Abstract
Recent years showed significant progress in the molecular characterization of the chronic myeloproliferative disorders (CMPD) which are classified according to the WHO classification of 2001 as polycythemia vera (PV), chronic idiopathic myelofibrosis (CIMF), essential thrombocythemia (ET), CMPD/unclassifiable (CMPD-U), chronic neutrophilic leukemia, and chronic eosinophilic leukemia (CEL)/hypereosinophilic syndrome, all to be delineated from BCR/ABL-positive chronic myeloid leukemia (CML). After 2001, the detection of the high frequency of the JAK2V617F mutation in PV, CIMF, and ET, and of the FIP1L1–PDGFRA fusion gene in CEL further added important information in the diagnosis of CMPD. These findings also enhanced the importance of tyrosine kinase mutations in CMPD and paved the way to a more detailed classification and to an improved definition of prognosis using also novel minimal residual disease (MRD) markers. Simultaneously, the broadening of therapeutic strategies in the CMPD, e.g., due to reduced intensity conditioning in allogeneic hematopoietic stem cell transplantation and the introduction of tyrosine kinase inhibitors in CML, in CEL, and in other ABL and PDGRFB rearrangements, increased the demands to diagnostics. Therefore, today, a multimodal diagnostic approach combining cytomorphology, cytogenetics, and individual molecular methods is needed in BCR/ABL-negative CMPD. A stringent diagnostic algorithm for characterization, choice of treatment, and monitoring of MRD will be proposed in this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic myeloproliferative disorders (CMPD) are clonal stem cell disorders encompassing a very heterogeneous complex of different entities which are defined by distinct clinical and cytomorphological phenotypes and, in some part, known genetic features. They are characterized by increased and effective proliferation of one to three hematopoietic cell lineages in the bone marrow associated to increased peripheral blood parameters. The recent detection of the high incidence of the JAK2 mutations in polycythemia vera (PV), chronic idiopathic myelofibrosis (CIMF), and essential thrombocythemia (ET) [1–5], the detection of the FIP1L1–PDGFRA gene fusion in chronic eosinophlilic leukemia (CEL) [6, 7], and the introduction of tyrosine kinase inhibitors such as imatinib in chronic myeloid leukemia (CML) or hypereosinophilic syndrome (HES)/CEL shed new interest on molecular diagnostics and detection of minimal residual disease (MRD) in CMPD.
Today, CMPD are primarily separated in CML as defined by the Philadelphia translocation t(9;22)(q34;q11)/BCR–ABL and in all other so-called BCR/ABL-negative CMPD. According to the WHO proposal of 2001 [8], the latter are subdivided into PV, CIMF, ET, and unclassified CMPD (CMPD-U). Some very rare disorders as chronic neutrophilic leukemia (CNL), HES, and CEL are additionally included. This broad spectrum becomes even more heterogeneous due to the continuous progress of stages, as all CMPD have the potential of clonal evolution and stepwise progression. They often terminate in bone marrow failure due to myelofibrosis or ineffective hematopoiesis or in acceleration and finally transformation to blast crisis. Differential diagnosis in CMPD is further hampered by the biologically given overlap of the diverse morphologic phenotypes and the sometimes close relationship to reactive conditions, and even show overlaps to myelodysplastic disorders. The WHO, thus, created a category of disorders combining myeloproliferative and myelodysplastic features in which chronic myelomonocytic leukemia (CMML), unclassified myelodysplastic/myeloproliferative disorder (MDS/MPD, U), and some very rare disorders as juvenile myelomonocytic leukemia (JMML) were incorporated [8, 9].
It is well known that PV has a median survival of 10 years, ET of 10–15 years, but CIMF of only 4 years. However, the clinical course in CMPD ranges from a few months with rapid leukemic transformation to several decades. These uncertainties in prognosis and the similarities in the clinical and morphological phenotypes at diagnosis plead for inclusion of other than clinical and morphologic parameters only into classification.
Although chromosomal abnormalities are not specific for distinct CMPD, they contribute to the definition of the prognosis and to the classification of the CMPD. However, aberrant karyotypes are detectable in only 5–45% of all BCR/ABL-negative CMPD, depending on the specific subtype.
Routinely applied methods further include by now polymerase chain reaction (PCR) screening for the V617F mutation in the JAK2 non-receptor tyrosine kinase [1–5] and will probably soon be included as diagnostic criteria in a revised WHO classification of the CMPD [10]. This novel marker is highly utile for the confirmation of a BCR/ABL-negative CMPD and might contribute to the definition of the prognosis and even for MRD strategies in the future [11]. Molecular methods in the CMPD further encompass PCR analyses of some rare gene fusions, e.g., in HES/CEL [6, 7] or in the 8p11 syndrome [12].
Adaptation of these extensive diagnostic procedures in CMPD to the laboratories’ resources becomes a major challenge. Major goals are standardization of diagnostic workflow, hierarchical order of methods, and combination of single results. This review intends to propose specific diagnostic algorithms for scenarios in BCR/ABL-negative CMPD.
Preanalytic conditions
To achieve optimal conditions in the diagnostic procedures, a standardized preparation of the samples and optimal conditions for transport are essential in the CMPD: Cytomorphology requires 3 ml bone marrow and 2 ml peripheral blood anticoagulated with ethylenediaminetetraacetic acid (EDTA), being aware that cytomorphology is hampered by heparine. Cytogenetics, in contrast, requires 5–10 ml heparinized bone marrow and 10–20 ml heparinized peripheral blood, as cultivation of metaphases is nearly inhibited by EDTA which induces apoptosis of cells. Multiparameter flow cytometry and all molecular genetic methods can be performed either on EDTA or heparinized material. Trephine biopsies should be performed for histomorphology and immunohistochemistry and allow cytomorphological evaluation by smears from the trephine cylinder in case of a dry tap. In the latter case, also for cytogenetics, a trephine cylinder can be transferred to isotone saline solution plus heparine, which, in many cases, makes metaphases after cultivation in cytogenetic medium possible.
Cytomorphology in CMPD
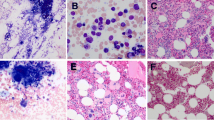
Differential diagnosis in the CMPD should always include investigation of peripheral blood smears, bone marrow aspirates, and trephine biopsies in parallel. Smears from peripheral blood and bone marrow are stained according to May Grunwald Giemsa. This may be completed by other stainings: Myeloperoxidase (MPO) reaction and non-specific-esterase (NSE) should be performed in blast crisis after CMPD and are warranted in cases of CMML. Iron staining may be performed additionally, but is of minor importance for the differential diagnostics, as in an early PV, iron will not always be absent. MPO and iron staining are further helpful in all cases with an overlap between the CMPD and MDS for detection of MPO deficiency and ringed sideroblasts. Cases with suspicious HES or CEL should, in addition, undergo toluidine blue staining for detection of mast cells which are frequently increased in CEL with the FIP1L1–PDGFRA gene fusion.
In PV, cytomorphology shows increased cellularity with trilineage cell proliferation. Stainable iron is completely missing in many cases. PV is further characterized by elevated blood counts in either cell line (Hb > 18.5 g/dl in men, >16.5 g/dl in women, platelets ≥400 × 109/l, WBC ≥12 × 109/l). In addition, other criteria as reduced serum erythropoietin levels below normal ranges [10, 13] or in vitro formation of endogenous erythroid colonies are included in the classification criteria [8]. In CIMF, bone marrow cytology is often hampered by myelofibrosis, and the peripheral blood shows the characteristical poikilocytosis and leukoerythroblastosis. However, these findings are not specific but occur as well in secondary myelofibrosis following other CMPD. ET is characterized by proliferation of the megakaryocytic lineage with clusters of enlarged mostly mature megakaryocytes in normocellular bone marrow. Granulopoiesis and erythropoiesis present as normal. According to the WHO [8], a diagnosis of ET requires a sustained peripheral platelet count ≥600 × 109/l, whereas reactive thrombocytosis must be excluded. Recently, an international expert panel recommended to lower the threshold for the diagnosis of ET to 450 × 109/l [10]. All CMPD, but especially CML, may show the so-called pseudo-Gaucher cells in the bone marrow, which represent glycolipide storing histiocytes resulting from increased cell proliferation [14]. Another specific cytomorphological subentity is represented by refractory anemia with ringed sideroblasts associated with marked thrombocytosis >500 × 109/l (RARS-T). This rare subtype may be included within the category of overlapping myelodysplastic and myeloproliferative diseases in the upcoming WHO classification [15–17].
Histomorphology in CMPD
Bone marrow histology has a central role in the diagnosis of CMPD. Staining is performed according to Giemsa, PAS, and chloroacetate esterase. Gomori silver impregnation allows assessment of reticulin fibers to quantify bone marrow connective tissue.
Thus, a diagnosis of CIMF requires at least a bone marrow histology, as bone marrow aspirates are hampered in most cases. Histology shows variable reticulin or collagen fibrosis, osteosclerosis, and sometimes even decreased cellularity. Sinuses are dilated with intraluminal hematopoiesis and erythrocyte extravasates. Megakaryopoiesis is increased with signs of dysplasia [8, 18].
PV demonstrates increased megakaryopoiesis, increased granulopoiesis, and erythropoiesis without storage iron, sinusoid hyperplasia, and variable myelofibrosis in combination with osteopenia. These characteristics allow discrimination from reactive erythrocytosis [19]. In more detail, differentiation from cases of secondary polycythemia includes the evaluation of megakaryopoiesis which shows clustering and pleomorphous appearance with very small and giant megakaryocytes with the characteristical staghorn-like nuclei neighboring each other [19, 20].
ET is characterized by clusters of enlarged mature megakaryocytes close to the sinusoids, whereas erythropoiesis and granulopoiesis are normal [10, 18]. A specific problem is provided by the differentiation between ET and prefibrotic CIMF, as both might be characterized by thrombocytosis in initial stages, and reticulin fibrosis might be minimal or absent in prefibrotic CIMF. However, prefibrotic CIMF is characterized by marked hypercellularity, left-shifted increased granulopoiesis, and a particular megakaryocyte morphology with nuclear features, whereas ET shows hyperlobulated and mature-appearing megakaryocytes [10, 21].
Cytogenetics in BCR/ABL-negative CMPD
The frequency of clonal karyotype anomalies varies considerably between the different BCR/ABL-negative CMPD entities. The presence of karyotype abnormalities at diagnosis per se seems to be prognostically negative [9]. CIMF has the highest karyotype aberration rate with 33–43% of all cases, followed by PV in 33–35%, whereas in ET, clonal abnormalities are extremely rare (<5%) [22–25]. In CMPD-U, aberrant karyotypes were reported in ∼20% [22], but definition of the true incidence is difficult due to the heterogeneity of subtypes in this category.
Chromosomal changes in the CMPD are not specific, but their presence at least confirms the diagnosis of a malignant hematopoietic disorder and contributes additional aspects to differential diagnosis. This can be exemplified in the 9p-aberrations which are closely associated to PV and to CIMF. In addition, translocations involving ABL, PDGFRA, PDGFRB or other tyrosine kinases can be detected by chromosome banding analyses, allowing the identification of patients who probably benefit from treatment with tyrosine kinase inhibitors.
Thus, chromosome banding analyses contribute a lot at diagnosis in many in cases with a suspicious or proven CMPD. However, they do not lead to important information for clinically clearly proven cases of ET. Cytogenetics may also be needed for the follow-up of the CMPD, as leukemic transformation is characterized in many cases by clonal evolution to more complex karyotypes resulting in higher rates of chromosomal abnormalities of ≥90% [9, 23, 26].
Interphase (IP-), metaphase (HMF-), and 24-color fluorescence in situ hybridization (FISH) may further confirm and clarify the results of the chromosome banding analyses. IP-FISH probes can be used for future MRD studies. Nearly all typically observed aberrations—e.g., +8, +9, gain of 9p, or del(20q)—can be monitored.
Trisomy 8 is the most frequent aberration in the CMPD being detected in ∼20% of all cytogenetic aberrant PV cases and in ∼10% in chromosomally aberrant CIMF—mostly as sole abnormality or in combination with +9. This is followed by trisomy 9 in ∼10% of all cytogenetically aberrant cases. Partial trisomies of 9p are equally frequent with a special association to PV [27–30]. Other recurrent aberrations are deletions of 13q and 20q and partial trisomies of 1q [9, 22, 31], whereas +19, +21, −7, −Y, del(12p), and i(17q) are less frequent.
Chromosomal changes show a characteristic distribution within the diverse CMPD. In detail, PV shows, as the most frequent changes, +9, followed by +8 and by del(20q) [23, 26]. CIMF has a more heterogeneous pattern with deletions of 13q and of 20q both in ∼9% of all cases [9, 25], structural abnormalities of 1q and 5q, and chromosome 7 abnormalities [23, 31]. In ET, chromosomal abnormalities are found in <5% of cases only, mostly represented by numerical gain of chromosome 9. Table 1 presents an overview on recurrent cytogenetic and molecular markers in the CMPD.
Balanced translocations as revealed by cytogenetics are rare in the CMPD. Many of these lead to the disruption of genes encoding tyrosine kinases. The breakpoints cluster in two regions at 5q31-33 and 8p11 which target the platelet-derived growth factor receptor beta [e.g., in the t(5;12)(q31q33;p12)/ETV6-PDGFRB)] and the fibroblast growth factor receptor 1 kinase [e.g., in t(8;13)(p11;q12)/FGFR1-ZNF198)]. Further, the ABL non-receptor tyrosine kinase might be involved in these rare rearrangements as in the t(9;12)(q34;p13)/ETV6-ABL [32]. The 8p11 myeloproliferative syndrome shows a specific profile outlined by frequent association to Non-Hodgkin’s lymphoma, high leukemic transformation rates, eosinophilia, and CML-like findings in bone marrow cytomorphology. It is most frequently caused by the t(8;13)(p11;q12)/FGFR1-ZNF198, but many other variants all involving 8p11/FGFR1 have been described. Bone marrow cytomorphology shows CML-like findings and eosinophilia [12]. As patients with PDFRB and ABL rearrangements are all candidates for tyrosine kinase inhibitor treatment, detection of these rare rearrangements by cytogenetics in combination with FISH and PCR is obligatory. For an overview on these reciprocal gene fusions, we refer to Cross and Reiter [32].
Molecular mutations in BCR/ABL-negative CMPD
As published in 2005 by several study groups, a high proportion of patients with BCR/ABL-negative CMPD have a somatic point mutation in the JAK2 gene on 9p24 (V617F) which codes for the JAK2 kinase. In detail, the mutation was found in 80–97% of all patients with PV, in >50% of all patients with CIMF, and in 40–57% in ET [1–5]. Janus kinases are non-receptor TKs which regulate the phosphorylation of several signaling pathways, e.g., JAK/STAT, whose activity is increased by the JAK2 mutation [3, 5]. Interestingly, JAK2V617F-positive ET cases were found to show considerable clinical similarities to PV. This pleads for common pathogenetic pathways in part of the ET cases and in PV [33]. It has to be expected that the JAK2V617F mutation will soon be included as a major criterion for PV diagnosis in a revised WHO classification, as nearly all cases were found to be positive [10]. According to this proposal, also in ET or in CIMF, the respective mutation will serve likewise to any other clonal marker as criterion for the diagnosis of ET or CIMF, which further emphasizes its value for diagnostics in the CMPD.
A positive mutation status seemed correlated with further advanced stages. Homozygous JAK2 mutations are more frequent in PV and CIMF than in ET [26] and are associated with a longer history of disease than heterozygous mutations [34]. Thus, a homozygous mutation status correlates with a more aggressive course and might indicate an inferior outcome.
Different assays were developed for JAK2 mutational analyses, e.g., allele specific PCR, real-time PCR, or pyrosequencing, which is able to convey information on the frequency of mutated alleles [35]. Kroger et al. [11] showed that quantitative assessment of the JAK2 mutation with real-time PCR after allogeneic hematopoietic stem cell transplantation was valid as minimal residual disease parameter allowing the adaptation of adoptive immunotherapy accordingly. Thus, determination of the JAK2V617F mutation status is highly valuable for all cases with a suspicious or proven BCR/ABL-negative CMPD and even contributes to determination of the prognosis and to MRD strategies.
The role of the JAK2V617F mutation is not limited to the “classical” CMPD but was detected in other myeloid malignancies as well, e.g., in 3–10% of all MDS cases [1, 36, 37] or in 50–90% in RARS-T representing an ambiguous subentity with overlapping myeloproliferative and myelodysplastic features [17, 38]. Interestingly, the JAK2V617F mutation was as well found in 20–30% of patients with abdominal vein thromboses and in 5% of patients with cerebral vein thromboses without signs of an overt hematologic disorder [39, 40].
Since the detection of the JAK2617F, the panel of known activating mutations in the CMPD is continuously increasing: PV patients who were JAK2V617F-negative were detected to carry somatic gain-of-function mutations within exon 12 of the JAK2 gene in 40% of cases in a recent study. This mutation subtype was shown to stimulate erythroid proliferation in in vitro experiments [40, 41]. Further on, ∼5% of CIMF and ∼1% of all ET cases show somatic mutations in codon 515 within the transmembrane domain of the MPL gene which encodes the thrombopoietin receptor. The respective point mutations lead to single amino exchanges (W515L and W515K) and induce constitutive cytokine-independent activation of the JAK-STAT pathway as gain-of-function-mutations likewise to the V617F [42–44].
Chronic neutrophilic leukemia
CNL is a very rare CMPD defined by persistent leukocytosis in pB ≥25 × 109/l, segmented neutrophils and bands >80% of WBC, immature WBC <10%, and myeloblasts <1% [8]. Survival is extremely heterogeneous and was reported from a few months to 20 years. Cytogenetic aberrations are rare and include +8, +9, del(20q), and del(11q) [8, 45, 46]. The JAK2 mutation was described in few cases of CNL [4, 22, 37, 45–48], but determination of the true incidence is extremely difficult due to the rare occurrence. Some CNL cases were identified to bear rare BCR–ABL fusion transcripts with a breakpoint between exons c3 and c4 of the BCR gene leading to a 230-kDa fusion protein [49, 50].
Hypereosinophilic syndrome/chronic eosinophilic leukemia
Persisting hypereosinophilia is, in most cases, reactive and is only rarely caused by a malignant disorder such as HES or CEL or other eosinophilia-associated CMPD [6, 7, 51–53]. HES is defined by persistent eosinophilia ≥1.5 × 109/l in peripheral blood >6 months and an increased number of bone marrow eosinophils of unknown origin; this is accompanied by organ involvement and dysfunction. Classification as HES requires exclusion of all other causes and failure of detection of the underlying genetic defect by cytogenetic and/or molecular screening.
A diagnosis of CEL requires >2% blasts in peripheral blood and >5–19% bone marrow blasts or evidence of clonality [8, 54]. The most frequent aberration in CEL is the FIP1L1–PDGFRA fusion which results from a cryptic interstitial deletion on chromosome 4q12. Whereas chromosome banding analyses fail to detect the respective cytogenetic correlate, it is revealed by IP-FISH with differently marked probes for CHIC2, FIP1L1, and PDGFRA, and with reverse transcription (RT)-PCR for FIP1L1–PDGFRA [55, 56].
Some more rare TK gene fusions were detected in eosinophilia-associated CMPD, which involve the tyrosine receptor kinases PDGFRA on 4q12, PDGFRB on 5q31, FGFR1 on 8p11, and the non-receptor kinase JAK2 on 9p24 [9, 57]. The beneficial response of patients with PDGFRA and PDGFRB rearrangements to imatinib makes the detection of these rearrangements obligatory [6, 7, 53, 58]. Therefore, a combination of cytomorphology, cytogenetics, IP-FISH, and RT-PCR based on the patient’s history provides the basis for optimized diagnosis in eosinophilia-associated CMPD followed by targeted therapy [32, 59, 60].
Chronic myelomonocytic leukemia
Due to its ambiguous character, CMML was incorporated by the WHO into a category which overlaps between myelodysplastic and myeloproliferative disorders [8] and was defined by peripheral monocytes >1 × 109/l and by dysgranulopoiesis >10%. Blasts and promonocytes were defined by <20% of WBC and by <20% of all nucleated cells in bone marrow. NSE was strongly recommended for bone marrow examination. Clonal karyotype abnormalities occur in 25–35% of all cases. Most frequent are changes of chromosome 7, trisomy 8, and complex aberrant karyotype which is defined by three or more chromosomal aberrations [9, 22, 61]. Mutations of the NRAS protooncogene are the most frequent so far identified molecular markers with variable incidences of 10–66% in this entity. Although there was a wide range in these studies (probably due to the limited samples size in the different studies), this high incidences suggest parallels to MDS or AML [61–63]. The JAK2 mutation was detected in 3–13% of all cases with CMML [1, 4, 37], which illustrates the vicinity to the CMPD in another part of CMML cases. This molecular heterogeneity correlates with the clinical and morphological diversity of CMML and supports the ambiguous position as suggested in the WHO classification.
Remission criteria in the CMPD
New therapeutic strategies including allogeneic stem cell transplantation as potentially curative option or targeted therapies in the CMPD implicate the need for more differentiated and sensitive criteria of remission. For CIMF, an international working group formulated new consensus criteria for response to treatment [64]. These criteria are based on a combination of clinical and laboratory parameters and include cyto- and histomorphological, cytogenetic, and molecular findings. Thus, highest so far applicable sensitivity is achieved. Clinical criteria include disappearance of clinical symptoms as palpable hepatosplenomegaly. The laboratory and cytomorphological criteria of complete remission imply normalization of trilineage peripheral blood count and the absence of blasts, immature progenitor cells, or nucleated erythroid precursors in peripheral blood. Bone marrow histologic remission criteria apply to cellularity, myeloblast percentage, and osteomyelofibrosis. Finally, cytogenetic response criteria discriminate major cytogenetic response, meaning absence of chromosomal abnormalities in cases with a preexisting aberration from minor cytogenetic response requiring a ≥50% reduction of abnormal metaphases. As the most sensitive criterion, major molecular response defines absence of a specific disease-associated mutation in previously positive cases [64].
Approach to a diagnostic algorithm in the CMPD
A diagnostic algorithm for all cases with diagnosis or suspicion of CMPD (Fig. 1) should start with the cytomorphologic evaluation of peripheral blood and bone marrow. This allows, in many, cases a differentiation between CML and a BCR/ABL-negative CMPD. In parallel, all cases should be evaluated by histomorphology.
Proposal for a diagnostic algorithm in BCR/ABL-negative CMPD. HES Idiopathic hypereosinophilic syndrome, CEL chronic eosinophilic leukemia, PV polycythemia vera, CIMF chronic idiopathic myelofibrosis, CMPD-U unclassifiable CMPD, ET essential thrombocytosis, RARS-T refractory anemia with ringed sideroblasts, CMML chronic myelomonocytic leukemia, MFC multiparameter flow cytometry, RT-PCR reverse transcription polymerase chain reaction. Dashed line may add information in difficult cases, but not obligatory
Chromosome banding analyses might gain important information in PV, CIMF, and also in CMPD-U, as chromosomal aberration rates of ∼20–45% were reported [22]. According to the recent guidelines of a British Committee, cytogenetics are considered as “stage 2 investigations” in case of PV and erythrocytosis which should be performed in dependence on the results of clinical evaluation, blood count, and the JAK2 mutation as well as other laboratory parameters such as serum ferritin which are obligatory as “stage 1 investigations” [65]. In contrast, cytogenetics can be neglected in clinically clear cases of ET due to the extremely low incidence of aberrant karyotypes. In cases in which the discrimination of a CMPD from a reactive disorder is not possible according to clinical, laboratory, and cyto-/histomorphological aspects, cytogenetics might contribute to differential diagnosis, as, in some cases, clonal abnormalities confirm the diagnosis of a hematologic malignancy. CMML should as well undergo cytogenetic analyses; in addition, molecular screening for NRAS mutations might be discussed due to their frequent occurrence and new drugs that may come up. This also includes the investigation of PDGF receptors expression.
The chromosomal aberrations as revealed by chromosome banding analyses—e.g., +8, +9, del(20q)—can be verified by FISH techniques. This further allows the selection of IP probes for distinct numerical and structural aberrations to provide parameters for MRD diagnostics.
Today, the backbone in all cases of suspicious or proven CMPD should be screening for the JAK2V617F mutation status by PCR, e.g., by a melting curve light cycler assay [66]. According to the proposals for a revised WHO classification, evidence of the JAK2V617F mutation (localized in exon 14 of the JAK2 gene) or a functionally similar mutation will be required as major criterion for the diagnosis of PV. This might justify additional screening for JAK2 mutations in exon 12 in cases which are highly suspicious for PV from morphological aspects but are negative for the JAK2V617F [10].
Finally, all cases with a suspected or proven CMPD should be evaluated by IP-FISH or PCR for BCR–ABL to exclude a diagnosis of CML due to the therapeutic consequences. This is even more emphasized by single cases showing a coincidence of the BCR–ABL fusion and the JAK2V617F mutation where the cytomorphological features of the CMPD can mask the CML aspect [67].
In cases with diagnosis or suspicion of HES/CEL, cytogenetic analysis is informative only in very few cases and may be omitted, whereas molecular diagnostics in search of the FIP1L1–PDGFRA gene fusion by IP-FISH and/or RT-PCR is obligatory.
Conclusions
For many years, diagnostics in the BCR/ABL-negative CMPD were mainly based on clinical symptoms, cytomorphology, and histomorphological findings. This has dramatically changed in recent years. The WHO (2001) [8] included cytogenetic aspects directly and indirectly in their classification system. This can be exemplified in ET which is excluded by evidence of a del(5q) or an inv(3)(q21q26), as both the 5q- syndrome in MDS or AML with the respective inversion 3 can show microkaryocytes and high thrombocytes. Clonal chromosomal abnormalities other than the Philadelphia translocation support the diagnosis of CMPD and allow to discriminate this from reactive conditions.
Additionally, the spectrum of molecular mutations considerably increased. Most molecular events target receptor TK (such as FGFR1, PDGFRA, and PDGFRA) and non-receptor-TK (such as ABL or JAK2). Especially, the detection of the JAK2 mutation in the majority of patients with a CMPD has revolutionized diagnostics in the CMPD [13] and allows, in many cases, now a rapid and clear discrimination of the CMPD from reactive conditions. It further may abolish the measurement of the PRV1 expression in cases with suspected PV. JAK2 mutated cases seem to be associated with higher complication rates and an increased need for therapeutic interventions when compared to wild-type patients [3]. This might play a role for the choice of therapy in the future. Finally, JAK2 might represent a target for specific compounds with anti-tyrosine kinase activity [2, 34]. The recent description of JAK2 mutations in exon 12 in V617F-negative PV cases [40, 41] and of the W515 mutations of the MPL gene in a low frequency in ET and CIMF [42–44] illustrate that we have to assume a complex network of activating mutations in the CMPD of which only parts are so far identified. Thus, a new classification of the CMPD according to the molecular substrate, e.g., the JAK2 mutation, likewise to the definition of CML, will be more appropriate [10, 68]. The inclusion of JAK2 mutation analysis as a major criterion for the PV diagnosis within the current and upcoming World Health Organization (WHO) diagnostic criteria was suggested [10].
The detection of the FIP1L1–PDGFRA fusion in CEL/HES in association to the good response to imatinib [6, 52] and the increasing detection of rare fusion transcript in the BCR/ABL-negative CMPD [32] contributed as well significantly to an improved molecular classification in CMPD.
MRD strategies are so far poorly established in the Philadelphia negative CMPD when compared to the acute leukemias or to CML. This might change in the near future, as it was already shown in a post-transplantation setting that quantitative assessment of the JAK2 mutation qualifies as MRD marker [11]. In CML, the definition of remission criteria allowed an international standardization in clinical studies and was helpful for clinical routine. This approach is increasingly important also for the BCR/ABL-negative CMPD as realized by an international working group proposing cytogenetic and molecular response criteria in CIMF [64].
In conclusion, diagnostics in the BCR/ABL-negative CMPD have abandoned the former perception which classified these complex disorders mainly on clinical and morphological aspects and are on the way to a comprehensive approach focussing increasingly on cyto- and molecular genetic aspects. Individual treatment is already available or will hopefully follow.
References
Jelinek J, Oki Y, Gharibyan V, Bueso-Ramos C, Prchal JT, Verstovsek S, Beran M, Estey E, Kantarjian HM, Issa JP (2005) JAK2 mutation 1849G>T is rare in acute leukemias but can be found in CMML, Philadelphia chromosome-negative CML, and megakaryocytic leukemia. Blood 106:3370–3373
Jones AV, Kreil S, Zoi K, Waghorn K, Curtis C, Zhang L, Score J, Seear R, Chase AJ, Grand FH, White H, Zoi C et al (2005) Widespread occurrence of the JAK2 V617F mutation in chronic myeloproliferative disorders. Blood 106:2162–2168
Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR, Tichelli A, Cazzola M, Skoda RC (2005) A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 352:1779–1790
Levine RL, Wadleigh M, Cools J, Ebert BL, Wernig G, Huntly BJ, Boggon TJ, Wlodarska I, Clark JJ, Moore S, Adelsperger J, Koo S et al (2005) Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell 7:387–397
Tefferi A, Lasho TL, Gilliland G (2005) JAK2 mutations in myeloproliferative disorders. N Engl J Med 353:1416–1417
Cools J, DeAngelo DJ, Gotlib J, Stover EH, Legare RD, Cortes J, Kutok J, Clark J, Galinsky I, Griffin JD, Cross NC, Tefferi A et al (2003) A tyrosine kinase created by fusion of the PDGFRA and FIP1L1 genes as a therapeutic target of imatinib in idiopathic hypereosinophilic syndrome. N Engl J Med 348:1201–1214
Gotlib J, Cools J, Malone JM3, Schrier SL, Gilliland DG, Coutre SE (2004) The FIP1L1-PDGFRalpha fusion tyrosine kinase in hypereosinophilic syndrome and chronic eosinophilic leukemia: implications for diagnosis, classification, and management. Blood 103:2879–2891
Jaffe ES, Harris NL, Stein H, Vardiman JWE (2001) World Health Organization classification of tumours: pathology and genetics of tumours of haematopoietic and lymphoid tissues. IARC, Lyon
Bench AJ, Cross NC, Huntly BJ, Nacheva EP, Green AR (2001) Myeloproliferative disorders. Best Pract Res Clin Haematol 14:531–551
Tefferi A, Thiele J, Orazi A, Kvasnicka HM, Barbui T, Hanson CA, Barosi G, Verstovsek S, Birgegard G, Mesa R, Reilly JT, Gisslinger H et al (2007) Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood 110:1092–1097
Kroger N, Badbaran A, Holler E, Hahn J, Kobbe G, Bornhauser M, Reiter A, Zabelina T, Zander AR, Fehse B (2007) Monitoring of the JAK2-V617F mutation by highly sensitive quantitative real-time PCR after allogeneic stem cell transplantation in patients with myelofibrosis. Blood 109:1316–1321
Reiter A, Hehlmann R, Goldman JM, Cross NC (1999) The 8p11 myeloproliferative syndrome. Med Klin (Munich) 94:207–210
McMullin MF, Bareford D, Campbell P, Green AR, Harrison C, Hunt B, Oscier D, Polkey MI, Reilly JT, Rosenthal E, Ryan K, Pearson TC et al (2005) Guidelines for the diagnosis, investigation and management of polycythaemia/erythrocytosis. Br J Haematol 130(2):174–195
Löffler H, Rastetter J, Haferlach TE (2005) Atlas of clinical hematology, 2nd edition. Springer, Berlin Heidelberg New York
Shaw GR (2005) Ringed sideroblasts with thrombocytosis: an uncommon mixed myelodysplastic/myeloproliferative disease of older adults. Br J Haematol 131:180–184
Szpurka H, Tiu R, Murugesan G, Aboudola S, Hsi ED, Theil KS, Sekeres MA, Maciejewski JP (2006) Refractory anemia with ringed sideroblasts associated with marked thrombocytosis (RARS-T), another myeloproliferative condition characterized by JAK2 V617F mutation. Blood 108:2173–2181
Gattermann N, Billiet J, Kronenwett R, Zipperer E, Germing U, Nollet F, Criel A, Selleslag D (2007) High frequency of the JAK2 V617F mutation in patients with thrombocytosis (platelet count > 600 × 109/l) and ringed sideroblasts more than 15% considered as MDS/MPD, unclassifiable. Blood 109:1334–1335
Tefferi A, Solberg LA, Silverstein MN (2000) A clinical update in polycythemia vera and essential thrombocythemia. Am J Med 109:141–149
Thiele J, Kvasnicka HM (2000) Polyglobuly versus polycythemia vera. Pathologe 21:24–30
Thiele J, Kvasnicka HM, Zankovich R, Diehl V (2001) The value of bone marrow histology in differentiating between early stage Polycythemia vera and secondary (reactive) Polycythemias. Haematologica 86:368–374
Thiele J, Kvasnicka HM, Orazi A (2005) Bone marrow histopathology in myeloproliferative disorders—current diagnostic approach. Semin Hematol 42:184–195
Bacher U, Haferlach T, Kern W, Hiddemann W, Schnittger S, Schoch C (2005) Conventional cytogenetics of myeloproliferative diseases other than CML contribute valid information. Ann Hematol 84:250–257
Bench AJ, Nacheva EP, Champion KM, Green AR (1998) Molecular genetics and cytogenetics of myeloproliferative disorders. Baillieres Clin Haematol 11:819–848
Sessarego M, Defferrari R, Dejana AM, Rebuttato AM, Fugazza G, Salvidio E, Ajmar F (1989) Cytogenetic analysis in essential thrombocythemia at diagnosis and at transformation. A 12-year study. Cancer Genet Cytogenet 43:57–65
Tefferi A, Mesa RA, Schroeder G, Hanson CA, Li CY, Dewald GW (2001) Cytogenetic findings and their clinical relevance in myelofibrosis with myeloid metaplasia. Br J Haematol 113:763–771
Schnittger S, Bacher U, Kern W, Haferlach T, Haferlach C (2007) JAK2V617F as progression marker in CMPD and as cooperative mutation in AML with trisomy 8 and t(8;21): a comparative study on 1103 CMPD and 269 AML cases. Leukemia 21:1843–1845
Andrieux J, Demory JL, Caulier MT, Agape P, Wetterwald M, Bauters F, Lai JL (2003) Karyotypic abnormalities in myelofibrosis following polycythemia vera. Cancer Genet Cytogenet 140:118–123
Bacher U, Haferlach T, Schoch C (2005) Gain of 9p due to an unbalanced rearrangement der(9;18): a recurrent clonal abnormality in chronic myeloproliferative disorders. Cancer Genet Cytogenet 160:179–183
Chen Z, Notohamiprodjo M, Guan XY, Paietta E, Blackwell S, Stout K, Turner A, Richkind K, Trent JM, Lamb A, Sandberg AA (1998) Gain of 9p in the pathogenesis of polycythemia vera. Genes Chromosomes Cancer 22:321–324
Najfeld V, Montella L, Scalise A, Fruchtman S (2002) Exploring polycythaemia vera with fluorescence in situ hybridization: additional cryptic 9p is the most frequent abnormality detected. Br J Haematol 119:558–566
Mertens F, Johansson B, Heim S, Kristoffersson U, Mitelman F (1991) Karyotypic patterns in chronic myeloproliferative disorders: report on 74 cases and review of the literature. Leukemia 5:214–220
Cross NC, Reiter A (2002) Tyrosine kinase fusion genes in chronic myeloproliferative diseases. Leukemia 16:1207–1212
Campbell PJ, Green AR (2006) The myeloproliferative disorders. N Engl J Med 355:2452–2466
Baxter EJ, Scott LM, Campbell PJ, East C, Fourouclas N, Swanton S, Vassiliou GS, Bench AJ, Boyd EM, Curtin N, Scott MA, Erber WN et al (2005) Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet 365:1054–1061
Steensma DP (2006) JAK2 V617F in myeloid disorders: molecular diagnostic techniques and their clinical utility: a paper from the 2005 William Beaumont Hospital Symposium on Molecular Pathology. J Mol Diagn 8:397–411
Levine RL, Loriaux M, Huntly BJ, Loh ML, Beran M, Stoffregen E, Berger R, Clark JJ, Willis SG, Nguyen KT, Flores NJ, Estey E et al (2005) The JAK2V617F activating mutation occurs in chronic myelomonocytic leukemia and acute myeloid leukemia, but not in acute lymphoblastic leukemia or chronic lymphocytic leukemia. Blood 106:3377–3379
Steensma DP, Dewald GW, Lasho TL, Powell HL, McClure RF, Levine RL, Gilliland DG, Tefferi A (2005) The JAK2 V617F activating tyrosine kinase mutation is an infrequent event in both “atypical” myeloproliferative disorders and myelodysplastic syndromes. Blood 106:1207–1209
Boissinot M, Garand R, Hamidou M, Hermouet S (2006) The JAK2-V617F mutation and essential thrombocythemia features in a subset of patients with refractory anemia with ring sideroblasts (RARS). Blood 108:1781–1782
Boissinot M, Lippert E, Girodon F, Dobo I, Fouassier M, Masliah C, Praloran V, Hermouet S (2006) Latent myeloproliferative disorder revealed by the JAK2-V617F mutation and endogenous megakaryocytic colonies in patients with splanchnic vein thrombosis. Blood 108:3223–3224
De S, V, Fiorini A, Rossi E, Za T, Farina G, Chiusolo P, Sica S, Leone G (2007) Incidence of the JAK2 V617F mutation among patients with splanchnic or cerebral venous thrombosis and without overt chronic myeloproliferative disorders. J Thromb Haemost 5:708–714
Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR, Futreal PA, Erber WN, McMullin MF, Harrison CN, Warren AJ, Gilliland DG et al (2007) JAK2 exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med 356:459–468
Levine RL, Wernig G (2006) Role of JAK-STAT signaling in the pathogenesis of myeloproliferative disorders. Hematology Am Soc Hematol Educ Program 510:233–239
Pardanani AD, Levine RL, Lasho T, Pikman Y, Mesa RA, Wadleigh M, Steensma DP, Elliott MA, Wolanskyj AP, Hogan WJ, McClure RF, Litzow MR et al (2006) MPL515 mutations in myeloproliferative and other myeloid disorders: a study of 1182 patients. Blood 108:3472–3476
Pikman Y, Lee BH, Mercher T, McDowell E, Ebert BL, Gozo M, Cuker A, Wernig G, Moore S, Galinsky I, DeAngelo DJ, Clark JJ et al (2006) MPLW515L is a novel somatic activating mutation in myelofibrosis with myeloid metaplasia. PLoS 3:e270
Bohm J, Schaefer HE (2002) Chronic neutrophilic leukaemia: 14 new cases of an uncommon myeloproliferative disease. J Clin Pathol 55:862–864
Bohm J, Kock S, Schaefer HE, Fisch P (2003) Evidence of clonality in chronic neutrophilic leukaemia. J Clin Pathol 56:292–295
Kako S, Kanda Y, Sato T, Goyama S, Noda N, Shoda E, Oshima K, Inoue M, Izutsu K, Watanabe T, Motokura T, Chiba S et al (2007) Early relapse of JAK2 V617F-positive chronic neutrophilic leukemia with central nervous system infiltration after unrelated bone marrow transplantation. Am J Hematol 82:386–390
Mc Lornan DP, Percy MJ, Jones AV, Cross NC, Mc Mullin MF (2005) Chronic neutrophilic leukemia with an associated V617F JAK2 tyrosine kinase mutation. Haematologica 90:1696–1697
Pane F, Frigeri F, Sindona M, Luciano L, Ferrara F, Cimino R, Meloni G, Saglio G, Salvatore F, Rotoli B (1996) Neutrophilic-chronic myeloid leukemia: a distinct disease with a specific molecular marker (BCR/ABL with C3/A2 junction). Blood 88:2410–2414
Christopoulos C, Kottoris K, Mikraki V, Anevlavis E (1996) Presence of the bcr/abl rearrangement in a patient with chronic neutrophilic leukaemia. J Clin Pathol 49:1013–1015
Brito-Babapulle F (2003) The eosinophilias, including the idiopathic hypereosinophilic syndrome. Br J Haematol 121:203–223
Cools J, Stover EH, Wlodarska I, Marynen P, Gilliland DG (2004) The FIP1L1-PDGFRalpha kinase in hypereosinophilic syndrome and chronic eosinophilic leukemia. Curr Opin Hematol 11:51–57
Pardanani A, Brockman SR, Paternoster SF, Flynn HC, Ketterling RP, Lasho TL, Ho CL, Li CY, Dewald GW, Tefferi A (2004) FIP1L1-PDGFRA fusion: prevalence and clinicopathologic correlates in 89 consecutive patients with moderate to severe eosinophilia. Blood 104:3038–3045
Fletcher S, Bain B (2007) Eosinophilic leukaemia. Br Med Bull 81–82:115–127
La Starza R, Specchia G, Cuneo A, Beacci D, Nozzoli C, Luciano L, Aventin A, Sambani C, Testoni N, Foppoli M, Invernizzi R, Marynen P et al (2005) The hypereosinophilic syndrome: fluorescence in situ hybridization detects the del(4)(q12)-FIP1L1/PDGFRA but not genomic rearrangements of other tyrosine kinases. Haematologica 90:596–601
Roche-Lestienne C, Lepers S, Soenen-Cornu V, Kahn JE, Lai JL, Hachulla E, Drupt F, Demarty AL, Roumier AS, Gardembas M, Dib M, Philippe N et al (2005) Molecular characterization of the idiopathic hypereosinophilic syndrome (HES) in 35 French patients with normal conventional cytogenetics. Leukemia 19:792–798
Vandenberghe P, Wlodarska I, Michaux L, Zachee P, Boogaerts M, Vanstraelen D, Herregods MC, Van Hoof A, Selleslag D, Roufosse F, Maerevoet M, Verhoef G et al (2004) Clinical and molecular features of FIP1L1-PDFGRA (+) chronic eosinophilic leukemias. Leukemia 18:734–742
Apperley JF, Gardembas M, Melo JV, Russell-Jones R, Bain BJ, Baxter EJ, Chase A, Chessells JM, Colombat M, Dearden CE, Dimitrijevic S, Mahon FX et al (2002) Response to imatinib mesylate in patients with chronic myeloproliferative diseases with rearrangements of the platelet-derived growth factor receptor beta. N Engl J Med 347:481–487
Cools J (2005) FIP1L1-PDGFR alpha, a therapeutic target for the treatment of chronic eosinophilic leukemia. Verh K Acad Geneeskd Belg 67:169–176
Jovanovic JV, Score J, Waghorn K, Cilloni D, Gottardi E, Metzgeroth G, Erben P, Popp H, Walz C, Hochhaus A, Roche-Lestienne C, Preudhomme C et al (2007) Low-dose imatinib mesylate leads to rapid induction of major molecular responses and achievement of complete molecular remission in FIP1L1-PDGFRA-positive chronic eosinophilic leukemia. Blood 109:4635–4640
Onida F, Kantarjian HM, Smith TL, Ball G, Keating MJ, Estey EH, Glassman AB, Albitar M, Kwari MI, Beran M (2002) Prognostic factors and scoring systems in chronic myelomonocytic leukemia: a retrospective analysis of 213 patients. Blood 99:840–849
Padua RA, Guinn BA, Al-Sabah AI, Smith M, Taylor C, Pettersson T, Ridge S, Carter G, White D, Oscier D, Chevret S, West R (1998) RAS, FMS and p53 mutations and poor clinical outcome in myelodysplasias: a 10-year follow-up. Leukemia 12:887–892
Bacher U, Haferlach T, Kern W, Haferlach C, Schnittger S (2007) A comparative study of molecular mutations in 381 patients with myelodysplastic syndrome and in 4130 patients with acute myeloid leukemia. Haematologica 92:744–752
Tefferi A, Barosi G, Mesa RA, Cervantes F, Deeg HJ, Reilly JT, Verstovsek S, Dupriez B, Silver RT, Odenike O, Cortes J, Wadleigh M et al (2006) International Working Group (IWG) consensus criteria for treatment response in myelofibrosis with myeloid metaplasia, for the IWG for myelofibrosis research and treatment (IWG-MRT). Blood 108:1497–1503
McMullin MF, Reilly JT, Campbell P, Bareford D, Green AR, Harrison CN, Conneally E, Ryan K (2007) Amendment to the guideline for diagnosis and investigation of polycythaemia/erythrocytosis. Br J Haematol 138:821–822
Schnittger S, Bacher U, Kern W, Schroder M, Haferlach T, Schoch C (2006) Report on two novel nucleotide exchanges in the JAK2 pseudokinase domain: D620E and E627E. Leukemia 20:2195–2197
Hussein K, Bock O, Seegers A, Flasshove M, Henneke F, Buesche G, Kreipe HH (2007) Myelofibrosis evolving during imatinib treatment of a chronic myeloproliferative disease with coexisting BCR-ABL translocation and JAK2V617F mutation. Blood 109:4106–4107
Lelievre H, Ferrand A, Mozziconacci MJ, Birnbaum D, Delaval B (2006) Myeloproliferative disorders: premalignant, stem cell, G1 diseases? Leukemia 20:1475–1480
Michiels JJ, Thiele J (2002) Clinical and pathological criteria for the diagnosis of essential thrombocythemia, polycythemia vera, and idiopathic myelofibrosis (agnogenic myeloid metaplasia). Int J Hematol 76:133–145
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License ( https://creativecommons.org/licenses/by-nc/2.0 ), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Haferlach, T., Bacher, U., Kern, W. et al. The diagnosis of BCR/ABL-negative chronic myeloproliferative diseases (CMPD): a comprehensive approach based on morphology, cytogenetics, and molecular markers. Ann Hematol 87, 1–10 (2008). https://doi.org/10.1007/s00277-007-0403-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-007-0403-6