Abstract
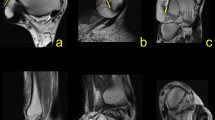
The purpose of the present study was to describe the anatomical structure of the tibiofibular syndesmosis. Dissection of the tibiofibular syndesmosis was performed on 30 cadaveric specimens of the ankle in adults. The stability of the tibiofibular mortise is ensured by three ligaments. The interosseous tibiofibular ligament forms a spatial network of fibers of a pyramidal shape filled with fibrofatty tissue. The anterior tibiofibular ligament consists of three parts: the upper one is the shortest, the medial one is the strongest and the lower part is the longest and the thinnest. The posterior tibiofibular ligament is a strong, compact ligament the lower margin of which literally forms the articular labrum for the lateral ridge of the trochlea of the talus. The so-called inferior transverse tibiofibular ligament, as this part of the ligament is sometimes characterized, cannot be considered as a separate ligament. Direct contact between the distal tibia and the fibula was found in 23 cases. Contact facets which were covered with articular cartilage were very small and located in the anterior half of the tibiofibular contact line. In the posterior part of the tibiofibular contact line a vertical V-shaped synovial plica attached by its lateral aspect to the fibula dipped between the two bones. In seven cases where there was no direct contact between the two bones this plica extended anteriorly to the anterior tibiofibular ligament. The findings show that in three quarters of cases the connection of the distal tibia and fibula is not a mere syndesmosis but also a synovial joint. The presented facts change traditional opinions on the structure of the tibiofibular syndesmosis and they should be reflected in the treatment of dislocation-fractures of the ankle as well as in case of so-called anterolateral ankle impingement.
Résumé
Le but du présent travail était de décrire la structure anatomique de la syndesmose tibio-fibulaire. La dissection de la syndesmose tibio-fibulaire a été réalisée sur 30 spécimens cadavériques de chevilles d'adultes. La stabilité de la mortaise tibio-fibulaire est assurée par trois ligaments. Le ligament tibio-fibulaire interosseux forme un réseau spatial de fibres, de forme pyramidale, dont les mailles sont remplies de tissu fibro-adipeux. Le ligament tibio-fibulaire antérieur est formé de trois parties; la partie supérieure est la plus courte, la partie médiale est la plus forte et la partie inférieure est la plus longue et la plus mince. Le ligament tibio-fibulaire postérieur est un fort ligament compact dont le bord inférieur forme littéralement un labrum articulaire destiné à la berge latérale de la trochlée du talus. Ce qui est classiquement appelé " ligament tibio-fibulaire transverse inférieur", comme on le dénomme parfois, ne peut être considéré comme un ligament séparé. Un contact direct entre l'extrémité distale du tibia et de la fibula a été trouvé dans 23 cas. Les facettes en contact, recouvertes de cartilage articulaire, étaient très petites et situées sur la moitié antérieure de la ligne de contact tibio-fibulaire. Sur la partie postérieure de la ligne de contact tibio-fibulaire, un repli synovial vertical en forme de V, attaché par son bord latéral à la fibula, plonge entre les deux os. Dans 7 cas où il n'y avait pas de contact direct entre les deux os, ce repli s'étendait vers l'avant jusqu'au ligament tibio-fibulaire antérieur. Nos constatations montrent que, dans trois quarts des cas, l'articulation entre la partie distale du tibia et celle de la fibula n'est pas une syndesmose pure, mais qu'il s'agit aussi d'une articulation synoviale. Les faits que nous présentons changent les idées traditionnelles sur les structures de la syndesmose tibio-fibulaire et ils devraient trouver des applications, principalement dans le traitement des luxations-fractures de la cheville, ainsi que dans les cas de ce que l'on désigne sous le terme de "conflit antéro-latéral de la cheville".





Similar content being viewed by others
References
Akseki D, Pinar H, Bozkurt M, Yaldiz K, Arac S (1992) The distal fascicle of the anterior inferior tibiofibular ligament as a cause of anterolateral ankle impingement. Acta Orthop Scand 70: 478–482
Barnett CH, Napier JR (1952) The axis of rotation at the ankle joint in man. Its influence upon the form of the talus and the mobility of the fibula. J Anat 86: 1–9
BartonŢček J, Doskočil M, Heřt J, Sosna A (1991) Chirurgická anatomie velkých končetinových kloubů. (Surgical anatomy of great limb joints) Avicenum, Prague, pp 217–230
Bassett FH, Gates HS, Billys JB, Morris HB, Nikolau PK (1990) Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am 72: 55–59
Boden SD, Labradopoulos PA, McCowin P, Lestini WF, Hurwitz SR (1989) Mechanical consideration for the syndesmosis screw. A cadaver study. J Bone Joint Surg Am 71: 1548–1555
Carr JB, Trafton PG (1998) Malleolar fractures and soft tissue injuries of the ankle. In: Browner BD, Jupiter JB, Levine AM, Trafton PG (eds) Skeletal trauma, vol 2. Saunders, Philadelphia, pp 2327–2404
Close JR (1956) Some applications of the functional anatomy of the ankle joint. J Bone Joint Surg Am 38: 761–781
Doskočil M (1988) DistálnŢ spojenŢ tibie a fibuly nenŢ jen syndesmoza. (Distal connection of the tibia and fibula is not only a syndesmosis.) SbornŢk lékařský 90: 1–7
Fick R (1904) Handbuch der Anatomie und Mechanik der Gelenke unter Berücksichtigung der bewegenden Muskeln. Part 1: Anatomie der Gelenke. Fischer, Jena, pp 440–421
Frazer JE (1946) The anatomy of the human skeleton, 4th edn. J & A Churchill, London, pp 130–137
Geisler WB, Tsao, MAK, Hughes, JL (1996) Fractures and injuries of the ankle. In: Rockwood ChA, Green DP, Bucholz RW, Heckeman JD (eds) Fractures in adults, vol 2, 4th edn. Lippincott-Raven, Philadelphia New York, pp 2201–2266
Grass R, Herzmann K, Biewener A, Zwipp H (2000) Verletzungen der unteren tibiofibularen Syndesmose. Unfallchirurgie 103: 520–532
Hamilton WC (ed) (1978) Traumatic disorders of the ankle. Springer, Berlin Heidelberg New York, pp 1–12
Heim U (1983) Malleolarfrakturen. Unfallheilkunde. 86: 248–258
Höcker K, Pachucki (1989) Die Incisura fibularis tibiae. Die Stellung der Fibula in der distalen Syndesmose am Querschnitt. Unfallchirurgie 92: 401–406
Jaeger M, Wirth CJ (1978) Kapselbandlaesionen. Thieme, Stuttgart, pp 82–191
Johnston TB, Davies DV, Davies F (eds) (1958) Gray´s anatomy, 32nd edn. Longmans Green, London, pp 530–536
Kelikian H, Kelikian AS (1952) Disorders of the ankle. Saunders, Philadelphia, pp 1–91
Kopsch F (1952) Rauber-Kopsch Lehrbuch und Atlas der Anatomie des Menschen, vol 1, 16th edn. Thieme, Leipzig, pp 423–427
Kos J (1957) CévnŢ zásobenŢ pouzdra hlezenného kloubu. (Blood supply of the articular capsule of the ankle.) Čs Morf 5: 80–93
Lanz T von, Wachsmuth W (1938) Praktische Anatomie, vol 1, part 4: Bein und Statik. Springer, Berlin Heidelberg New York, pp 338–347
Leeds HC, Ehrlich MG (1984) Instability of the distal tibiofibular syndesmosis after bimalleolar and trimalleolar ankle fractures. J Bone Joint Surg Am 66: 490–503
Lutz W (1942) Zur Struktur der unteren Tibiofibularverbindung und der Membrana interossea cruris. Anat Entwickl Gesch 111: 315–321
Michelson JD (1995) Current concepts review. Fractures about the ankle. J Bone Joint Surg Am 77: 142–152
Monk CJE (1969) Injuries of the tibio-fibular ligaments. J Bone Joint Surg Br 51: 330–337
Tillmann B, Bartz B, Schleicher A (1985) Stress in the human ankle joint: a brief review. Arch Orthop Trauma Surg 103: 385–391
Vander Gried R, Michelson JD, Bone LB (1996) Fractures of the ankle and the distal part of the tibia. J Bone Joint Surg Am 78: 1772–1783
Weber BG (1966) Die Verletzungen des oberen Sprunggelenkes. Huber, Bern, pp 20–23
Weinert CR, McMaster JH, Ferguson RJ (1973) Dynamic function of the human fibula. Am J Anat 138: 145–150
Xenos JS, Hopkins WJ, Mulligan ME, Olson EJ (1995) The tibiofibular syndesmosis. J Bone Joint Surg Am 77: 847–856
Zwipp H (1994) Chirurgie des Fusses. Springer, Berlin Heidelberg New York, pp 12–45
Acknowledgement
This study was supported by the Research Goal of the 3rd Faculty of Medicine of Charles University: J 13/98:111 2000 3.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Bartoníček, J. Anatomy of the tibiofibular syndesmosis and its clinical relevance. Surg Radiol Anat 25, 379–386 (2003). https://doi.org/10.1007/s00276-003-0156-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00276-003-0156-4