Abstract
Purpose
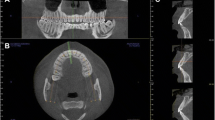
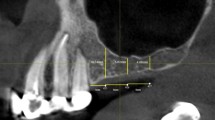
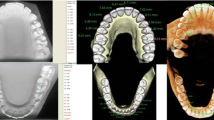
The purpose of this study was to evaluate the prevalence of mandibular lingual concavities and to measure them using CBCT (Cone-Beam Computerized Tomography).
Methods
In this study, CBCT scans of 200 patients requiring dental implants were assessed for lingual concavities. Reconstructed CBCT images were transferred as DICOM files to the 3D DOCTOR software program, and metric, volumetric, and surface area measurements were obtained. Two-way mixed ANOVA was used to model side (left/right, anterior), measurement type, and gender with side and type taken as within-subject variables, gender as between-subject variables, and age as a covariate. A comparison between the dentate and edentulous groups in the samples with lingual concavities was performed using an unpaired Student’s t test.
Results
Submandibular concavity mean depth and volume were found to be 2.4 mm and 130.7 mm3, whereas mean depth and volume of sublingual concavities were found to be 1.3 mm and 26.5 mm3. Significant inverse ratios were found between age and volume and between age and surface area (p < 0.05). All measurements were higher in males than females, but the differences were not statistically significant. The differences between the presence of concavity (sublingual, right, and left submandibular) and dental status (dentate/edentulous) were statistically insignificant (p > 0.05).
Conclusion
Mandibular lingual concavity dimensions were found to vary by age, location, and the presence/absence of teeth. Third party software can be used to generate 3-dimensional models that provide useful information about shape, size, and location of sublingual and submandibular concavities prior to implant placement.


Similar content being viewed by others
References
Alghamdi AST (2013) Pain sensation and post surgical complications in posterior mandibular implant placement using ridge mapping, panoramic radiography, and infiltration anesthesia. ISRN Dent. doi:10.1155/2013/134210
Chan HL, Benavides E, Yeh CY, Fu JH, Rudek IE, Wang HL (2011) Risk assessment of lingual plate perforation in posterior mandibular region: a virtual implant placement study using cone-beam computed tomography. J Periodontol 82:129–135
Chan HL, Brooks SL, Fu JH, Yeh CY, Rudek I, Wang HL (2011) Cross-sectional analysis of the mandibular lingual concavity using cone beam computed tomography. Clin Oral Impl Res 22:201–206
Chau ACM, Fung K (2009) Comparison of radiation dose for implant imaging using conventional spiral tomography, computed tomography, and cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:559–565
Dubois L, de Lange J, Baas E, Van Ingen J (2010) Excessive bleeding in the floor of the mouth after endosseus implant placement: a report of two cases. Int J Oral Maxillofac Surg 39:412–415
Horiuchi M, Ichikawa T, Kanitani H, Wigianto R, Kawamoto N, Matsumoto N (1995) Pilot-hole preparation for proper implant positioning and the enhancement of bone formation. J Oral Implantol 21:318–324
Kalpidis CD, Setayesh RM (2004) Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol 75:631–645
Kamburoğlu K, Murat S, Kılıç C, Yüksel S, Avsever H, Farman A, Scarfe WC (2014) Accuracy of CBCT images in the assessment of buccal marginal alveolar peri-implant defects: effect of field of view. Dentomaxillofac Radiol. doi:10.1259/dmfr.20130332
Lamas Pelayo J, Peñarrocha Diago M, Martí Bowen E, Peñarrocha Diago M (2008) Intraoperative complications during oral implantology. Med Oral Patol Oral Cir Bucal 13:239–243
Leong DJ, Chan HL, Yeh CY, Takarakis N, Fu JH, Wang HL (2011) Risk of lingual plate perforation during implant placement in the posterior mandible: a human cadaver study. Implant Dent 20:360–363
Lin MH, Mau LP, Cochran DL, Shieh YS, Huang PH, Huang RY (2014) Risk assessment of inferior alveolar nerve injury for immediate implant placement in the posterior mandible: a virtual implant placement study. J Dent. doi:10.1016/j.jdent.2013.12.014
Palma-Carrio C, Balaguer-Martinez J, Penarrocha-Oltra D, Penarrocha-Diago M (2011) Irritative and sensory disturbances in oral implantology: literature review. Med Oral Patol Oral Cir Bucal 16:1043–1046
Parnia F, Fard EM, Mahboub F, Hafezeqoran A, Gavgani FE (2010) Tomographic volume evaluation of submandibular fossa in patients requiring dental implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:32–36
Philipsen HP, Takata T, Reichart PA, Sato S, Suei Y (2002) Lingual and buccal mandibular bone depressions: a review based on 583 cases from a world-wide literature survey, including 69 new cases from Japan. Dentomaxillofac Radiol 31:281–290
Quirynen M, Mraiwa N, van Steenberghe D, Jacobs R (2003) Morphology and dimensions of the mandibular jaw bone in the interforaminal region in patients requiring implants in the distal areas. Clin Oral Impl Res 14:280–285
Scaravilli MS, Mariniello M, Sammartino G (2010) Mandibular lingual vascular canals (MLVC): evaluation on dental CTs of a case series. Eur J Radiol 76:173–176
Scarfe WC, Farman AG (2006) Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc 72:75–80
Shiratori LN, Marotti J, Yamanouchi J, Chilvarquer I, Contin I, Tortamano-Neto P (2012) Measurement of buccal bone volume of dental implants by means of cone-beam computed tomography. Clin Oral Impl Res 23:797–804
Tyndall D, Brooks S (2000) Selection criteria for dental implant site imaging: a position paper of the American Academy of Oral and Maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 89:630–637
Uchida Y, Goto M, Danjo A, Yamashita Y, Kuraoka A (2012) Anatomic measurement of the depth and location of the sublingual fossa. Int J Oral Maxillofac Surg 41:1571–1576
Watanabe H, Mohammad Abdul M, Kurabayashi T, Aoki H (2010) Mandible size and morphology determined with CT on a premise of dental implant operation. Surg Radiol Anat 32:343–349
Woo BM, Al-Bustani S, Ueeck BA (2006) Floor of mouth haemorrhage and life-threatening airway obstruction during immediate implant placement in the anterior mandible. Int J Oral Maxillofac Surg 35:961–964
Acknowledgment
This study was conducted as part of the Ankara University Scientific Research Project No: 12H3334001.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kamburoğlu, K., Acar, B., Yüksel, S. et al. CBCT quantitative evaluation of mandibular lingual concavities in dental implant patients. Surg Radiol Anat 37, 1209–1215 (2015). https://doi.org/10.1007/s00276-015-1493-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-015-1493-9