Abstract
Purpose
The minimally invasive lateral retroperitoneal transpsoas approach is a recent technique developed for lumbar interbody fusion and discectomy. The proximity of the retroperitoneal vessels and ventral nerve roots to the surgical pathway increases the risk of injury to these anatomical structures. A precise knowledge of the regional anatomy of the lumbar plexus is required for safe passage through the psoas muscle. Preoperative examination of the axial MRI images will allow the surgeon to observe the neural structures at the operative levels and confirm that abdominal vessels do not obstruct the lateral disc space. The objective of this study was to determine the anatomic position of the ventral nerve roots and the retroperitoneal vessels in relation to the vertebral body in the degenerative spine and to delineate a safe working zone using magnetic resonance imaging (MRI).
Methods
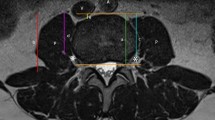
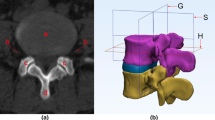
We retrospectively evaluated lumbar spine MRI in 78 patients (from L1–L2 to L4–L5). The total number of lumbar vertebrae measured was 304 levels. Sagittal MRI sections were used to measure disc height (anterior, middle, posterior). Axial MRI sections were used to measure the sagittal and transversal vertebral endplate diameters, the overlap between ventral nerve roots and the posterior border of the lower endplate of the vertebral body, and the overlap between the retroperitoneal vessels and the anterior border of the lower endplate of the vertebral body. The safe zone was subsequently calculated. It was defined as the relative lower endplate vertebral body sagittal diameter that is anterior to the nerve root and is posterior to the retroperitoneal vessels.
Results
The safe working zone was 75.3% of the lower endplate of the vertebral body sagittal diameter at L1–L2, 59.5% at L2–L3, 51.9% at L3–L4 and 37.8% at L4–L5 levels. This area significantly decreases from L1–L2 to L4–L5 (p < 0.05). Compared with L1–L2, L2–L3 levels, the more anterior position of the nerve root and the more posterior position of the retroperitoneal vessels at the L4–L5 level causes a significant reduction of this area. Compared with the L3–L4 level, we observed that the safe zone decrease was simply secondary to the more anterior position of the nerve roots at the L4–L5 level.
Conclusion
Preoperative planning and safe zone delineation are a simple method to assess the relative position of neural and vascular anatomic structures in relation to the surgical area. This method can help spine surgeons to prevent perioperative complications.


Similar content being viewed by others
References
Anand N, Baron EM, Thaiyananthan G, Khalsa K, Goldstein TB (2008) Minimally invasive multilevel percutaneous correction and fusion for adult lumbar degenerative scoliosis: a technique and feasibility study. J Spinal Disord Tech 21:459–467
Baker JK, Reardon PR, Reardon MJ, Heggeness MH (1993) Vascular injury in anterior lumbar surgery. Spine 18:2227–2230
Benglis DM, Vanni S, Levi AD (2009) An anatomical study of the lumbosacral plexus as related to the minimally invasive transpsoas approach to the lumbar spine. J Neurosurg Spine 10:139–144
Bergey DL, Villavicencio AT, Goldstein T, Regan JJ (2004) Endoscopic lateral transpsoas approach to the lumbar spine. Spine 29:1681–1688
Brau SA (2002) Mini-open approach to the spine for anterior lumbar interbody fusion: description of the procedure, results, complications. Spine J 2:216–223
Dakwar E, Cardona RF, Smith DA, Uribe JS (2010) Early outcomes and safety of the minimally invasive, lateral retroperitoneal transpsoas approach for adult degenerative scoliosis. Neurosurg Focus 28:E8
Eck JC, Hodges S, Humphreys SC (2007) Minimally invasive lumbar spinal fusion. J Am Acad Orthop Surg 15:321–329
Fantini GA, Pappou IP, Girardi FP, Sandhu HS, Cammisa FP Jr (2007) Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine 32:2751–2758
Garg J, Woo K, Hirsch J, Bruffey JD, Dilley RB (2010) Vascular complications of exposure for anterior lumbar interbody fusion. J Vasc Surg 51:946–950
Gu Y, Ebraheim NA, Xu R, Rezcallah AT, Yeasting RA (2001) Anatomic considerations of the posterolateral lumbar disk region. Orthopedics 24:56–58
Gumbs AA, Bloom ND, Bitan FD, Hanan SH (2007) Open anterior approaches for lumbar spine procedures. Am J Surg 194:98–102
Hackenberg L, Halm H, Bullmann V, Vieth V, Schneider M, Liljenqvist U (2005) Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 14:551–558
Hasegawa T, Mikawa Y, Watanabe R, An HS (1996) Morphometric analysis of the lumbosacral nerve roots and dorsal root ganglia by magnetic resonance imaging. Spine 21:1005–1009
Knight RQ, Schwaegler P, Hanscom D, Roh J (2009) Direct lateral lumbar interbody fusion for degenerative conditions: early complication profile. J Spinal Disord Tech 22:34–37
Kuklo TR, Lehman RA Jr, Lenke LG (2005) Structures at risk following anterior instrumented spinal fusion for thoracic adolescent idiopathic scoliosis. J Spinal Disord Tech 18:S58–S64
Moro T, Kikuchi S, Konno S, Yaginuma H (2003) An anatomic study of the lumbar plexus with respect to retroperitoneal endoscopic surgery. Spine 28:423–428
Ozgur BM, Aryan HE, Pimenta L, Taylor WR (2006) Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6:435–443
Regev GJ, Chen L, Dhawan M, Lee YP, Garfin SR, Kim CW (2009) Morphometric analysis of the ventral nerve roots and retroperitoneal vessels with respect to the minimally invasive lateral approach in normal and deformed spines. Spine 34:1330–1335
Uribe JS, Arredondo N, Dakwar E, Vale FL (2010) Defining the safe working zones using the minimally invasive lateral retroperitoneal transpsoas approach: an anatomical study. J Neurosurg Spine 13:260–266
Yan DL, Pei FX, Li J, Soo CL (2008) Comparative study of PLIF and TLIF treatment in adult degenerative spondylolisthesis. Eur Spine J 17:1311–1316
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guérin, P., Obeid, I., Gille, O. et al. Safe working zones using the minimally invasive lateral retroperitoneal transpsoas approach: a morphometric study. Surg Radiol Anat 33, 665–671 (2011). https://doi.org/10.1007/s00276-011-0798-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-011-0798-6