Abstract
Purpose
Using a pig model: (1) to evaluate the vascular distribution pattern, including the homogeneity and completeness of the intra-arterial microsphere distribution, of 40–120-μm trisacryl-gelatin microspheres (Embospheres) in acute whole-kidney embolization; (2) to evaluate the durability and biocompatibility of 40–120-μm trisacryl-gelatin microspheres (Embospheres) in chronic partial kidney embolization.
Methods
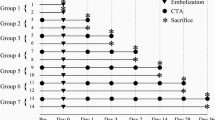
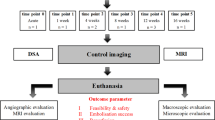
Twenty-two animals were divided into four groups: group 1 (n = 4) underwent total arterial renal occlusion with immediate euthanasia. Groups 2–4 had chronic superselective and partial renal embolization with increasing follow-up times: group 2 (n = 2), 1 week; group 3 (n = 7), 4 weeks; and group 4 (n = 9), 14 weeks. Key endpoints in group 1 were homogeneity and completeness of acute embolizations. In groups 2–4 the key endpoints were durability of embolization and particle-related inflammation in chronic partial embolizations as assessed by quantitative angiography or histomorphometry. A numerical angiographic occlusion score (0.0 to 4.0, where 3.0 is optimal) was developed to assess and quantify the angiographic durability of superselective embolizations (groups 2–4).
Results
In group 1, a relatively homogeneous distribution of the particles from segmental arteries to the precapillary level was shown by histomorphometry. Some particles reached the glomerular vas afferens (10 μm diameter). In groups 2–4, a mild recanalization appeared during follow-up. The immediate average postembolization occlusion score of 3.18 ± 0.73 was reduced to 1.44 ± 0.73 (statistically significant). Microscopy revealed subtotal necrosis but no foreign body granuloma formation. The intra-arterial appearance of giant cells closely attaching to the surface of the embolic spheres inside the vessel lumen was noted. Vessel walls showed major ischemic reactions.
Conclusion
Microspheres 40–120 μm in diameter might achieve total occlusion of the arterial kidney vasculature when injected centrally as a result of their fairly homogeneous distribution. Segmental renal infarction occurs after chronic partial embolization despite recanalizations during follow-up. Only mild specific intra-arterial foreign body reactions were found.







Similar content being viewed by others
References
Goodwin SC, Vedantham S, McLucas B, et al. (1997) Preliminary experience with uterine artery embolization for uterine fibroids. J Vasc Interv Radiol 8:517–526
Bradley EA, Reidy JF, Forman RG, et al. (1998) Transcatheter uterine artery embolization to treat large uterine fibroids. Br J Obstet Gynaecol 105:235–240
Goodwin SC, McLucas B, Lee M, et al. (1999) Uterine artery embolization for the treatment of uterine leiomyomata midterm results. J Vasc Interv Radiol 10:1159–1165
Nikolic B, Spies JB, Abbara S, et al. (1999) Ovarian artery supply of uterine fibroids as a cause of treatment failure after uterine artery embolization: a case report. J Vasc Interv Radiol 10:1167–1170
Siskin GP, Eaton LA Jr, Stainken BF, et al. (1999) Pathologic findings in a uterine leiomyoma after bilateral uterine artery embolization. J Vasc Interv Radiol 10:891–894
Spies JB, Scialli AR, Jha RC, et al. (1999) Initial results from uterine fibroid embolization for symptomatic leiomyomata. J Vasc Interv Radiol 10:1149–1157
Siskin GP, Englander M, Stainken BF, et al. (2000) Embolic agents used for uterine fibroid embolization. AJR Am J Roentgenol 175:767–773
Pelage JP, Le Dref O, Beregi JP, et al. (2003) Limited Uterine Artery Embolization with Tris-acryl Gelatin Microspheres for Uterine Fibroids. J Vasc Interv Radiol 14:15–20
Beaujeux R, Laurent A, Wassef M, et al. (1996) Trisacryl gelatin microspheres for therapeutic embolization, II: preliminary clinical evaluation in tumors and arteriovenous malformations. AJNR Am J Neuroradiol 17:541–548
Han YM, Kim JK, Roh BS, et al. (1997) Renal angiomyolipoma: selective arterial embolization—effectiveness and changes in angiomyogenic components in long-term follow-up. Radiology 204:65–70
Kauffmann GW, Rohrbach R, Richter G, et al. (1984) Kidney tumor embolization. Progress, experiences and complications. Urologe A 23:109–116
Richter G, Rassweiler J, Kauffmann GW, et al. (1984) Experimental study of the effectiveness of capillary embolization using contrast-enhanced Ethibloc. Invest Radiol 19:36–44
Kauffmann GW, Richter GM, Rohrbach R, et al. (1989) Prolonged survival following palliative renal tumor embolization by capillary occlusion. Cardiovasc Intervent Radiol 12:22–28
Kauffmann GW, Richter GM, Roeren TK (1992) Renal tumor embolization. Radiologe 32:127–131
Hansmann HJ, Hallscheidt P, Aretz K, et al. (1999) Renal tumor embolization. Radiologe 39:783–789
Livraghi T (2003) Radiofrequency ablation, PEIT, and TACE for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg 10:67–76
Miyayama S, Matsui O, Nishida H, et al. (2003) Transcatheter arterial chemoembolization for unresec Table hepatocellular carcinoma fed by the cystic artery. J Vasc Interv Radiol 14:1155–1161
Sugo H, Futagawa S, Beppu T, et al. (2003) Role of preoperative transcatheter arterial chemoembolization for resec Table hepatocellular carcinoma: relation between postoperative course and the pattern of tumor recurrence. World J Surg 27:1295–1299
Spies JB (2003) Uterine artery embolization for fibroids: understanding the technical causes of failure. J Vasc Interv Radiol 14:11–14
Pelage JP, Laurent A, Wassef M, et al. (2002) Uterine artery embolization in sheep: comparison of acute effects with polyvinyl alcohol particles and calibrated microspheres. Radiology 224:436–445
Siskin GP, Dowling K, Virmani R, et al. (2003) Pathologic evaluation of a spherical polyvinyl alcohol embolic agent in a porcine renal model. J Vasc Interv Radiol 14:89–98
Derdeyn CP, Graves VB, Salamat MS, et al. (1997) Collagen-coated acrylic microspheres for embolotherapy: in vivo and in vitro characteristics. AJNR Am J Neuroradiol 18:647–653
Bendszus M, Klein R, Burger R, et al. (2000) Efficacy of Trisacryl Gelatin Microspheres versus Polyvinyl Alcohol Particles in the Preoperative Embolization of Meningiomas. AJNR Am J Neuroradiol 21:255–261
Laurent A, Beaujeux R, Wassef M, et al. (1996) Trisacryl gelatin microspheres for therapeutic embolization, I: development and in vitro evaluation. AJNR Am J Neuroradiol 17:533–540
Laurent A, Wassef M, Saint Maurice JP, et al. (2006) Arterial distribution of calibrated tris-acryl gelatin and polyvinyl alcohol microspheres in a sheep kidney model. Invest Radiol. 41:8–14
Ng HK, Poon WS, Goh K, et al. (1996) Histopathology of post-embolized meningiomas. Am J Surg Pathol 20:1224–1230
Acknowledgment
This work was supported by a research grant from Biosphere Medical, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stampfl, S., Stampfl, U., Rehnitz, C. et al. Experimental Evaluation of Early and Long-Term Effects of Microparticle Embolization in Two Different Mini-Pig Models. Part I: Kidney. Cardiovasc Intervent Radiol 30, 257–267 (2007). https://doi.org/10.1007/s00270-005-0309-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-005-0309-4