Abstract
Background
Section of the right posterior attachment (RPA) of the pancreatic head from the adventicia of the superior mesenteric artery (SMA) is the last step of pancreaticoduodenectomy. This procedure might be technically demanding, time consuming and potentially dangerous. A method using a stapler has been proposed to simplify this step of the pancreaticoduodenectomy.
Methods
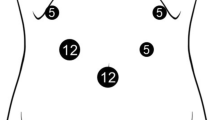
To evaluate the potential consequences of RPA section using this new method, we used an experimental model of pancreaticoduodenectomy in 20 cadavers. After RPA stapling, the residual areolar tissue located between the staple line and SMA was removed (by sub adventicial dissection) and weighed. This allowed an evaluation of: (1) the theoretical risk of SMA injury and (2) the potential carcinological consequences of using stapling division, in comparison with the lymphadenectomy obtained with the conventional sub-adventicial dissection.
Results
A right hepatic artery was accidentaly injured in 10% of cases because of the lack of arterial dissection and arterial anatomy recognition. Forty-three percent of the RPA containing nerves and lymphatics remains in place. Using the stapling technique for RPA division theoretically increases the risk of micro or macroscopically positive margin after surgical resection.
Conclusion
The result of this human cadaver-based dissection suggests that the use of the mechanical stapling device for final division of the RPA might increase the risk of SMA injury. The risk of vascular injury has been reported in surgical literature and is confirmed by this study. Such results (10% of accidentaly injury) may not be representative in leaving human patients, thanks to the use of a detectable palpable pulse of the SMA. The latter is important in avoiding vascular injury during RPA division. This study also shows that this new technique may increase the risk of incomplete tumor resection.







Similar content being viewed by others
References
Dionigi R, Dominioni L, Benevento A, Carcano G (1991) Stapling techniques to facilitate resection of the head of the pancreas. J R Coll Surg Edinb 36:233–237
Ducasse E, Roy F, Chevalier J, Massouille D, Smith M, Speziale F, Fiorani P, Puppinck P (2004) Aneurysm of the pancreaticoduodenal arteries with celiac trunk lesion: current management. J Vasc Surg 39:906–11
Evans DB, Abbruzzese JL, Wilet CG (2001) Cancer of the pancreas. In: De Vita VT, Hellman S, Rosenberg SA (eds) Cancer, principles and practice of oncology. 6th edn. Lippicott Williams and Wilkins, Philadelphia, pp 1126–1161
Evans DB, Pisters PWT (2003) Novel applications of endoGIA linear staplers during pancreaticoduodenectomy and total pancreatectomy. Am J Surg 185:606–607
Heald RJ, Husband EM, Ryall RDH (1982) The mesorectum in rectal cancer surgery-the clue to pelvic recurrence. Br J Surg 69:613–616
Ikard R, Merendino KA (1970) Accidental excision of the superior mesenteric artery. Technical and physiological considerations. Surg Clin North Am 50:1075–85
Jones RM, Hardy KJ (2001) The hepatic artery: a reminder of surgical anatomy. J R Coll Surg Edinb 46:168–70
MacFarlane JK, Ryall RDH, Heald RJ (1993) Mesorectal excision for rectal cancer. Lancet 341:457–60
Nagomey DM, Edis AJ (1981) A use of stapler in pancreatic surgery. Am J Surg 142:384–385
Nano M, Dal Corso H, Ferronato M, Solej M, Hornung JP (2003) Can intestinal innervation be preserved in pancreatoduodenectomy for cancer ? Results of an anatomical study. Surg Radiol Anat 25:1–5
Pissas A (1984) Anatomo-clinical and anatomo-surgical essay on the lymphatic circulation of the pancreas. Anat Clin 6:255–280
Pissas A (1984) Essai d’Anatomie clinique et chirurgicale sur la circulation lymphatique du pancréas. J Chir 121:557–571
Pissas A (1985) La lame rétroportale gauche du pancréas ou lame rétropancréatique gauche. J Chir 122:9–15
Pissas A (1994) Les grandes voies lymphatiques abdominales. In: Chevrel JP (ed) Anatomie clinique. Springer, Paris
Pissas A, Dyon JF, Sarrazin R, Bouchet Y (1979) Le drainage lymphatique de l’estomac. J Chir 116:583–590
Povosky SP (2001) Novel applications of Endo GIA linear stapler during pancreaticoduodenectomy and total pancreatectomy. Am J Surg 182:77–80
Prioton JB, Laux R (1960) La lame rétroportale du pancréas céphalique. Incidences de sa topographie en chirurgie pancréatique et portale. Cr Ass Anat 108:667–673
Richelme H, Michetti C, Birttwisle Y, Bourgeon A (1986) La section de la lame rétropancréatique droite au cours de la duodénopancréatectomie céphalique. Ann Chir 40:401–404
Stojadinovic A, Brooks A, Hoos A, Jaques DP, Conlon KC, Brennan MF (2003) An evidence-based approach to the surgical management of resectable pancreatic adenocarcinoma. J Am Coll Surg 196:954–964
Yeo CJ, Cameron JL, Lillemoe KD, Sohn TA, Campbell KA, Sauter PK, Abrams RA, Hruban RH (2002) Pancreatectomy with or without distal gastrectomy and extended retroperitoneal lymphadenectomy for periampullary adenocarcinoma, part 2: randomized controlled trial evaluating survival, morbidity, and mortality. Ann Surg 236:355–366
Yoschioka H, Wakabayshi T (1941) Traitement de la douleur des pancréatites chroniques par la neurotomie de la tête du pancréas. Lyon Chir 38:114–612
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baqué, P., Iannelli, A., Delotte, J. et al. Division of the right posterior attachments of the head of the pancreas with a linear stapler during pancreaticoduodenectomy: vascular and oncological considerations based on an anatomical cadaver-based study. Surg Radiol Anat 31, 13–17 (2009). https://doi.org/10.1007/s00276-008-0353-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-008-0353-2