: frequent durable responses in BRCA carrier ovarian cancer correlating with platinum-free interval. J Clin Oncol 2:2512–2519. doi:10.1200/JCO.2009.26.9589
Dann RB, DeLoia JA, Timms KM, Zorn KK, Potter J, Flake DD 2nd, Lanchbury JS, Krivak TC (2012) BRCA1/2 mutations and expression: response to platinum chemotherapy in patients with advanced stage epithelial ovarian cancer. Gynecol Oncol 125:677–682. doi:10.1016/j.ygyno.2012.03.006
Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, Kyle S, Meuth M, Curtin NJ, Helleday T (2005) Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature 434:913–917. doi:10.1038/nature03443
Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, Santarosa M, Dillon KJ, Hickson I, Knights C, Martin NM, Jackson SP, Smith GC, Ashworth A (2005) Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 434:917–921. doi:10.1038/nature03445
Dedes KJ, Wilkerson PM, Wetterskog D, Weigelt B, Ashworth A, Reis-Filho JS (2011) Synthetic lethality of PARP inhibition in cancers lacking BRCA1 and BRCA2 mutations. Cell Cycle 10:1192–1199
Takahashi M, Koi M, Balaguer F, Boland CR, Goel A (2011) MSH3 mediates sensitization of colorectal cancer cells to cisplatin, oxaliplatin, and a poly(ADP-ribose) polymerase inhibitor. J Biol Chem 286:12157–12165. doi:10.1074/jbc.M110.198804
Papadopoulos N, Nicoladesi NC, Wei YF, Ruben SM, Carte KC, Rosen CA, Haseltine WA, Fleishmann RD, Fraser CM, Adams MD, Venter JC, Hamilton SR, Petersen P, Watson GM, Lynch HT, Peltomaki P, Mecklin JP, de la Chapelle A, Kinzler KW, Vogelstein B (1994) Mutation of a mutL homolog in hereditary colon cancer. Science 263:1625–1629
Haugen AC, Goel A, Yamada K, Marra G, Nguyen TP, Nagasaka T, Kanazawa S, Koike J, Kikuchi Y, Zhong X, Arita M, Shibuya K, Oshimura M, Hemmi H, Boland CR, Koi M (2008) Genetic instability caused by loss of MutS homologue 3 in human colorectal cancer. Cancer Res 68:8465–8472. doi:10.1158/0008-5472.CAN-08-0002
Koi M, Umar A, Chauhan DP, Cherian SP, Carethers JM, Kunkel TA, Boland CR (1994) Human chromosome 3 corrects mismatch repair deficiency and microsatellite instability and reduces N-methyl-N’-nitro-N-nitrosoguanidine tolerance in colon tumor cells with homozygous hMLH1 mutation. Cancer Res 54:4308–4312
Jacob S, Aguado M, Fallik D, Praz F (2001) The role of the DNA mismatch repair system in the cytotoxicity of the topoisomerase inhibitors camptothecin and etoposide to human colorectal cancer cells. Cancer Res 61:6555–6562
Marra G, Iaccarino I, Lettieri T, Roscilli G, Delmastro P, Jiricny J (1998) Mismatch repair deficiency associated with overexpression of the MSH3 gene. Proc Natl Acad Sci USA 95:8568–8573
Tentori L, Leonetti C, Scarsella M, D’Amati G, Vergati M, Portarena I, Xu W, Kalish V, Zupi G, Zhang J, Graziani G (2003) Systemic administration of GPI 15427, a novel poly(ADP-ribose) polymerase-1 inhibitor, increases the antitumor activity of temozolomide against intracranial melanoma, glioma, lymphoma. Clin Cancer Res 9:5370–5379
Yamane K, Taylor K, Kinsella TJ (2004) Mismatch repair-mediated G2/M arrest by 6-thioguanine involves the ATR-Chk1 pathway. Biochem Biophys Res Commun 318:297–302
Rottenberg S, Jaspers JE, Kersbergen A, van der Burg E, Nygren AO, Zander SA, Derksen PW, de Bruin M, Zevenhoven J, Lau A, Boulter R, Cranston A, O’Connor MJ, Martin NM, Borst P, Jonkers J (2008) High sensitivity of BRCA1-deficient mammary tumors to the PARP inhibitor AZD2281 alone and in combination with platinum drugs. Proc Natl Acad Sci USA 105:17079–17084. doi:10.1073/pnas.0806092105
Zhu G, Chang P, Lippard SJ (2010) Recognition of platinum-DNA damage by poly(ADP-ribose) polymerase-1. Biochemistry 49:6177–6183. doi:10.1021/bi100775t
Vilar E, Bartnik CM, Stenzel SL, Raskin L, Ahn J, Moreno V, Mukherjee B, Iniesta MD, Morgan MA, Rennert G, Gruber SB (2011) MRE11 deficiency increases sensitivity to poly(ADP-ribose) polymerase inhibition in microsatellite unstable colorectal cancers. Cancer Res 71:2632–2642. doi:10.1158/0008-5472.CAN-10-1120
Oplustilova L, Wolanin K, Mistrik M, Korinkova G, Simkova D, Bouchal J, Lenobel R, Bartkova J, Lau A, O’Connor MJ, Lukas J, Bartek J (2012) Evaluation of candidate biomarkers to predict cancer cell sensitivity or resistance to PARP-1 inhibitor treatment. Cell Cycle 11:3837–3850. doi:10.4161/cc.22026
Gottipati P, Vischioni B, Schultz N, Solomons J, Bryant HE, Djureinovic T, Issaeva N, Sleeth K, Sharma RA, Helleday T (2010) Poly(ADP-ribose) polymerase is hyperactivated in homologous recombination-defective cells. Cancer Res 70:5389–5398. doi:10.1158/0008-5472.CAN-09-4716
Acknowledgments
This work was supported by a grant from the Italian Ministry of Education and Research, “Programmi di ricerca scientifica di Rilevante Interesse Nazionale” (PRIN) project to LT. A.M. is recipient of a fellowship from “Regione Lazio-Filas”. The funders had no role in study design, data collection and analysis, or preparation of the manuscript.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
280_2013_2175_MOESM1_ESM.pptx
Fig. S1 Analysis of apoptosis and cell cycle in MLH1-deficient and MLH1-proficient HCT116 cells treated with oxaliplatin. Cells were exposed to 1.2 and 2.5 μM oxaliplatin (Oxa) and analysed by flow cytometry at 72 h after treatment. The percentages of apoptotic cells are indicated. The percentages of MLH1-deficient cells in the different phases of cell cycle are as follows: Ctr, G1 41%, S 42%, G2/M 17%; Oxa 1.2 μM, G1 56%, S 17%, G2/M 27%; Oxa 2.5 μM, G1 52%, S 13%, G2/M 35%. The percentages of MLH1-proficient cells in the different phases of cell cycle are as follows: untreated control (Ctr), G1 54%, S 29%, G2/M 17%; Oxa 1.2 μM, G1 56%, S 7%, G2/M 37%; Oxa 2.5 μM, G1 52%, S 6%, G2/M 42% (PPTX 307 kb)
280_2013_2175_MOESM2_ESM.pptx
Fig. S2 Cell cycle analysis of HCT116+3 and HCT116+3+5 cells treated with PARPi. HCT116+3 and HC116+3+5 cells were exposed to GPI 15427 (5 μM) and analysed by flow cytometry at 72 h after treatment. The percentages of cells in the different phases of cell cycle are as follows: HCT116+3, Ctr, G1 52%, S 32%, G2/M 16%; HCT116+3, PARPi, G1 53%, S 29%, G2/M 18%; HCT116+3+5, Ctr, G1 54%, S 24%, G2/M 22%; HCT116+3+5, PARPi, G1 52%, S 22%, G2/M 26% (PPTX 121 kb)
Rights and permissions
About this article
Cite this article
Tentori, L., Muzi, A., Dorio, A.S. et al. MSH3 expression does not influence the sensitivity of colon cancer HCT116 cell line to oxaliplatin and poly(ADP-ribose) polymerase (PARP) inhibitor as monotherapy or in combination. Cancer Chemother Pharmacol 72, 117–125 (2013). https://doi.org/10.1007/s00280-013-2175-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-013-2175-0