Abstract
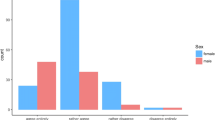
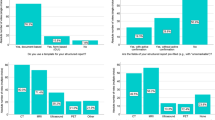
Purpose: Official recommendations for obtaining informed consent for interventional radiology procedures are that the patient gives their consent to the operator more than 24 hr prior to the procedure. This has significant implications for interventional radiology practice. The purpose of this study was to identify the proportion of European interventional radiologists who conform to these guidelines. Methods: A questionnaire was designed consisting of 12 questions on current working practice and opinions regarding informed consent. These questions related to where, when and by whom consent was obtained from the patient. Questions also related to the use of formal consent forms and written patient information leaflets. Respondents were asked whether they felt patients received adequate explanation regarding indications for intervention, the procedure, alternative treatment options and complications. The questionnaire was distributed to 786 European interventional radiologists who were members of interventional societies. The anonymous replies were then entered into a database and analyzed. Results: Two hundred and fifty-four (32.3%) questionnaires were returned. Institutions were classified as academic (56.7%), non-academic (40.5%) or private (2.8%). Depending on the procedure, in a significant proportion of patients consent was obtained in the outpatient department (22%), on the ward (65%) and in the radiology day case ward (25%), but in over half (56%) of patients consent or re-consent was obtained in the interventional suite. Fifty percent of respondents indicated that they obtain consent more than 24 hr before some procedures, in 42.9% consent is obtained on the morning of the procedure and 48.8% indicated that in some patients consent is obtained immediately before the procedure. We found that junior medical staff obtained consent in 58% of cases. Eighty-two percent of respondents do not use specific consent forms and 61% have patient information leaflets. The majority of respondents were satisfied with their level of explanation regarding indications for treatment (69.3%) and the procedure (78.7%). Fifty-nine percent felt patients understood alternative treatment options. Only 37.8% of radiologists document possible complications in the patient’s chart. Comments from respondents indicated that there is insufficient time for radiologists to obtain consent in all patients. Suggestions to improve current local policies included developing the role of radiology nursing staff and the use of radiology outpatient clinics. Conclusions: More than 50% of respondents are unhappy with their policies for obtaining informed consent. Interventional societies have a role to play in advocating formal consent guidelines.

Similar content being viewed by others
References
MJ O’Sullivan HP Redmond (2001) ArticleTitleInformed consent in Ireland: where are we now? J Irish Coll Phys Surg 30 3
JF Merz (1991) ArticleTitleAn empirical analysis of the medical informed consent doctrine: search for a “standard” of disclosure. RISK 2 27
The Medical Defence Union of Ireland (1999) Consent to treatment. MDU, Ireland
General Medical Council (1999) Seeking patients’ consent: the ethical considerations. GMC, London
Marchant J (2000) Informed consent helps minimize litigation risk. Diagnostic Imaging Europe
DJ Byrne A Napier A Cuschieri (1988) ArticleTitleHow informed is signed consent? BMJ (Clin Res Ed) 296 839–840 Occurrence Handle1:STN:280:BieB383ntF0%3D
C Lavelle-Jones DJ Byrne P Rice A Cuschieri (1993) ArticleTitleFactors affecting quality of informed consent. BMJ 306 885–890 Occurrence Handle1:STN:280:ByyB2MjpvFw%3D Occurrence Handle8490411
G Trotteur L Stockx RF Dondelinger (2000) ArticleTitleSedation, analgesia and anesthesia for interventional radiological procedures in adults. 1. Survey of interventional radiological practice in Belgium. JBR-BTR 83 111–115 Occurrence Handle1:STN:280:DC%2BD3cvnvVSmsw%3D%3D Occurrence Handle11025921
MH Edwards (1990) ArticleTitleSatisfying patients’ needs for surgical information. Br J Surg 77 463–465 Occurrence Handle1:STN:280:By%2BB2MvjvFw%3D Occurrence Handle2340401
PJ Dawes P Davison (1994) ArticleTitleInformed consent: what do patients want to know? J R Soc Med 87 149–152 Occurrence Handle1:STN:280:ByuB3M%2Fkt1w%3D Occurrence Handle8158593
BM Stanley DJ Walters GJ Maddern (1998) ArticleTitleInformed consent: how much information is enough? Aust N Z J Surg 68 788–791 Occurrence Handle1:STN:280:DyaK1M%2FivFyrsg%3D%3D Occurrence Handle9814743
AP Armstrong AA Cole RE Page (1997) ArticleTitleInformed consent: are we doing enough? Br J Plast Surg 50 637–640 Occurrence Handle10.1016/S0007-1226(97)90510-5 Occurrence Handle1:STN:280:DyaK1c3ns1emtw%3D%3D Occurrence Handle9613407
D Mulcahy K Cunningham D McCormack N Cassidy M Walsh (1997) ArticleTitleInformed consent from whom? J R Coll Surg Edinb 42 161–164 Occurrence Handle1:STN:280:ByiA3sbisFU%3D Occurrence Handle9195806
DJ Houghton S Williams JD Bennett G Back AS Jones (1997) ArticleTitleInformed consent: patients’ and junior doctors’ perceptions of the consent procedure. Clin Otolaryngol 22 515–518 Occurrence Handle10.1046/j.1365-2273.1997.00059.x Occurrence Handle1:STN:280:DyaK1c7islajug%3D%3D Occurrence Handle9466060
JS Huntley DA Shields NK Stallworthy (1998) ArticleTitleConsent by the junior house officer: is it informed? J R Soc Med 91 528–530 Occurrence Handle1:STN:280:DyaK1M7mvFGhtw%3D%3D Occurrence Handle10070372
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
O’Dwyer, H., Lyon, S., Fotheringham, T. et al. Informed Consent for Interventional Radiology Procedures: A Survey Detailing Current European Practice . CVIR 26, 428–433 (2003). https://doi.org/10.1007/s00270-003-0058-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-003-0058-1