Abstract
Background
In search of an ideal cosmesis, transoral endoscopic thyroidectomy via vestibular approach (TOETVA) has recently been introduced to avoid a visible scar. Although ambulatory thyroid surgery is considered safe in carefully selected patients, this remains unclear for TOETVA.
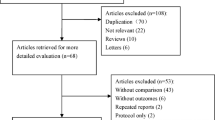
Methods
All consecutive adult patients who underwent ambulatory TOETVA or open thyroid surgery at a French university hospital were prospectively enrolled from 12/2020 until 11/2021. The primary outcome was postoperative morbidity (recurrent laryngeal nerve (RLN) palsy, re-intervention for bleeding, wound morbidity, or hospital readmission). The secondary outcome was quality of life (QoL), measured by a survey including a validated questionnaire (SF-12) and a modified thyroid surgery questionnaire six weeks after surgery.
Results
Throughout the study period, 374 patients underwent a unilateral lobectomy or isthmectomy in ambulatory setting, of which 34 (9%) as TOETVA (including 21 (62%) for a possible malignancy). In the TOETVA group, younger age (median 40 (IQR 35–50) vs. 51 (40–60) years, P < 0.001) and lower BMI (median 23.1 (20.9–25.4) vs. 24.9 (22.1–28.9) kg/m2, P = 0.001) were noted. No cases were converted to open cervicotomy. TOETVA was at least as good as open cervicotomy with nil versus four (1%) re-interventions for bleeding, one temporary (5%) versus 13 (4%) (temporary) RLN palsies, and one (<1%) wound infection (open cervicotomy group). No hospital readmissions occurred in all ambulatory surgery patients. No differences were found in physical (P = 0.280) and mental (P = 0.569) QoL between TOETVA and open surgery.
Conclusions
In carefully selected patients, the feasibility and safety of ambulatory TOETVA are comparable to open surgery.
Similar content being viewed by others
Introduction
In search of an ideal cosmetic result, transoral endoscopic thyroidectomy via vestibular approach (TOETVA) has recently been introduced to avoid a visible scar[1]. This new surgical technique has proven to be as feasible and safe as an open thyroidectomy for selected patients with benign thyroid nodules and differentiated thyroid cancers [2, 3]. More than half of all patients undergoing thyroid surgery may be eligible for TOETVA [4].
The increased costs and spending in the treatment of thyroid nodules have placed additional pressure on health care systems [5]. Moreover, the ongoing COVID-19 pandemic has forced surgeons and hospitals to restructure care for the sake of bed capacity, often leading to an increased number of outpatient surgical procedures [6].
The initial reluctant attitude toward ambulatory endocrine neck surgery was linked to the fear of an out-of-hospital compressive hematoma [7]. Indeed, careful patient selection is paramount when performing ambulatory thyroid surgery [8]. Several international studies have been able to identify risk factors for postoperative bleeding, facilitating patient selection [8,9,10]. Implementing TOETVA in ambulatory setting and evaluating its safety and feasibility, including patient satisfaction and quality of life (QoL), has not yet been published.
This study aims to compare the feasibility, safety, and short-term QoL of TOETVA and open surgery via cervicotomy in ambulatory setting in a tertiary referral university hospital with extensive experience in ambulatory thyroid surgery.
Material and methods
Study cohort
All consecutive adult patients who underwent a hemithyroidectomy or isthmectomy via cervicotomy or a TOETVA procedure at a tertiary referral university hospital in France were enrolled from December 2020 until November 2021. All patients provided written informed consent. No total thyroidectomies were performed in ambulatory setting. A prospectively maintained database combining data from EUROCRINE® and a coded Excel® file contains all endocrine surgical procedures. The department is a high-volume center specialized in endocrine surgery, with around 1400 thyroid surgical procedures every year, of which 374 (27%) isthmectomies and unilateral lobectomies are performed in ambulatory setting. At the hospital site, a pavilion exclusively dedicated to ambulatory surgery is used. Patients are selected for ambulatory surgery according to predefined criteria that were previously published [8]. Proper patient selection requires clinical assessment of social, patient-specific factors including the presence of adequate family or friend support and the ability to follow postoperative instructions. A thyroidectomy by TOETVA is only performed at patients’ request (in those wishing to avoid a cervical scar) and in thyroid pathology with the following characteristics: a thyroid <45 ml and/or with a nodule <50 mm in case of Bethesda <4 cytology, or <20 mm in case of Bethesda ≥5, without lateral lymph node spread nor mediastinal extension [11]. Dental hygiene should be satisfactory, and the patients should be able to conduct the required perioperative oral care [12]. Specific contra-indications for a TOETVA were previously described by others and applied in our center: previous neck surgery, cancer >2 cm, benign nodules >5 cm, substernal goiter, previous neck radiation, oral abscesses, and lymph node involvement on neck ultrasound [4, 13, 14]. All TOETVA procedures were performed at the patients’ request for esthetic reasons to avoid a visible scar.
Patient characteristics
Patient demographics (age at surgery, sex, length, weight, body mass index (BMI), family history of thyroid cancer, and family history of other cancers) were collected. Patient comorbidity was evaluated by the American Society of Anesthesiology (ASA, categorized as I [healthy], II [mild systemic disease], and III–IV [severe systemic disease]) score and the New York heart association (NYHA) classification of heart failure [15]. The main indication for surgery, preoperative thyroid-stimulating hormone (TSH, reference value 0.45–4.50 mIU/L), and the presence of hypo- or hyperthyroidism, arterial hypertension, hypercholesterolemia, and diabetes were collected.
Preoperative investigations
All patients underwent a preoperative neck ultrasound evaluating thyroid nodularity, lymph nodes, and thyroid nodule size and appearance (classified by the EU-TIRADS score [16]). Ultrasound-guided fine-needle aspiration was performed and classified according to the 2017 Bethesda scoring system [17] in patients with suspicious nodules on neck ultrasound. Antibiotics were started perioperatively and continued for five days. Amoxicillin (3 g/day) with clavulanic acid (187 mg/day) are the treatment of choice (for clean/contaminated surgery) [2, 18]. Chlorhexidine mouthwash three times a day was started the day before surgery and continued for at least five days [2, 18].
Surgical technique
The TOETVA procedure was introduced in our center in February 2020, based on the technique first described by Anuwong[1]. After an initial experience with 21 uneventful inpatient cases, the technique was first performed in ambulatory setting in December 2020. The procedure is performed under general anesthesia with an endotracheal tube. One 10 mm port (midline), two 5 mm ports (left and right), and a 30 degrees angled scope are used. An endoscopic bipolar forceps and a Ligasure™ (Medtronic, Jacksonville, Florida) endoscopic vessel sealer are used for dissection and hemostasis. Intermittent intra-operative nerve monitoring (IONM) is performed via one of the 5 mm ports (NIM-Response/Medtronic, Jacksonville, Florida).
Surgical characteristics
Time from referral to surgery (in days), date and duration of surgery, surgical procedure (isthmectomy or hemithyroidectomy with or without prophylactic unilateral central lymph node dissection), identification of the RLN, number of RLNs at risk, parathyroid gland identification and re-implantation, use of IONM, and change of surgical strategy were recorded.
Pathology and clinical/surgical outcome data
Pathology reports included the main and secondary histological diagnosis, multifocality, largest tumor size, presence of parathyroid glands, the weight of the resected specimen, and 8th edition of the American joint committee on cancer/union for international cancer control (AJCC/UICC) TNM staging system. Surgical and clinical outcome data included length of hospital stay, time until first surgical follow-up, RLN palsy (temporary/permanent), laryngoscopy results, hypoparathyroidism (temporary/permanent), oral calcium and/or vitamin D supplementation, re-intervention for bleeding, thyroid function six weeks after surgery, and wound infection. All procedures were performed under general anesthesia. No additional local anesthesia was administered. Post-operative laryngoscopy was performed selectively (on clinical grounds). The postoperative pain protocol did not differ from the protocol for a traditional cervicotomy[19].
Study outcome
All patients were phoned the day after surgery by a member of our dedicated nurses’ team to check on their well-being. All patients were seen in person six weeks after surgery. The primary outcome was the presence of postoperative morbidity (recurrent laryngeal nerve palsy, re-intervention for bleeding, wound morbidity, or hospital readmission). The secondary outcome was QoL, measured by a modified online survey (Google Forms®) including a validated questionnaire (SF-12) [20] and a self-developed thyroid surgery questionnaire six weeks after surgery. The SF-12 questionnaire is available in French and has been validated as a practical alternative to the SF-36 in France [21]. The authors selected 13 additional questions, related to morbidity after neck surgery (Supplementary Table 1). All questions could only be answered with: not at all (1), a little (2), some (3), quite a bit (4), and very much/completely (5).
Statistics
Continuous variables are reported as medians and interquartile ranges (IQR), and nominal variables as counts and percentages. Descriptive statistics were used to compare differences between patients that underwent TOETVA and open surgery in ambulatory setting, using the Chi-square test and the Mann–Whitney U test, as appropriate. The SF-12 QoL questionnaire translates into a physical and mental score for comparison. The additional 13 thyroid surgery specific questions (range 1–5) translated into a mean value and were compared using the Mann–Whitney U test. P-values < 0.05 indicate statistically significant differences. All statistical analyses were conducted using STATA® (StataCorp, V.16·1/MP).
Results
Throughout the study period, 374 adult patients underwent a lobectomy (94%, n = 353) or isthmectomy (6%, n = 21) in ambulatory setting of which 34 (9%) via TOETVA and 340 (91%) via cervicotomy. All 13 patients that underwent an isthmectomy would have had an isthmectomy in case of a cervicotomy.
Demographic and preoperative data for both study groups are presented in Table 1. The overall median age at surgery was 49 (39–59) years, with a significantly younger TOETVA group (40 (35–50) years). The overall female-to-male ratio was 3.61 with no male patients in the TOETVA group. The median BMI was 24.8 (22.0–28.7) kg/m2, with a significantly slimmer TOETVA group (23.1 (20.9–25.4) kg/m2). Twelve patients (3%) reported a positive family history of thyroid cancer. The overall cohort was healthy, with 60% ASA score I, 84% NYHA score I, and low numbers of hyperthyroidism, arterial hypertension, hypercholesterolemia, and diabetes. The TOEVA group showed significantly better ASA scores (P = 0.023).
The main indication for surgery was excluding a thyroid malignancy (59%, n = 222), confirmed by EU-TIRADS IV or higher scores in 229 patients (61%) and Bethesda 3 or higher scores in 223 patients (60%). No significant differences were found between both groups. The median maximum thyroid nodule size was 33 (17–43) mm, with a significantly smaller maximum nodule size in the TOETVA group (24 (18–33) mm).
Intra-operative characteristics
After a median waiting period of 55 (38–75) days between surgical referral and date of surgery, 158 (42%) patients underwent a left hemithyroidectomy, 195 (52%) patients underwent a right hemithyroidectomy, and 21 (6%) an isthmectomy. Intra- and postoperative data for both study groups are presented in Table 2. Significantly more TOETVA patients underwent an isthmectomy (38% vs. 2%). No TOETVA cases were converted to an open approach. Median operative time was 49 (40–60) min, with significantly longer operative times in the TOETVA group (79 (60–90) min). Intermittent IONM was used in all TOETVA cases involving a hemithyroidectomy (62%, n = 21), but only in selected cases for the cervicotomy group (5%, n = 16). No returns to theatre for a compressive hematoma occurred in the TOETVA group compared to four (1%) in the cervicotomy group. None of these occurred outside the mandatory surveillance period of six hours before discharge.
Postoperative outcomes
Surgical morbidity is presented in Table 2. No hospital readmissions occurred. After a median surgical follow-up of 44 (34–45) days, few major complications were noted. One temporary vocal cord palsy (5%) was suspected by postoperative hoarseness and confirmed by flexible nasal laryngoscopy in the TOETVA group. The vocal cord function recovered within six weeks after surgery. Thirteen (4%) vocal cord palsies were confirmed by flexible nasal laryngoscopy in the cervicotomy group. No mental nerve injuries or perioperative skin punctures were recorded in the TOETVA group. One patient developed a wound infection (<1%) in the cervicotomy group one month after surgery, treated with oral antibiotics. A minority of cases became hypothyroid without treatment (15%, n = 47). Median TSH at six weeks after surgery was 2.46 (1.79–3.66) mIU/L. No significant difference was found between both study groups. However, no patients in the TOETVA group required thyroid hormone replacement compared to 47 (14%) patients in the open surgery group.
Pathology
The results of the final pathology reports are presented in Table 3. The median weight of the resected specimen was 16 (8–29) g, with significantly lighter specimens in the TOETVA group (7 (4–12) g). Some 133 patients (36%) received a diagnosis of thyroid cancer on final histopathology. The median tumor size was 12 (7–30) mm.
Quality of life
Some 168 (45%) patients completed the QOL questionnaire six weeks after surgery (Table 4). No significant differences were found in overall physical (P = 0.280) and mental (P = 0.569) scoring of quality of life between both study groups (SF-12). The thyroid surgery specific QOL questions revealed significantly more neck discomfort (P = 0.015), loss of sensation (P = 0.001), and neck movement difficulties (P = 0.032) in the TOETVA group. Twelve patients (55%) experienced at least moderate neck discomfort and 13 (59%) at least moderate loss of sensation in the TOETVA group compared to 30 (21%) and 19 (13%) in the cervicotomy group, respectively. More itching of the scar (20% vs. 5% at least moderate, P < 0.001) and fashion changes (22% vs. 9% at least moderate, P = 0.001) were noted in the open surgery group. No differences were found in the overall influence of the surgery on quality of life (at least moderate in 18% of the TOETVA group vs. 16% of the cervicotomy group, P = 0.509).
Discussion
This retrospective analysis of a prospective cohort compared the feasibility, safety, and QoL of TOETVA and open surgery in ambulatory setting. Of the 374 patients that underwent a hemithyroidectomy or isthmectomy, 34 (9%) underwent a TOETVA. Patients selected for TOETVA were younger, healthier, and presented with smaller nodules. In the TOETVA group, no major complications occurred, and all ambulatory patients were discharged as planned. No hospital readmissions were noted in the overall cohort. No differences were found in short-term physical and mental scores of QoL between TOETVA and open surgery. More neck discomfort and loss of sensation were noted in the TOETVA group, but no differences were found in the overall influence of the surgery on quality of life.
This is the first study to evaluate and compare morbidity and QoL of TOETVA and open surgery in ambulatory setting. The inclusion of all consecutive patients reduces the risk of selection bias. The extensive experience of the department with ambulatory thyroid surgery, the standardized work-up and surgical approach, and the completeness of the dataset strengthen the analysis and results.
To our knowledge, no thyroid surgery specific questionnaire exists. The validated ThyPRO questionnaire [22] is useful to evaluate QoL in patients with thyroid disease but is time-consuming, extensive, and not specifically developed for a surgical population with specific surgery-related morbidity. Our QoL analysis was restricted to one moment in time (six weeks after surgery) and therefore only reflects short-term outcomes. No baseline comparison for QoL was available and possible differences between both study groups before surgery could not be adjusted for. However, no significant difference was found in the overall negative impact on QoL between both groups. Validation of our short-term results and analyzing long-term results are required. The results presented in our series must be interpreted with caution as all TOETVA patients were female. Moreover, TOETVA patients were strictly selected and only treated by TOETVA at patient’s request.
An extensive experience with ambulatory thyroid surgery and overcoming the initial experience with TOETVA are required to perform this new technique safely. Starting an ambulatory thyroidectomy program for TOETVA should be progressive, cautious, and validated by the surgeons, anesthesiologists, and nursing staff. Also, patient selection is paramount in ambulatory surgery. Specific selection criteria are available considering clinical, social, and procedural factors [23]. In our series, younger patients with lower BMI and smaller nodules underwent a TOETVA. However, patients were only selected for TOETVA at the patients’ request to avoid a visible scar. A simple and reproducible predictive score of early discharge for lobectomy was followed [8]. All neck hematomas occurred after open cervicotomy but developed within the mandatory six hours of surveillance. No hospital readmissions occurred in both study groups. A recent narrative scoping review on outpatient thyroidectomy highlighted the safety, high patient satisfaction, and decreased health costs of same-day discharge [24].
The main advantage of TOETVA is avoiding a visible scar. Nevertheless, in our series, patients undergoing TOETVA experienced more neck discomfort, loss of sensation, and neck movement difficulties in the first weeks following surgery compared to open cervicotomy. Firstly, the operative time is longer, which means patients tend to be in hyperextension for a larger amount of time. Secondly, in our series, all patients with open surgery received an injection of local anesthetics which was not performed in the TOETVA group. Indeed, multimodal regimens have been shown to decrease pain after thyroid surgery [19]. Thirdly, the swelling related to the hydro dissection and blunt dissection might cause more trauma to the surrounding tissues. This information is important to include in the informed consent. The altered sensation after TOETVA was recently evaluated with transient impairment, especially at the chin [25]. Very few studies have commented on pain after TOETVA. One recent analysis found TOETVA to be associated with reduced neck, cervical back, and swallowing VAS scores and higher jaw, brushing teeth, lower lip, and chin pain [26]. In addition, one other group found different pain control experiences with similar or more analgesics needed for adequate pain control perioperatively [27]. Recently, postoperative pain management with administration of oral acetaminophen (650 mg) supplemented with intramuscular ketorolac tromethamine injection (30 mg) if needed was proposed to reduce pain after TOETVA [28]. More research regarding short-term and long-term postoperative pain assessment and management is needed. Specifically, the influence of local or locoregional anesthetics and different perioperative pain regimens in patients with TOETVA needs to be evaluated.
Conclusion
In carefully selected patients, performing TOETVA in ambulatory setting is safe and feasible with morbidity and quality of life comparable to open surgery.
References
Anuwong A (2016) Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg 40:491–497
Anuwong A, Ketwong K, Jitpratoom P et al (2018) Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg 153:21–27
Wang Y, Zhou S, Liu X et al (2021) Transoral endoscopic thyroidectomy vestibular approach vs conventional open thyroidectomy: meta-analysis. Head Neck 43:345–353
Grogan RH, Suh I, Chomsky-Higgins K et al (2019) Patient eligibility for transoral endocrine surgery procedures in the United States. JAMA Netw Open 2:e194829
Van Den Heede K, Tolley NS, Di Marco AN et al (2021) Differentiated thyroid cancer: a health economic review. Cancers (Basel) 13:2253
Weissman GE, Crane-Droesch A, Chivers C et al (2020) Locally informed simulation to predict hospital capacity needs during the COVID-19 pandemic. Ann Intern Med 173:21–28
Doran HE, England J, Palazzo F et al (2012) Questionable safety of thyroid surgery with same day discharge. Ann R Coll Surg Engl 94:543–547
Chereau N, Godiris-Petit G, Noullet S et al (2021) Risk score of neck hematoma: how to select patients for ambulatory thyroid surgery? World J Surg 45:515–521
Doran HE, Wiseman SM, Palazzo FF et al (2021) Post-thyroidectomy bleeding: analysis of risk factors from a national registry. Br J Surg 108:851–857
Salem FA, Bergenfelz A, Nordenstrom E et al (2019) Evaluating risk factors for re-exploration due to postoperative neck hematoma after thyroid surgery: a nested case-control study. Langenbecks Arch Surg 404:815–823
Zhang D, Park D, Sun H et al (2019) Indications, benefits and risks of transoral thyroidectomy. Best Pract Res Clin Endocrinol Metab 33:101280
Dionigi G, Chai YJ, Tufano RP et al (2018) Transoral endoscopic thyroidectomy via a vestibular approach: why and how? Endocrine 59:275–279
Anuwong A, Sasanakietkul T, Jitpratoom P et al (2018) Transoral endoscopic thyroidectomy vestibular approach (TOETVA): indications, techniques and results. Surg Endosc 32:456–465
Dionigi G, Lavazza M, Bacuzzi A et al (2017) Transoral endoscopic thyroidectomy vestibular approach (TOETVA): from A to Z. Surg Technol Int 30:103–112
Caraballo C, Desai NR, Mulder H et al (2019) Clinical implications of the New York heart association classification. J Am Heart Assoc 8:e014240
Russ G, Bonnema SJ, Erdogan MF et al (2017) European thyroid association guidelines for ultrasound malignancy risk stratification of thyroid nodules in adults: the EU-TIRADS. Eur Thyroid J 6:225–237
Cibas ES, Ali SZ (2017) The 2017 Bethesda system for reporting thyroid cytopathology. Thyroid 27:1341–1346
Deroide G, Honigman I, Berthe A et al (2021) Trans oral endoscopic thyroidectomy (TOETVA): first French experience in 90 patients. J Visc Surg 158:103–110
Uhlmann RA, ReinhartPostevka HAE et al (2019) A review of postoperative pain management for thyroid and parathyroid surgery. J Surg Res 241:107–111
Ware J Jr, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Gandek B, Ware JE, Aaronson NK et al (1998) Cross-validation of item selection and scoring for the SF-12 health survey in nine countries: results from the IQOLA project. International quality of life assessment. J Clin Epidemiol 51:1171–1178
Watt T, Bjorner JB, Groenvold M et al (2015) Development of a short version of the thyroid-related patient-reported outcome ThyPRO. Thyroid 25:1069–1079
Terris DJ, Snyder S, Carneiro-Pla D et al (2013) American thyroid association statement on outpatient thyroidectomy. Thyroid 23:1193–1202
Philteos J, Baran E, Noel CW et al (2021) Feasibility and safety of outpatient thyroidectomy: a narrative scoping review. Front Endocrinol (Lausanne) 12:717427
Liang TJ, Wang KC, Liu SI et al (2022) Multimodal assessments of altered sensation after transoral endoscopic thyroidectomy. World J Surg 46:600–609
Zhang D, Caruso E, Sun H et al (2019) Classifying pain in transoral endoscopic thyroidectomy. J Endocrinol Invest 42:1345–1351
Lan KM, Chen CM, Chuang CC et al (2017) Less postoperative pain in patients receiving trans-oral vestibular endoscopic thyroidectomy: a plausible finding? Gland Surg 6:420–421
You JY, Kim H, Park DW et al (2021) Prevention of transoral thyroidectomy complications: an analysis of surgical outcomes in 423 consecutive series. Surgery 170:1155–1159
Acknowledgements
Drs Van Den Heede and Chereau had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. We would like to thank Dr. Walid Hadji for his additional help with the data collection.
Author information
Authors and Affiliations
Contributions
KVDH, NC, FM: study concept and design; KVDH, NC, FM: acquisition, analysis, or interpretation of data; KVDH: drafting of the manuscript; All authors: critical revision of the manuscript for important intellectual content; KVDH, NB: statistical analysis; All authors: administrative, technical, or material support; KVDH, NC, FM: supervision.
Corresponding author
Ethics declarations
Conflict of interest
None reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Van Den Heede, K., Brusselaers, N., Gaujoux, S. et al. Feasibility and Safety of Ambulatory Transoral Endoscopic Thyroidectomy via Vestibular Approach (TOETVA). World J Surg 46, 2678–2686 (2022). https://doi.org/10.1007/s00268-022-06666-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06666-y