Abstract
Background
In the Netherlands, there are no specialized or certified pediatric trauma centers, especially for severely injured children. National and regional agreements on centralization of pediatric trauma care are scarce. This study aims to describe the incidence, injury mechanism and in-hospital mortality of pediatric trauma in the Netherlands, as a prelude to the further organization of pediatric trauma care.
Methods
A retrospective cohort analysis of data from the Dutch National Trauma Registry in 2009–2018, concerning all children (0–16 years) hospitalized due to injury in the Netherlands.
Results
The annual number of admitted injured children increased from 8666 in 2009 to 13,367 in 2018. Domestic accidents were the most common cause of non-fatal injury (67.9%), especially in children aged 0–5 years (89.2%). Severe injury (injury severity score ≥ 16) accounted for 2.5% and 74% of these patients were treated in level-1 trauma centers. In both deceased and surviving patients with severe injuries, head injuries were the most common (72.1% and 64.3%, respectively). In-hospital mortality after severe injury was 8.2%. Road-traffic accidents (RTAs) were the leading cause of death (46.5%).
Conclusions
Domestic accidents are the most common cause of injury, especially in younger children, whereas RTAs are the lead cause of fatal injury. Severe pediatric trauma in the Netherlands is predominantly managed in level-1 trauma centers, where a multidisciplinary team of experts is available. Improving the numbers of severely injured patients primarily brought to level-1 trauma centers may help to further reduce mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since 2000, an average number of 80 children younger than 15 years old have died due to unintentional injuries each year in the Netherlands [1]. Regional studies showed that about 80% of the children that survive severe injuries in the Netherlands recover well, whereas 20% remain disabled to some extent after long-term follow-up [2, 3].
In 1999/2000, the Dutch trauma care system was regionalized with dedicated trauma centers appointed per region [4]. As a result, the injury-related in-hospital mortality rate in children aged 13–18 years has decreased over the period 1996–2006. However, no change was observed for children younger than 12 years. Injury prevention strategies, such as road safety regulations, have also led to a decrease in mortality related to some types of childhood injuries. In 2018, 19 children had died in a road-traffic accident in the Netherlands; on average 46 less fatalities per year than in the period 1996–2000 [5], due to improved road and traffic safety over the last decade.
Trauma care in children is fundamentally different from that in adults, because of their anatomical and physiological dissimilarities [6]. In the Netherlands, there are no specialized pediatric trauma centers and severely injured children are treated in any of the level-1 trauma centers. This may affect the outcome of care, especially for severely injured children, since it has been proven difficult to provide optimal pediatric trauma care without adequate experience [7].
The objective of this study is to describe the current epidemiology of pediatric trauma in the Netherlands, since an up-to-date overview is lacking. By analyzing data from the Dutch National Trauma Registry (DNTR), we aimed to determine the incidence of pediatric injury, and to identify trends in cause of injury, injury patterns and outcome of pediatric patients who were admitted to a hospital after trauma. Insight in these data will help to further optimize pediatric patient trauma care as well as trauma prevention on a national level in the Netherlands.
Material and methods
Study design and population
This retrospective cohort study analyzed data obtained from the DNTR, which was established in 2007 and includes information from all Dutch hospitals of patients admitted due to injury [8]. All pediatric patients aged 0 to 16 years who were admitted to one of the Dutch hospitals due to injury between January 1st, 2009, and December 31st, 2018, were included.
Data collection
The primary outcome of this study was in-hospital mortality. Secondary outcomes were length of hospital stay (LOHS) and admittance to the intensive care unit (ICU). Other data included age, sex, type of hospital (trauma (level-1) vs. non-trauma center), injury characteristics (injury mechanism, injury type, abbreviated injury scale (AIS) score, injury severity score (ISS)) and vital signs on admission to the Emergency Department (ED) (Glasgow Coma Scale (GCS), respiratory rate (RR), systolic blood pressure (SBP)). In the DNTR, injuries are classified according to the AIS98 (up to 2015) and AIS08 (since 2015).
Definitions
Patients with an ISS ≥ 16 and ISS ≥ 25 were considered as severely and critically injured, respectively [9]. A GCS of 13–15 corresponds with mild head injury, 9–12 with moderate head injury and 3–8 with severe head injury. Normal values for systolic blood pressure and respiratory rate vary per age group [10]. For each age category, values below normal were considered low and values above normal were considered high.
Statistical analysis
To allow comparisons between age groups, children were divided in three age categories (0–5, 6–11, 12–16 years old). Categorical data were presented as number and percentage and compared using the Chi-square test. Injury severity scores were presented as median (interquartile range [IQR]) and compared using the Mann–Whitney test or Kruskal–Wallis test for independent samples. Additional analyses compared deceased and survived children and children treated in trauma vs. non-trauma centers. Missing data in this descriptive study were not accounted for in the analysis. The statistical analyses were performed in SPSS (IBM Corp. Released 2020. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp).
No formal approval from the Institutional Review Boards was necessary, since only summarized data from the DNTR were obtained.
Results
Total admitted pediatric trauma population
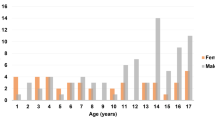
The annual number of admitted injured children increased from 8666 in 2009 to 13,367 in 2018 (Fig. 1). During the study period, a total of 129,840 children were hospitalized due to injury, of whom 23.1% were treated in a level-1 trauma center (Table 1). The largest group was the 0–5-year-old group (44.9%). Over time, the proportion of hospitalized children aged 0–5 years increased and decreased for children aged 12–16 years (Fig. 2). Boys represented 58.8% of the population and formed the majority in all age categories (Table 1). Sex distribution remained unaltered over time.
Penetrating trauma was rare in each age group, but highest in the 12-16-year-old group (3.7%) (Table 1). Domestic accidents were the most common injury mechanism in children aged 0–11 years. The proportion of hospitalized children due to sport-related accidents and RTAs increased with age (Table 1). The distribution of other types of injury mechanisms was stable over time (Fig. 3).
Children aged 0–5 years were the least severely injured (Table 1). In 2015–2018, ISS was lower in all age categories compared to 2009–2014 due to the switch in the DNTR to AIS version 2008 in 2015 (Table 1).
Severely injured (ISS ≥ 16) pediatric trauma population
Characteristics per age group and injury mechanism.
Severe injury accounted for 2.5% of all pediatric injury-related hospital admissions and children aged 12–16 years formed the largest age group in this population (44%) (Table 2). The majority in each age group were boys (62.8% in the total group). The age distribution of the severely injured children varied somewhat over time (Fig. 2).
RTAs were the leading injury mechanism in severely injured children aged 12–16 years (59.8%), while domestic accidents (41.3%) were most common in children 0–5 years (74.5%) and children aged 6–11 years (44.8%) (Table 2). Over time, the proportion of children with severe injury due to RTAs increased and there was a decrease in the proportion of children with severe injury due to domestic accidents (Fig. 3).
Children aged 12–16 years with severe injury had the highest median ISS: 21 (IQR 17–25) for the years 2009–2014 and 22 (IQR 17–26) for the years 2015–2018 (Table 2). More than one-third of the severely injured population was critically injured (ISS ≥ 25). This proportion differed significantly by age group (Table 2) and injury mechanism (Table 3).
Head injuries were the most common severe injuries (AIS ≥ 3) (65%, Table 2). Severe injuries to the head and external injuries were the most frequent in children 0–5 years, whereas severe injuries to the face, thorax, abdomen, spine and extremities were more common in older children (Table 2). Severe head injury was present in the majority of children with severe injury after RTAs, domestic accidents and violent accidents (Table 3). About 20% of the severely injured children had severe injuries to the thorax and abdomen, mostly after RTAs, sport accidents (abdomen), self-harm (thorax), and violent accidents (Table 3).
Vital signs of severely injured children differed between the age groups. Age-specific low respiratory rates and high systolic blood pressure were more common in the youngest age group (Table 2). Children 12–16 years had the longest LOHS (median 6 days) and were admitted most often to the ICU (63%), whereas children 0–5 years had the shortest LOHS (median 4 days) and were less frequently admitted to the ICU (58%, Table 2).
Trauma center admission
Seventy-four percent of the severely injured children were treated in a level-1 trauma center (Table 2). Severely injured children who were injured in an RTA, had a lower level of consciousness (GCS < 13), high RR, low SBP, higher ISS and severe injuries to the head, thorax, spine and lower extremities were more likely to be treated in a level-1 trauma center (Table 4). Consequently, severely injured children who were treated in a trauma center were longer hospitalized, were more frequently admitted to the ICU and had a higher mortality rate than those treated in a non-trauma center. Severely injured children who suffered a domestic or sport-related accident or had severe abdominal injury were more likely to be treated in a non-trauma center.
In-hospital mortality
In the study period 2009–2018, 262 (8.2%) of the children with severe injuries died in the hospital (Table 2), mostly after an RTA or domestic accident (Table 5). Most of them were critically injured (ISS ≥ 25: 89.2% in the years 2009–2014; 93.5% in the years 2015–2018) and were in a coma (93.9% with GCS of 3–8). Nearly half of them were hypotensive on hospital admission (49.3%) (Table 5). Non-survivors more frequently had severe injuries to the head, neck, thorax and spine, as well as more severe external injuries (Table 5).
Discussion
The annual number of registered pediatric injury-related hospitalizations in the Netherlands increased by nearly 60% from 2009 to 2014 and remained stable thereafter. This trend may predominantly be explained as an artifact, because the hospital participation rate in the DNTR increased from 64% in 2007 to 100% in 2015 [11]. Since 2015, the registration of patients admitted due to injury in the DNTR is near complete. Children aged 0–5 years accounted for an increasing part of all hospital admissions due to injury, which may be caused by the fact that young children are more likely to be admitted as a precaution than older ones [12].
Domestic accidents were the most common injury mechanism in children. Prevention of such injuries remains a global challenge [13]. Parent-focused strategies and product and environmental modifications have been proven effective in preventing childhood injuries [14, 15]. Modifications in the child’s environment such as the installment of stair gates, window guards and smoke alarms, childproofing caps on medication packaging, securing cabinets on walls and fencing a pool are some important first steps in home-injury prevention. Also, home visits by professionals can help improve the home environment and provide parents with information on safety equipment [16]. In the Netherlands, the Consumer and Safety Institute VeiligheidNL provides information to both parents and professionals regarding children’s safety and injury prevention [17]. In cooperation with the Ministry of Public Health, they organize trainings, campaigns and behavioral interventions with national, regional and local authorities. Active participation of local authorities to enhance the role of this organization may further help spreading awareness on childhood injury and prevention. Implementation of preventative measures is challenging, however. In addition to information campaigns, legal requirement and enforcement of prevention measures that are proven effective are necessary where possible.
In children aged 12–16 years, RTAs were the main cause of injury (60% of the cases). Children in this age group commonly bicycle unsupervised, making them more vulnerable in daily road traffic. Besides bicycling, use of light mopeds (two-wheeled vehicle) is quite common among Dutch 16-year-old children. Both modes of transportation do not require helmet use and make children at this age prone to head injury in RTAs. As observed in other studies, most RTA-related deaths in Dutch children involved children either as cyclists or pedestrians [18], while the majority of light-moped riders involved in fatal crashes between 2010 and 2015 were 16–17 years old [19].
Improvements in both road infrastructure and vehicle safety such as reducing the speed limit in areas where and at times when children and motorized traffic meet and introducing autonomous emergency braking systems with cyclist/pedestrian recognition will help to increase children’s safety in traffic [20]. For years, the obligatory use of bicycle helmets for Dutch children has been a matter of discussion. Bicycle helmets are still not obligatory because of the fear that this will strongly decrease bicycling, while this is good exercise for children. In our study, severe head injury was present in 65% of the total group of severely injured children and in 72% of the severely injured children that died in the hospital. Weijermars et al. [21] calculated that if all children under 12 years were to wear a bicycle helmet in the Netherlands, this could annually prevent up to 5 casualties and approximately 200 cases with survivable severe road-traffic injuries.
Even though the majority of the severely injured children were treated in a trauma center, 26% were treated in a non-trauma center, suggesting that further centralization of pediatric trauma in the Netherlands is necessary. Centralization of Dutch trauma care started in 1999 and since then treatment of severely injured patients including children has shifted to level-1 trauma centers, resulting in a regional reduction of 50% in crude mortality of trauma patients [22]. The goal of further centralization of care is not only to further reduce mortality but also to optimize outcomes of severely injured children who survive by offering timely and optimal diagnostics and treatment. The American College of Surgeons Committee on Trauma (ACS-COT) recommends a maximum undertriage rate of 5% in polytrauma patients [23], while in the Netherlands, this is 10% [22]. In pediatric trauma, undertriage rates often exceed 20%, which is mostly caused by differences in triage protocols [24, 25]. Currently, the Dutch National Protocol of Ambulance Services and Field Triage Decision Scheme triage protocols are used in pediatric field triage in the Netherlands. Recent studies revealed that both protocols cannot meet current sensitivity targets but also cannot accurately distinguish between low-risk and high-risk trauma patients [26, 27]. Accordingly, the development of a sensitive and child-specific triage protocol is needed in order to prevent undertriage in severely injured children.
Overall in-hospital mortality (0.2%) was low compared to other European countries and the USA (Spain, 0.5%; Norway, 1%; the USA, 1.2%; the UK, 3.7%; Switzerland, 5.5%; Denmark, 7.3%), and mortality after severe injury (8.2%) was comparable to mortality for similar patients in other countries (the USA, 3.2%; Spain, 12.8%; Germany, 13.4%; Switzerland, 17.5%) [28,29,30,31,32,33,34,35]. This suggests that the quality of early pediatric trauma care in the Netherlands is high, including short prehospital times, advanced trauma care at the accident site, designation of trauma centers, improvements in intensive care, assessing of all injured patients according to ATLS guidelines and ‘quick’ interhospital transfers [36].
There are some limitations to take into consideration when interpreting the results of this study. The first limitation is the missing data for some of the cases. Variables with the highest percentages of missing values were mechanism of injury (39% in the total group and 46% in the severely injured group) and physiological variables (GCS 15%, RR 30%, SBP 14% in the severely injured patients), while the remaining variables were complete for 90–100% of the cases (Tables 1–2). Missing values for mechanism of injury were considered to be missing at random. Physiological variables may be missing not at random, since values within the normal clinical range are more likely not to be reported in the medical files. We assume that the reasons for missingness of data were not different in the subgroups of patients that were described, so that Tables 1–3 offer a fair comparison of these subgroups. Heinänen et al. and Ali et al. reported a 97% and 61% case completeness of the Helsinki and Navarre (Spain) Trauma Registry, respectively [37, 38]. Registration of initial observations of the injured patients must be further improved in order to increase data quality and reliability of the results.
A second limitation is the update of the injury severity scoring tool, the AIS, from the 1998 to the 2005 version, which took place in 2015. According to Hsu et al. [39], the adaptation of the AIS-2005 version resulted in a significant reduction of severity of injury scores in the measurement of the same injuries. Since the aim of this study was to observe recent trends in the epidemiology of pediatric trauma, we included the years 2015–2018, for which the AIS-2005 version applied. By splitting the study period in two (2009–2014 and 2015–2018), we were able to present injury severity scores adapted to the AIS-2005 version separated from each other, in an attempt to minimize misleading outcomes of injury severity. Nonetheless, the results concerning injury severity should be interpreted with caution.
Conclusions
Domestic accidents are a significant cause of injury, especially in younger children, and RTAs are the lead cause of fatal injury. Severe pediatric trauma in the Netherlands is predominantly managed in trauma centers, where a multidisciplinary team of experts is available. Improving the numbers of severely injured patients primarily brought to level-1 trauma centers may help further reduce mortality. Also, injury prevention programs should be directed toward increasing safety measures in traffic.
References
Statistics Netherlands: Causes of death by age and gender in 2020 (2020) Available from: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/7052_95/table?fromstatweb. Accessed 19 Jan 2022
Van der Sluis CK, Kingma J, Eisma WH et al (1997) Pediatric polytrauma: short-term and long-term outcomes. J Trauma 43(3):501–506
Janssens L, Gorter JW, Ketelaar M et al (2009) Long-term health condition in major pediatric trauma: a pilot study. J Pediatr Surg 44:1591–1600
Janssens L, Holtslaq HR, van Beeck EF et al (2012) The effects of regionalization of pediatric trauma care in the Netherlands: a surveillance based before-after study. J Trauma Acute Care Surg 73:1284–1287
Stam C, Blatter B (2019) Injuries 2018: Key figures Injury information system. Veiligheid NL, Report No.:795, Project No.: 20.0012, p 91
Kissoon N, Dreyer J, Walia M (1990) Pediatric trauma: differences in pathophysiology, injury patterns and treatment compared with adult trauma. CMAJ 142(1):27–34
Hamill J, Beasley SW (2006) Training in pediatric trauma: the problem of safer societies. ANZ J Surg 76(7):596–599
National Network Acute Care 2015 Available from: http://www.lnaz.nl. Accessed 12 Jan 2022
Copes WS, Champion HR, Sacco WJ et al (1988) The injury severity score revisited. J Trauma 28(1):69–77
Dr. Pediatric Education Online, Peds Cases: Pediatric Vital Signs Reference Chart 2020 Available from: http://www.pedscases.com/pediatric-vital-signs-reference-chart. Assessed 02 Jan 2022
Driessen MLS, Sturms LM, Bloemers FW et al (2020) The Dutch nationwide trauma registry: the value of capturing all acute trauma admissions. Injury 51(11):2553–2559
Eilering M, Stam C (2017) Injuries in children and young adults 0–18 years old in 2015: injury figures. Veiligheid NL, Report No.: 674, Project No.: 20.0012, p 47
Sleet DA (2018) The global challenge of child injury prevention. Int J Environ Res Public Health 15(9):1921
Morrongiello BA, Ondejko L, Littlejohn A (2004) Understanding toddlers’ in-home injuries: II. Examining parental strategies, and their efficacy, for managing child injury risk. J Pediatr Psychol 29:433–446
Jullien S (2021) Prevention of unintentional injuries in children under five years. BMC Pediatr 21(Suppl 1):311
Kendrick D, Elkan R, Hewitt M et al (2000) Does home visiting improve parenting and the quality of the home environment? A systematic review and meta-analysis. Arch Dis Child 82(6):443–451
Consumer and Safety Institute VeiligheidNL: Safety in and around the house, Available from: https://www.veiligheid.nl/kinderveiligheid/veilig-thuis/hulpmiddelen/huiskamer. Accessed 25 March 2022
Institute for Road Safety Research (SWOV) (2019) Children aged 0–14 years. SWOV Fact sheet, July 2019, The Hague, Available from: https://www.swov.nl/en/facts-figures/factsheet/children-aged-0-14
Institute for Road Safety Research (SWOV) (2017) Moped and light-moped riders. SWOV Fact sheet, October 2017. SWOV, The Hague, Available from: https://www.swov.nl/en/facts-figures/factsheet/moped-and-light-moped-riders
Aarts L, Eenink R, Weijermars W (2014) Shifting up to more road-safety: Towards maximum road safety for and by everyone. Institute for Road Safety Research (SWOV), Report No.:2014–37, Available from: https://www.swov.nl/publicatie/opschakelen-naar-meer-verkeersveiligheid-0
Weijermars WAM, Boele-Vos MJ, Stipdonk HL et al (2019) Potential casualty reduction by use of bicycle helmets. Institute for Road Safety Research (SWOV), Report No.:2019–2. Available from: https://www.swov.nl/publicatie/mogelijke-slachtofferreductie-door-de-fietshelm
Hietbrink F, Houwert RM, van Wessem KJP et al (2020) The evolution of trauma care in the Netherlands over 20 years. Eur J Trauma Emerg Surg 46:329–335
Escobar MA Jr, Morris CJ (2016) Using a multidisciplinary and evidence-based approach to decrease undertriage and overtriage of pediatric trauma patients. J Pediatr Surg 51(9):1518–1525
Nakamura Y, Daya M, Bulger EM et al (2012) Evaluating age in the field triage of injured persons. Ann Emerg Med 60(3):335–345
Peng J, Wheeler K, Groner JI et al (2017) Undertriage of pediatric major trauma patients in the United States. Clin Pediatr 56(9):845–853
Van der Sluijs R, Lokerman RD, Waalwijk JF et al (2020) Pre-hospital trauma triage research collaborative (PTTRC). Accuracy of pre-hospital trauma triage and field triage decision rules in children (P2–T2 study): an observational study. Lancet Child Adolesc Health 4(4):290–298
Van der Sluijs R, van Rein EAJ, Wijnand JGJ et al (2018) Accuracy of pediatric trauma field triage: a systematic review. JAMA Surg 153(7):671–676
Navascués JA, Matute J, Soleto J et al (2005) Pediatric trauma in Spain: a report from the HUGM trauma registry. Eur J Pediatr Surg 15(1):30–37
Nesje E, Valøy NN, Krüger AJ et al (2019) Epidemiology of pediatric trauma in Norway: a single trauma center observational study. Int J Emerg Med 12(1):18
Bayreuther J, Wagener S, Woodford M et al (2009) Paediatric trauma: injury pattern and mortality in the UK. Arch Dis Child Educ Pract Ed 94:37–41
Do HQ, Steinmetz J, Rasmussen LS (2012) In-hospital mortality pattern of severely injured children. Injury 43(12):2060–2064
Schoeneberg C, Schilling M, Keitel J et al (2014) Mortality in severely injured children: experiences of a German level 1 trauma center (2002–2011). BMC Pediatr 14:194
Avraham JB, Bhandari M, Frangos SG et al (2019) Epidemiology of paediatric trauma presenting to US emergency departments: 2006–2012. Inj Prev 25(2):136–143
Oliver J, Avraham J, Frangos S et al (2018) The epidemiology of inpatient pediatric trauma in United States hospitals 2000 to 2011. J Pediatr Surg 53(4):758–764
Svantner J, Dolci M, Heim C et al (2021) Pediatric trauma: six years of experience in a Swiss trauma center. Pediatr Emerg Care 37(12):e1133–e1138
El Mestoui Z, Jalalzadeh H, Giannakopoulos GF et al (2017) Incidence and etiology of mortality in polytrauma patients in a Dutch level I trauma center. Eur J Emerg Med 24(1):49–54
Ali Ali B, Fortun M, Belzunegui T (2016) Missing variables in major trauma registry of Navarre. J Intensive Crit Care 2:2
Heinänen M, Brinck T, Lefering R et al (2021) How to validate data quality in a trauma registry? The Helsinki trauma registry internal audit. Scand J Surg 110(2):199–207
Hsu SY, Wu SC, Rau CS et al (2019) Impact of adapting the abbreviated injury scale (AIS)-2005 from AIS-1998 on injury severity scores and clinical outcome. Int J Environ Res Public Health 16(24):5033
Acknowledgments
The authors would like to thank the data managers and coordinators of the 11 Dutch trauma centers for the data acquisition and their permission to use these data for national analysis (Amsterdam University Medical Center, locations AMC and VUMC, Amsterdam; Medical Spectrum Twente, Enschede; University Medical Center Groningen, Groningen; Leiden University Medical Center, Leiden; Maastricht University Medical Center, Maastricht; Radboud University Medical Center, Nijmegen; Erasmus Medical Center, Rotterdam; Elisabeth Two Cities Hospital, Tilburg; University Medical Center Utrecht, Utrecht; and Isala Hospitals, Zwolle).
Funding
No grants were received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
Informed consent and approval of an institutional or national review board were not obtained since the authors received only summarized data from the national trauma registry.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fylli, C., Schipper, I.B. & Krijnen, P. Pediatric Trauma in The Netherlands: Incidence, Mechanism of Injury and In-Hospital Mortality. World J Surg 47, 1116–1128 (2023). https://doi.org/10.1007/s00268-022-06852-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06852-y