Abstract
Objective
The anticancer drug docetaxel is extensively metabolized by cytochrome P450 (CYP) 3A isozymes. Furthermore, docetaxel is also a substrate for the transmembrane ATP-binding cassette efflux transporter protein ABCB1. CYP3A-inhibition significantly reduces docetaxel total systemic clearance, on average by 50%. However, data on the effect of CYP3A-inhibition on the fecal and urinary excretion of docetaxel are lacking. To further elucidate the role of CYP3A- and ABCB1-mediated elimination pathways for docetaxel we investigated the effect of the potent CYP3A-inhibitor, and also ABCB1-inhibitor, ketoconazole on the fecal and urinary disposition of docetaxel in cancer patients.
Methods
Fifteen patients were treated with docetaxel (100 mg/m2), followed 3 weeks later by a reduced dose in combination with orally administered ketoconazole, or vice versa. Six patients were also administered [3H]-radiolabeled docetaxel. Fecal and urinary specimens, collected up to 72-h post-infusion, were analyzed for cumulative parent drug and radioactivity excretion.
Results
Ketoconazole coadministration increased fecal parent drug excretion twofold from 2.6 ± 2.8 to 5.2 ± 5.4% (mean ± SD, P = 0.03) but did not affect urinary parent drug excretion (P = 0.69). The sum of fecal and urinary parent drug excretion was 5.3 ± 3.0% for docetaxel alone and 7.8 ± 5.6% in the presence of ketoconazole, respectively (P = 0.04). Total recovered radioactivity values were 45.8 ± 19.1 and 32.4 ± 19.7%, respectively (P = 0.23).
Conclusion
CYP3A-inhibition by ketoconazole increases fecal parent drug excretion twofold in cancer patients. A more pronounced increase was not achieved, most likely due to concomitant intestinal ABCB1-inhibition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, the clinical pharmacokinetics (PK) of the anticancer drug docetaxel has been subject of thorough investigation. After intravenous administration the drug is extensively metabolized by hepatic and intestinal cytochrome P450 (CYP) isozymes 3A [1, 2], the catalytic activity of which is represented by two major isoforms, CYP3A4 and CYP3A5, albeit that CYP3A4 is the most active, possesses the highest affinity for docetaxel [3] and is predominant in Caucasians [4]. Moreover, CYP3A activity is readily induced or inhibited by a broad range of compounds. Docetaxel is also a substrate for the ATP-binding cassette membrane-localized transporter, ABCB1 (P-glycoprotein; MDR-1) which acts as a (drug/xenobiotic-)efflux pump [5, 6], ABCB1 is expressed in several tissues including the renal tubule, biliary tract and intestinal epithelium [7] and plays a prominent role in the fecal elimination of docetaxel [8, 9].
Preclinical studies with [14C]-radiolabeled docetaxel have demonstrated that administered radioactivity is predominately (85–95%) excreted in the feces within 7 days and that urinary excretion accounts for less than 5% [10–12]. Furthermore, the administered dose is primarily (≥75%) excreted as four pharmacologically inactive metabolites [13] and less than 10% is excreted unchanged [14]. Clinical studies assessing excretion of [14C]-radiolabeled docetaxel are limited; in cancer patients (N = 3) approximately 80% of total administered radioactivity was excreted in feces collected up to 7 days post-infusion and 5% of total radioactivity was recovered in urine [15].
The fecal disposition of docetaxel in the presence of ABCB1-inhibition has been studied previously [8], however, the effect of inhibition of CYP3A, the drug’s major route of inactivation, on docetaxel fecal and urinary excretion, has never yet been evaluated. We previously studied the effect of concomitant orally administered ketoconazole, a potent CYP3A-inhibitor [16] and also weak to modest ABCB1-inhibitor [7, 17, 18], on docetaxel plasma PK in cancer patients [19, 20]. Subsequently, the current study was undertaken to evaluate, for the first time, the effect of both CYP3A- and ABCB1-inhibition on docetaxel fecal and urinary excretion. The objectives of the current study were therefore to evaluate the influence of ketoconazole on (1) the fecal and urinary excretion of unchanged docetaxel (parent drug), on (2) the total fecal and urinary excretion of docetaxel using [3H]-radiolabeled docetaxel and on (3) the mass balance of ([3H]-radiolabeled-)docetaxel.
Wide variation in total CYP3A activity exists, as reflected by substantial interindividual PK variability for CYP3A substrates [21]. Part of this variability has been related to genetic diversity in the genes encoding CYP3A4 and CYP3A5 proteins [22]. However, currently, most evidence infers that it is unlikely that CYP3A4 single nucleotide polymorphisms (SNPs) contribute substantially to variability in CYP3A4 activity in vivo [23–25] due to the low frequency of genetic polymorphisms. On the other hand, more than 80% of Caucasians is deficient in CYP3A5 activity due to the CYP3A5*3C/*3C variant genotype [4]. In individuals with at least one CYP3A5*1 allele, CYP3A5 may account for at least 50% of total CYP3A content, resulting in two to threefold higher CYP3A activity in vitro [26]. Moreover, CYP3A4 and CYP3A5 show distinct differences in susceptibility to inhibition by ketoconazole [27]. ABCB1 polymorphisms have not been shown to affect docetaxel plasma PK [28, 29], yet their influence on fecal and urinary excretion is unknown. We included CYP3A5 and ABCB1 genotyping in our study to gain insight in the effect of the various SNPs on docetaxel fecal and urinary excretion. Genotyping for CYP3A4 rare polymorphisms was performed to exclude genetic diversity in CYP3A4 activity.
We here report on the disposition of docetaxel in the feces and urine of cancer patients, after intravenous administration of the drug with and without concomitant oral administration of ketoconazole, a potent inhibitor of the drug’s major route of inactivation.
Methods
Patient selection and study design
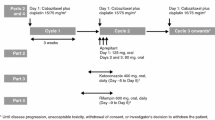
Eligibility criteria and study design have been reported previously [19, 20]. Briefly, cancer patients for whom no other treatment was available were treated with two courses of docetaxel administered as a 1-h intravenous infusion once every 3-weeks. Initially, one course was given at a dose of 100 mg/m2 and the other at a dose of 10 mg/m2 in combination with three 200-mg doses of ketoconazole, orally administered once every 24 h up to 47 h after docetaxel infusion (standard-dose ketoconazole) [30]. Seven patients were treated accordingly followed by plasma PK analysis. We observed wide variability in the reduction of docetaxel total clearance [19], which was attributed to variability in systemic ketoconazole exposure. We subsequently treated patients with a higher ketoconazole dose (400-mg every 8 h, up to 47 h after docetaxel infusion, i.e. a total of seven doses of 400-mg ketoconazole; high-dose ketoconazole) [31] in combination with docetaxel (15 mg/m2) [20]. We hypothesized that an increase in ketoconazole dose would result in sufficiently high ketoconazole exposure in each patient and thus in maximum CYP3A-inhibition overall, thereby reducing the variability in the extent to which docetaxel clearance is reduced. In addition, we administered a tracer-dose of [3H]-radiolabeled docetaxel to each patient for radioactivity measurements in feces and urine, in the absence and presence of high-dose ketoconazole. The study protocol was approved by the Erasmus MC Investigational Review Committee and all patients gave written informed consent for participation.
Chemicals
Tritiated [3H]-docetaxel (1.0 mCi/mL in ethanol, specific activity 7.2 Ci/mmol; Moravek Biochemicals, Brea, CA, USA) and 5 mL aliquots of a 200-fold dilution in ethanol absolute (>99.9%; Merck, Darmstadt, Germany) were stored at −80°C prior to adding to unlabeled docetaxel diluted in 250 mL 0.9% (w/v) sodium chloride solution. Purity of [3H]-docetaxel was analyzed by a reversed-phase high performance liquid chromatography (HPLC) method with UV-detection at 230 nm [32]. The elution profile of the recovered radioactivity was compared to the chromatographic profile of unlabeled docetaxel; the product showed no signs of degradation or decreased purity [33].
Sample collection
During both courses, complete stool collections were obtained up to 72 h post-infusion and stored at −80°C until processing. Subsequently, weighted feces samples were homogenized in three volumes (1:3 w/v) of phosphate buffered saline solution (PBS - Oxoid, Basingstoke, UK) using an Ultra-TurraxT25 homogenizer (Janke&Kunkel, IKA®Labortechnik, Staufen, Germany) operating at 20,500 rpm and then stored at −80°C prior to radioactivity measurements. Aliquots of feces homogenates were further diluted (up to fivefold) with PBS and stored at −80°C prior to chromatographic analysis. All voided urine was collected quantitatively during three intervals post-infusion (0–24, 24–48, 48–72 h) and two portions from each interval were stored at −80°C prior to radioactivity measurements and chromatographic analysis.
Docetaxel analysis
Docetaxel was quantitated in feces and urine samples using HPLC with tandem mass-spectrometric detection (LC-MS/MS). Prior to extraction all samples were diluted at volume ratios of at least 1:1 up to 1:50 with analyte-free lithium-heparinized human plasma. Hereafter, 100 μL aliquots of the diluted feces or urine sample were processed and analyzed as described previously [20]. Docetaxel feces and urine concentrations were quantitated over the range of 5.00–500 ng/mL. For quantitation of docetaxel in the patient samples, quality control (QC) samples at docetaxel concentrations of 5.00, 15.0, 400 and 6,000 ng/mL, the latter QC diluted 20-fold prior to processing, were assayed in duplicate and distributed among the calibrators and samples in the analytical run. Finally, given the volume of collected urine and the weight of the collected feces samples, the absolute amount of docetaxel excreted in each urine and feces specimen was calculated assuming that 1 g unhomogenized feces equals 1 mL.
Radioactivity measurements
Details of the development and validation of the analytical method used to quantitate radioactivity levels in feces and urine have been reported elsewhere [33]. Briefly, the radionuclide fraction of [3H] was obtained after complete combustion of a known amount of sample aliquot (undiluted urine and 1:3 w/v diluted feces) in a closed-type combustion flask of known weight, thus yielding a known amount of tritiated combustion water, [3H]2O. Subsequently, liquid scintillation (LS) cocktail was added to a quantitatively taken amount of [3H]2O, the solution then mixed until homogeneous and the samples counted in a LS-counter. Finally, based on the amount of radioactivity in the produced [3H]2O, the excreted radioactivity in the combusted samples was determined and thus the total amount of recovered radioactivity in the collected feces and urine specimens. As [3H]-radiolabeled docetaxel is metabolized and eliminated identically to unlabeled drug, the recovered radioactivity reflects the sum of radioactivity from excreted parent drug and all excreted metabolites.
Genotype analysis
Polymerase chain reaction (PCR)-restriction fragment length polymorphism analysis for CYP3A5*3C, CYP3A5*6, CYP3A4*1B, CYP3A4*3, CYP3A4*17, CYP3A4*18A and ABCB1 3435C > T variant alleles was performed as described previously [4, 34, 35]. Based on allele frequencies in the Caucasian population, in which the CYP3A5*3C allele is the predominant allele, the rare CYP3A5*6 variant allele, which also results in completely or severely decreased CYP3A5 activity was only determined for individuals with no, or only one CYP3A5*3C allele (i.e. with apparently at least one CYP3A5*1 allele).
Statistical considerations
Excretion parameters are reported as mean values ± SD unless stated otherwise. The difference in parameters between the two courses was evaluated statistically using a non-parametric two-tailed, Wilcoxon signed rank test for paired observations after testing for period effects. Mean (±SD) urinary parent drug excretion values for the standard- and high-dose ketoconazole patient-groups were 2.2% (±0.95) and 3.0% (±1.09), respectively. Mean (±SD) fecal parent drug excretion values for the standard- and high-dose ketoconazole patient-groups were 5.5% (±5.41) and 4.8% (±5.77), respectively. Subsequent comparison of the mean urinary and fecal parent drug excretion (in the presence of ketoconazole) between the standard- and high-dose ketoconazole patient-groups showed no significant differences (P = 0.17 and P = 0.95 respectively, Mann–Whitney U-test). Furthermore, the extent to which docetaxel total clearance was reduced was almost identical for high- and standard-dose ketoconzole treatment [19, 20] suggesting that the increase in ketoconazole dose did not augment the extent of CYP3A-inhibition. Therefore, the excretion data of all patients were evaluated together, irrespective of ketoconazole dose. The significance level was set at P < 0.05. Statistical calculations were performed with SPSS version 11.5 (Chicago, IL, USA).
Results
Baseline patient profiles
A total of 15 Caucasian patients were included (standard-dose ketoconazole, N = 7; high-dose ketoconazole, N = 8). For all patients urine samples were collected during both courses. For one patient (high-dose ketoconazole group) no feces samples were collected, thus feces samples were available for 14 patients during both courses. None of the patients were administered CYP3A- inducing or inhibiting co-medication, however two patients were administered medication known to reduce ketoconazole gastro-intestinal absorption (pantoprazole and ranitidine), thus (potentially) decreasing systemic ketoconazole exposure [36]. For the patient administered pantoprazole (and high-dose ketoconazole) ketoconazole exposure (area under the concentration-time curve, AUC) was approximately fourfold higher than median exposure (AUC = 60.1 mg × h/L; range 19.6–81.3 mg × h/L) for patients treated with standard-dose ketoconazole (without interfering medication). As previously discussed, we did not observe a significant difference in docetaxel urinary and fecal excretion in the presence of ketoconazole between standard- or high-dose ketoconazole, therefore this patient was included in our analysis. Of note, this was also the patient for whom no feces samples were available. For the patient administered ranitidine (and standard-dose ketoconazole), ketoconazole exposure was indeed the lowest (AUC = 12.8 mg × h/L), yet differed only marginally from the exposure (AUC = 19.6 mg × h/L) for another patient not administered interfering co-medication. Furthermore, for this patient, fecal parent drug excretion in the presence of ketoconazole was increased by 44% suggesting an inhibitory effect of ketoconazole. We therefore also included this patient in our analysis. Thus, 15 patients were evaluable for cumulative urinary parent drug excretion-analysis and 14 for cumulative fecal parent drug excretion-analysis. Urine and feces samples for radioactivity measurements were available for six and five patients, respectively, in the absence and presence of high-dose ketoconazole. Table 1 summarizes the baseline characteristics for the evaluable patients.
All patients were genotyped for CYP3A5*3C, CYP3A4*1B, CYP3A4*3, CYP3A4*17 and CYP3A4*18A variant alleles. Fourteen patients were homozygous for the CYP3A5*3C variant allele, and consequently deficient in CYP3A5 activity, indicating that for these patients total hepatic and intestinal CYP3A activity is solely attributable to CYP3A4 activity. Only CYP3A5 (not CYP3A4) is expressed to any significant degree in renal tubular epithelial cells [37]. Thus for the CYP3A5*3C homozygous individuals, any effect of ketoconazole on urinary parent drug excretion cannot be attributed to CYP3A(5)-inhibition. One patient carried a single CYP3A5*1 allele, yet not the CYP3A5*6 variant allele, indicating that in this patient CYP3A5 is (most probably) active. This same patient was the only heterozygous carrier of the CYP3A4*1B variant allele (*1A/*1B). All other patients were homozygous CYP3A4*1A/*1A. No patients carried variant alleles for CYP3A4*3, CYP3A4*17 or CYP3A4*18A. ABCB1 3435C > T genotyping results were available for 13 patients. The genotype distribution was one homozygous wild-type patient (C/C), eight heterozygous variant patients (C/T) and four homozygous variant patients (T/T).
Fecal and urinary parent drug excretion
A summary of the cumulative excretion of parent drug in feces and urine collected up to 72 h post-infusion during both courses is listed in Tables 2 and 3. Data are reported as total fraction (i.e. percentage) of the administered absolute docetaxel dose which is excreted unchanged in the feces (fef,%) or urine (feu,%). After single agent dosing a minor fraction of the administered docetaxel dose was recovered in the feces unchanged (2.6 ± 2.8%). Total fecal parent drug excretion was approximately twofold higher in the presence of ketoconazole (5.2 ± 5.4%, P = 0.03). We observed a trend toward statistical significance when the fecal parent drug excretion in the absence and presence of ketoconazole was evaluated for each 24-h interval (0–24 h, P = 0.87, N = 7; 24–48 h, P = 0.52, N = 9; 48–72 h, P = 0.03, N = 6). Fecal specimens were not available for every patient in each 24-h interval, explaining why the number of patients included in these sub-analyses is less than the 14 evaluable patients. Furthermore, this also explains why the sum of the average fraction of parent drug excreted during each 24-h period does not equal the total cumulative fecal parent drug excretion (0–72 h).
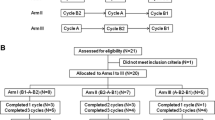
Figure 1a shows the cumulative fecal parent drug excretion in the absence of ketoconazole as a function of CYP3A4*1B, CYP3A5*3C and ABCB1 3435C > T genotype. Mean fecal parent drug excretion for the CYP3A5*3C and CYP3A4*1A homozygous patients was 2.6 and 2.4% for the single CYP3A5*3C and CYP3A4*1B heterozygous patient. The genotype distribution (13 vs. 1) does not allow statistical evaluation, however, these data do not suggest a substantial difference in fecal excretion for the evaluated genotypes. Mean fecal parent drug excretion for the C/T and T/T ABCB1 genotypes was 2.6 and 4.2%, respectively (P = 0.85). Fecal excretion for the patient with C/C genotype was 1.3%.
Box plots of the percentage cumulative fecal parent drug excretion (a) and cumulative urinary parent drug excretion (b) as a function of CYP3A5*3C, CYP3A4*1B and ABCB1 C3435T genotype; (1) denotes CYP3A5*3C homozygous variant allele carriers and patients carrying no CYP3A4*1B variant allele (i.e. CYP3A4*1A/*1A, N = 14); (2) denotes CYP3A5*3C heterozygous variant allele carriers and CYP3A4*1B heterozygous variant allele carriers (N = 1); C/C denotes ABCB1 homozygous wild-type allele carriers (N = 1), C/T denotes patients carrying one variant allele (N = 8) and T/T denotes homozygous variant allele carriers (N = 4). The box represents the difference between the 25th and 75th percentiles (i.e. the interquartile range), whereas the horizontal line inside the box represents the median. Open circles are defined as outliers. Whiskers are drawn from the ends of the box to the largest and smallest values that are not outliers
The cumulative urinary parent drug excretion did not differ significantly between the two courses (P = 0.69) and renal parent drug excretion predominantly (>80%) took place during the first 24 h post-infusion regardless of ketoconazole administration (Table 3). The ratio of the fraction of parent drug excreted during the first 24 h to the total fraction of excreted parent drug (feu0–24 h:feu0–72 h) was significantly lower in the presence of ketoconazole (P = 0.02, N = 15). This was also the case when we evaluated this ratio for patients administered high-dose ketoconazole separately (P = 0.01), yet not for patients administered standard-dose ketoconazole (P = 0.93).
Figure 1b shows the cumulative urinary parent drug excretion in the absence of ketoconazole as a function of CYP3A4*1B, CYP3A5*3C and ABCB1 3435C > T genotype. Mean urinary parent drug excretion for the CYP3A5*3C and CYP3A4*1A homozygous patients was 2.6 and 2.8% for the CYP3A5*3C and CYP3A4*1B heterozygous individual, again not suggesting a substantial difference between the evaluated genotypes. Mean urinary parent drug excretion for the C/T and T/T ABCB1 genotypes was 2.8 and 1.7%, respectively, (P = 0.04). Urinary excretion for the patient with C/C genotype was 5.2%.
Radioactivity recovered in feces and urine
A summary of the cumulative radioactivity recovered in feces (Raf,%) and urine (Rau,%) samples collected up to 72 h post-infusion during both treatments is listed in Table 4. Mean cumulative fecal excretion of radioactivity was lower in the presence of ketoconazole (27.7% vs. 40.4%), but this difference was not significant (P = 0.23). Mean fecal parent drug excretion in the presence and absence of ketoconazole was 6.7 and 3.3% (for these five patients), respectively, suggesting that the fraction of excreted metabolites in the presence and absence of ketoconazole was 21.0 and 37.1%, respectively (P = 0.14). We evaluated the influence of ketoconazole on the ratio of fecal parent drug excretion to fecal excretion of parent drug and all metabolites, the latter reflected by cumulative radioactivity excretion. This ratio (fef:Raf) was significantly higher (P = 0.04) in the presence of ketoconazole (0.26 ± 0.09) compared to single agent docetaxel (0.10 ± 0.05), confirming the observed increased parent drug excretion.
The total fraction of radioactivity recovered in urine did not differ significantly between the two courses (P = 0.17). For both courses, the percentage of urinary recovered radioactivity is approximately 2% higher than cumulative urinary parent drug excretion, suggesting that approximately 2% of the administered docetaxel dose is eliminated renally as metabolite(s). The ratio of the cumulative fraction of radioactivity recovered in urine during the first 24 h to the total fraction of urinary excreted radioactivity (ratio Rau0–24 h:Rau0–72 h) was significantly lower in the course with ketoconazole (P = 0.03). In contrast to the fecal excretion data, ketoconazole did not influence the ratio of urinary parent drug excretion to urinary excretion of parent drug and all metabolites (feu:Rau; P = 0.27).
Mass balance
The mass balances of excreted parent drug and recovered radioactivity (determined by adding the cumulative fecal and urinary excretion data) for each course are summarized in Table 5. For parent drug total cumulative excretion is significantly higher in the presence of ketoconazole (P = 0.04). The mass balance of recovered radioactivity was lower in the course with ketoconazole, yet the difference was not significant (P = 0.23).
Mean cumulative total parent drug excretion for the CYP3A5*3C and CYP3A4*1A homozygous patients was 5.3 and 5.2% for the CYP3A5*3C and CYP3A4*1B heterozygous individual. Mean cumulative total parent drug excretion for the C/T and T/T ABCB1 genotypes was 5.5 and 5.8%, respectively (P = 1.0). Cumulative total parent drug excretion for the patient with C/C genotype was 6.5%.
Discussion
Although docetaxel plasma PK in cancer patients is well characterized, data on the fecal and urinary excretion of the drug are limited. In this study we evaluated the fecal and urinary excretion of docetaxel parent drug and [3H]-radiolabeled docetaxel in cancer patients, after intravenous docetaxel administration with and without concomitant orally administered ketoconazole, a potent inhibitor of CYP3A-mediated metabolism, the drug’s major route of inactivation and also a (weak to modest) inhibitor of ABCB1, which plays an important role in the fecal disposition of docetaxel [8, 9]. Assessing purposeful modulation of docetaxel fecal and urinary disposition can contribute to a better overall understanding of the mechanistic aspects involved in docetaxel metabolism. Recently, hepatic CYP3A-induction in vitro led to CYP2C8-mediated formation of a previously unidentified docetaxel metabolite [38]. Furthermore, preliminary data indicate that renal function (creatinine clearance) is the most significant predictor of docetaxel clearance in the presence of ketoconazole (Pearson’s correlation coefficient, R = 0.484; P = 0.002) [39], which is in contrast with single agent treatment where hepatic function is a significant predictor of docetaxel clearance [40, 41].
In the absence of ketoconazole, fecal parent drug excretion was consistent with previous findings [9] and approximately twofold increased in the presence of ketoconazole. The relative contribution of ABCB1-inhibition is quantitatively less significant than the contribution of CYP3A-inhibition to the overall effect of ketoconazole-mediated drug interactions [7, 17, 18]. Thus, the here observed drug-interaction should primarily be attributed to CYP3A-inhibition, however the influence of concomitant ABCB1-inhibition should not be overlooked. In the presence of a selective ABCB1-inhibitor re-absorption of docetaxel parent drug from the intestinal lumen (following biliary secretion) is a very efficient process and subsequent CYP3A-mediated metabolism in the liver and intestinal mucosa consequently leads to a marked reduction in fecal parent drug excretion [8, 9]. If theoretically, ketoconazole was to act only as a selective CYP3A-inhibitor, adequate ABCB1-mediated efflux of parent drug into the intestinal lumen would not be impaired. Consequently, due to ketoconazole-mediated selective CYP3A-inhibition, one would expect the administered docetaxel dose to be excreted predominantly as parent drug. Concomitant ketoconazole-mediated ABCB1-inhibition most likely explains why we did not observe a more marked increase in fecal parent drug excretion in the presence of ketoconazole (Fig. 2: a schematic representation of the role of hepatic CYP3A and intestinal ABCB1 in docetaxel metabolism and excretion and the inhibitory effect of ketoconazole). Interestingly, we observed a trend toward a statistically significant difference in fecal parent drug excretion in the presence and absence of ketoconazole as the time-interval post-infusion increased. The effect of ABCB1-inhibition is expected to be most pronounced shortly after ketoconazole administration due to high local drug concentrations in the gut, and to decrease over time, such that in the 48–72 h interval, when no ketoconazole was administered, the (relative) contribution of ketoconazole-mediated CYP3A-inhibition is more pronounced than in the 0–24 h interval.
Schematic representation of the role of hepatic CYP3A and intestinal ABCB1 in docetaxel metabolism and elimination in humans and ketoconazole-mediated inhibition. a Model of the hepatic-cellular plate showing the bile collecting system with (1) inhibition by ketoconazole (depicted by a cross) of cytochrome P450 3A isozyme-mediated hepatic metabolism of docetaxel from the systemic circulation or the portal vein after re-absorption following biliary secretion and (2) its subsequent secretion in the terminal bile duct. b Model of the intestinal epithelium showing (1) re-uptake of docetaxel into the intestinal lumen, (2) ABCB1-mediated efflux of docetaxel and its inhibition by ketoconazole (depicted by a cross) and (3) intestinal metabolism by the cytochrome P450 3A enzyme system and its inhibition by ketoconazole (depicted by a cross). Abbreviations: ABCB, ABCB1; doc, docetaxel; keto, ketoconazole; M, docetaxel metabolite M4; CYP3A, enzymes of the cytochrome P450 family, isoform 3A
A second consequence of temporarily inhibiting CYP3A-mediated metabolism is a reduction in the fraction of formed metabolites. The difference between fecal recovered radioactivity (i.e. parent drug and all excreted metabolites) and fecal parent drug excretion reflects the fecal excretion of metabolites. We observed a lower fraction of excreted metabolites in the presence of ketoconazole (21.0 vs. 37.1%), although the difference was not statistically significant (P = 0.14). The lack of significance is possibly also a consequence of concomitant ABCB1-inhibition or because alternative routes of metabolism then prevail or due to our limited sample size (N = 5).
The cumulative fraction of fecal recovered radioactivity was not significantly lower in the presence of ketoconazole (P = 0.23). This is in line with the concept of mass conservation, stating that (tritium-labeled) mass is neither created nor destroyed during a chemical reaction, i.e. metabolism. Thus, despite CYP3A-inhibition, the total fraction of excreted parent drug and all metabolites (i.e. recovered radioactivity) should not differ between the two courses.
Urinary excretion plays a minor role in the elimination of docetaxel. We determined urinary parent drug excretion and urinary excretion of metabolites each to be approximately 2%. Interestingly, substantially increasing the ketoconazole dose significantly reduced parent drug excretion during the first 24 h post-infusion relative to total parent drug excretion (ratio feu0–24 h:feu0–72 h). This effect is most likely attributable to ketoconazole-mediated ABCB1-inhibition as, with the exception of one, all patients were deficient in renal CYP3A(5) activity. Ketoconazole-mediated inhibition of ABCB1 transport function is concentration dependant [42], therefore it is likely that the higher ketoconazole dose effectively inhibits ABCB1 localized on the apical surface of renal tubular epithelial cells [43] thereby limiting ABCB1-mediated renal parent drug secretion. Again, (the effect of) renal ABCB1-inhibition seems most pronounced shortly after ketoconazole administration. However, ketoconazole-mediated ABCB1-inhibition was not marked enough to affect the cumulative urinary elimination of docetaxel.
The mass balance for cumulative parent drug excretion was increased upon concomitant ketoconazole administration, yet not as marked as one may have expected, due to the discussed influence of concomitant intestinal ABCB1-inhibition. The mass balance for the fraction of recovered radioactivity, although lower in the presence of ketoconazole, did not differ significantly between the two courses, due to abovementioned reasons.
To our knowledge, the fecal and urinary excretion of docetaxel has not previously been evaluated as function of genotype. As our patient group was limited in size we only tentatively correlated parent drug excretion (in the absence of ketoconazole) to genotype. The mean cumulative fecal excretion for patients carrying the ABCB1 T/T genotype was more than threefold that observed for the (single) patient with the C/C genotype which is consistent with data suggesting higher expression of intestinal ABCB1 for the T/T genotype [44]. Interestingly, the observed higher fecal excretion for homozygous variant allele carriers (T/T) compared to the homozygous wild-type (C/C) patient is inversed for urinary excretion and could be a reflection of different ABCB1 3435C > T expression among tissues [44, 45].
We are aware of several limitations in our study; (1) the number of patients was limited, especially the sub-group administered [3H]-radiolabeled docetaxel, yet more than in previous excretion studies using radiolabeled docetaxel; [15] (2) specimens were collected up to 72 h post-infusion, the period of hospital admission; ideally specimens should be collected up to 7 days post-infusion yet this poses practical and logistical difficulties; (3) although patients consented to collection of all fecal and urinary specimens, it is possible that collection is not complete; (4) we did not analyze the fecal and urinary excretion of the major metabolites due to unavailability of reference compounds and (5) it is likely that by assuming that 1 g unhomogenized feces is equivalent to 1 mL, we have underestimated the cumulative fecal excretion. However, despite these limitations, this study has further elucidated the elimination pathways of docetaxel. Moreover, to the best of our knowledge, for the first time fecal and urinary excretion of docetaxel were evaluated after temporarily inhibiting the drug’s major route of inactivation.
References
Marre F, Sanderink GJ, de Sousa G, Gaillard C, Martinet M, Rahmani R (1996) Hepatic biotransformation of docetaxel (Taxotere) in vitro: involvement of the CYP3A subfamily in humans. Cancer Res 56:1296–1302
Royer I, Monsarrat B, Sonnier M, Wright M, Cresteil T (1996) Metabolism of docetaxel by human cytochromes P450: interactions with paclitaxel and other antineoplastic drugs. Cancer Res 56:58–65
Shou M, Martinet M, Korzekwa KR, Krausz KW, Gonzalez FJ, Gelboin HV (1998) Role of human cytochrome P450 3A4 and 3A5 in the metabolism of taxotere and its derivatives: enzyme specificity, interindividual distribution and metabolic contribution in human liver. Pharmacogenetics 8:391–401
van Schaik RH, van der Heiden IP, van den Anker JN, Lindemans J (2002) CYP3A5 variant allele frequencies in Dutch Caucasians. Clin Chem 48:1668–1671
Ringel I, Horwitz SB (1991) Studies with RP 56976 (taxotere): a semisynthetic analogue of taxol. J Natl Cancer Inst 83:288–291
Shirakawa K, Takara K, Tanigawara Y, Aoyama N, Kasuga M, Komada F, Sakaeda T, Okumura K (1999) Interaction of docetaxel (“Taxotere”) with human P-glycoprotein. Jpn J Cancer Res 90:1380–1386
Lin JH (2003) Drug-drug interaction mediated by inhibition and induction of P-glycoprotein. Adv Drug Deliv Rev 55:53–81
van Zuylen L, Verweij J, Nooter K, Brouwer E, Stoter G, Sparreboom A (2000) Role of intestinal P-glycoprotein in the plasma and fecal disposition of docetaxel in humans. Clin Cancer Res 6:2598–2603
van Zuylen L, Sparreboom A, van der Gaast A, Nooter K, Eskens FA, Brouwer E, Bol CJ, de Vries R, Palmer PA, Verweij J (2002) Disposition of docetaxel in the presence of P-glycoprotein inhibition by intravenous administration of R101933. Eur J Cancer 38:1090–1099
Bruno R, Sanderink GJ (1993) Pharmacokinetics and metabolism of Taxotere (docetaxel). Cancer Surv 17:305–313
Gaillard C, Monsarrat B, Vuilhorgne M, Royer I, Monegier B, Sable S, Guenard C, Gires P, Archimbaud Y, Wright M, Sanderink GJ (1994) Docetaxel (Taxotere) metabolism in the rat in vivo and in vitro. Proc Am Assoc Cancer Res 35:2553a
Marlard M, Gaillard C, Sanderink GJ, Roberts S, Joannou P, Facchini V, Chapelle P, Frydman A (1993) Kinetics, distribution, metabolism and excretion of radiolabelled Taxotere (14C-RP56976) in mice and dogs. Proc Am Assoc Cancer Res 34:2343a
Sparreboom A, Van Tellingen O, Scherrenburg EJ, Boesen JJ, Huizing MT, Nooijen WJ, Versluis C, Beijnen JH (1996) Isolation, purification and biological activity of major docetaxel metabolites from human feces. Drug Metab Dispos 24:655–658
Bardelmeijer HA, Roelofs AB, Hillebrand MJ, Beijnen JH, Schellens JH, van Tellingen O (2005) Metabolism of docetaxel in mice. Cancer Chemother Pharmacol 56:299–306
de Valeriola D, Brassinne C, Gaillard C, Ketler JP, Tomiak E, Van Vreckem A, Fruhling J, Frydman A, Kerger J, Piccart M, Chapelle P, Blanc C (1993) Study of excretion balance, metabolism and protein binding of C14 radiolabelled Taxotere (TXT) (RP56976, NSC628503) in cancer patients. Proc Am Assoc Cancer Res 34:2221a
Venkatakrishnan K, Von Moltke LL, Greenblatt DJ (2001) Human drug metabolism and the cytochromes P450: application and relevance of in vitro models. J Clin Pharmacol 41:1149–1179
Wandel C, Kim RB, Kajiji S, Guengerich P, Wilkinson GR, Wood AJ (1999) P-glycoprotein and cytochrome P-450 3A inhibition: dissociation of inhibitory potencies. Cancer Res 59:3944–3948
Choo EF, Leake B, Wandel C, Imamura H, Wood AJ, Wilkinson GR, Kim RB (2000) Pharmacological inhibition of P-glycoprotein transport enhances the distribution of HIV-1 protease inhibitors into brain and testes. Drug Metab Dispos 28:655–660
Engels FK, Ten Tije AJ, Baker SD, Lee CK, Loos WJ, Vulto AG, Verweij J, Sparreboom A (2004) Effect of cytochrome P450 3A4 inhibition on the pharmacokinetics of docetaxel. Clin Pharmacol Ther 75:448–454
Engels FK, Mathot RA, Loos WJ, van Schaik RH, Verweij J (2006a) Influence of high-dose ketoconazole on the pharmacokinetics of docetaxel. Cancer Biol Ther 5:833–839
Lamba JK, Lin YS, Schuetz EG, Thummel KE (2002) Genetic contribution to variable human CYP3A-mediated metabolism. Adv Drug Deliv Rev 54:1271–1294
Ozdemir V, Kalowa W, Tang BK, Paterson AD, Walker SE, Endrenyi L, Kashuba AD (2000) Evaluation of the genetic component of variability in CYP3A4 activity: a repeated drug administration method. Pharmacogenetics 10:373–388
Baker SD, van Schaik RH, Rivory LP, Ten Tije AJ, Dinh K, Graveland WJ, Schenk PW, Charles KA, Clarke SJ, Carducci MA, McGuire WP, Dawkins F, Gelderblom H, Verweij J, Sparreboom A (2004) Factors affecting cytochrome P-450 3A activity in cancer patients. Clin Cancer Res 10:8341–8350
Floyd MD, Gervasini G, Masica AL, Mayo G, George AL Jr., Bhat K, Kim RB, Wilkinson GR (2003) Genotype-phenotype associations for common CYP3A4 and CYP3A5 variants in the basal and induced metabolism of midazolam in European- and African-American men and women. Pharmacogenetics 13:595–606
Lee SJ, Bell DA, Coulter SJ, Ghanayem B, Goldstein JA (2005) Recombinant CYP3A4*17 is defective in metabolizing the hypertensive drug nifedipine, and the CYP3A4*17 allele may occur on the same chromosome as CYP3A5*3, representing a new putative defective CYP3A haplotype. J Pharmacol Exp Ther 313:302–309
Kuehl P, Zhang J, Lin Y, Lamba J, Assem M, Schuetz J, Watkins PB, Daly A, Wrighton SA, Hall SD, Maurel P, Relling M, Brimer C, Yasuda K, Venkataramanan R, Strom S, Thummel K, Boguski MS, Schuetz E (2001) Sequence diversity in CYP3A promoters and characterization of the genetic basis of polymorphic CYP3A5 expression. Nat Genet 27:383–391
Gibbs MA, Thummel KE, Shen DD, Kunze KL (1999) Inhibition of cytochrome P-450 3A (CYP3A) in human intestinal and liver microsomes: comparison of Ki values and impact of CYP3A5 expression. Drug Metab Dispos 27:180–187
Puisset F, Chatelut E, Dalenc F, Busi F, Cresteil T, Azema J, Poublanc M, Hennebelle I, Lafont T, Chevreau C, Roche H (2004) Dexamethasone as a probe for docetaxel clearance. Cancer Chemother Pharmacol 54:265–272
Goh BC, Lee SC, Wang LZ, Fan L, Guo JY, Lamba J, Schuetz E, Lim R, Lim HL, Ong AB, Lee HS (2002) Explaining interindividual variability of docetaxel pharmacokinetics and pharmacodynamics in Asians through phenotyping and genotyping strategies. J Clin Oncol 20:3683–3690
Nizoral prescribing information. http://www.janssen.com
Figg WD, Liu Y, Acharya MR, Gulley J, Arlen PM, Lewis M, Parnes HL, Chen CC, Jones E, Dahut W (2003) A phase I trial of high dose ketoconazole plus weekly docetaxel in metastatic androgen independent prostate cancer. Proc Am Soc Clin Oncol 22:1731a
Loos WJ, Verweij J, Nooter K, Stoter G, Sparreboom A (1997) Sensitive determination of docetaxel in human plasma by liquid-liquid extraction and reversed-phase high-performance liquid chromatography. J Chromatogr B Biomed Sci Appl 693:437–441
Engels FK, Buijs D, Loos WJ, Verweij J, Bakker WH, Krenning EP (2006b) Quantification of [3H]docetaxel in feces and urine: development and validation of a combustion method. Anticancer Drugs 17:63–67
van Schaik RH, de Wildt SN, van Iperen NM, Uitterlinden AG, van den Anker JN, Lindemans J (2000) CYP3A4-V polymorphism detection by PCR-restriction fragment length polymorphism analysis and its allelic frequency among 199 Dutch Caucasians. Clin Chem 46:1834–1836
van Schaik RH, de Wildt SN, Brosens R, van Fessem M, van den Anker JN, Lindemans J (2001) The CYP3A4*3 allele: is it really rare? Clin Chem 47:1104–1106
Daneshmend TK, Warnock DW (1998) Clinical pharmacokinetics of ketoconazole. Clin Pharmacokinet 14:13–34
Dai Y, Iwanaga K, Lin YS, Hebert MF, Davis CL, Huang W, Kharasch ED, Thummel KE (2004) In vitro metabolism of cyclosporine A by human kidney CYP3A5. Biochem Pharmacol 68:1889–1902
Komoroski BJ, Parise RA, Egorin MJ, Strom SC, Venkataramanan R (2005) Effect of the St. John’s wort constituent hyperforin on docetaxel metabolism by human hepatocyte cultures. Clin Cancer Res 11:6972–6979
Tham LS, Goh BC, Wang LZ, Yong WP, Wong CI, Lee SC, Soo R, Sukri N, Lee HS (2006) Ketoconazole inhibition of CYP3A activity made midazolam but not docetaxel pharmaockinetics more predictable [abstract # PI-62] Proc Am Soc Clin Pharmacol Ther. Clin Pharmacol Ther 76:P23
Bruno R, Hille D, Riva A, Vivier N, ten Bokkel Huinnink WW, van Oosterom AT, Kaye SB, Verweij J, Fossella FV, Valero V, Rigas JR, Seidman AD, Chevallier B, Fumoleau P, Burris HA, Ravdin PM, Sheiner LB (1998) Population pharmacokinetics/pharmacodynamics of docetaxel in phase II studies in patients with cancer. J Clin Oncol 16:187–196
Bruno R, Vivler N, Vergniol JC, De Phillips SL, Montay G, Sheiner LB (1996) A population pharmacokinetic model for docetaxel (Taxotere): model building and validation. J Pharmacokinet Biopharm 24:153–172
Wang EJ, Lew K, Casciano CN, Clement RP, Johnson WW (2002) Interaction of common azole antifungals with P glycoprotein. Antimicrob Agents Chemother 46:160–165
Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I, Willingham MC (1987) Cellular localization of the multidrug-resistance gene product P-glycoprotein in normal human tissues. Proc Natl Acad Sci USA 84:7735–7738
Nakamura T, Sakaeda T, Horinouchi M, Tamura T, Aoyama N, Shirakawa T, Matsuo M, Kasuga M, Okumura K (2002) Effect of the mutation (C3435T) at exon 26 of the MDR1 gene on expression level of MDR1 messenger ribonucleic acid in duodenal enterocytes of healthy Japanese subjects. Clin Pharmacol Ther 71:297–303
Siegsmund M, Brinkmann U, Schaffeler E, Weirich G, Schwab M, Eichelbaum M, Fritz P, Burk O, Decker J, Alken P, Rothenpieler U, Kerb R, Hoffmeyer S, Brauch H (2002) Association of the P-glycoprotein transporter MDR1(C3435T) polymorphism with the susceptibility to renal epithelial tumors. J Am Soc Nephrol 13:1847–1854
Acknowledgments
The authors wish to thank the department of Nuclear Medicine, Erasmus MC – Daniel den Hoed Cancer Center for the use of their facilities and Dirk Buys in particular for his technical assistance during the radioactivity measurements. Conflict Of Interest Statement None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Engels, F.K., Loos, W.J., Mathot, R.A.A. et al. Influence of ketoconazole on the fecal and urinary disposition of docetaxel. Cancer Chemother Pharmacol 60, 569–579 (2007). https://doi.org/10.1007/s00280-006-0412-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-006-0412-5