Abstract
Background
Inadvertent injury of the recurrent laryngeal nerve can occur during radiofrequency ablation (RFA) of thyroid nodules. Methods to avoid permanent injury have not been described. Laryngeal ultrasonography (LUSG) can assess the function of vocal cords (VCs) in real time. The present study aimed to evaluate the feasibility and accuracy of LUSG in assessing real-time VC function during RFA of benign thyroid nodules.
Methods
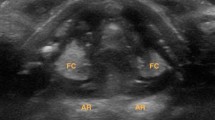
Consecutive patients undergoing RFA for benign thyroid nodules under local anesthesia were included. Spontaneous VC movements were checked with intra-operative LUSG (iLUSG) following each transverse ablation plane. In case of reduced VC movement, the ablation was stopped immediately. Post-ablation VC function was rechecked by LUSG on day-0 and flexible laryngoscopy (FL) on day-7. A concordance with day-0 LUSG or day-7 FL was a “true positive” or “true negative” depending on the presence or absence of VC palsy (VCP). Accuracy was calculated as the sum of all true positives and negatives divided by total nerves-at-risk.
Results
Of 65 eligible patients, 56 (86.2%) were females. Twelve (18.5%) patients had bilateral lobe RFA, while 53 (81.5%) had unilateral RFA. The total number of nerves-at-risk was 77. Three unilateral VCPs (3.9%) were initially detected on iLUSG and confirmed by day-0 LUSG. All recovered fully within one week. The overall accuracy of iLUSG was 100%.
Conclusion
iLUSG is a highly accurate method that permits real-time feedback on the function of the VCs during RFA procedure. Real-time detection of VCP may prevent permanent injury. Methodological routine use of iLUSG is recommended during thyroid RFA.
Similar content being viewed by others
Data availability
Datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Kim J-H, Baek JH, Lim HK et al (2018) 2017 Thyroid Radiofrequency ablation guideline: korean society of thyroid radiology. Korean J Radiol 19:632–655. https://doi.org/10.3348/kjr.2018.19.4.632
Kuo JH, Lee JA (2021) The adoption of ultrasound-guided radiofrequency ablation of thyroid nodules in the United States. Ann Surg 273:e10–e12. https://doi.org/10.1097/SLA.0000000000003930
National institute for health and care excellence (2016) Ultrasound-guided percutaneous radiofrequency ablation for benign thyroid nodules. In: Natl Inst Heal Care Excell Interv Proced Guid https://www.nice.org.uk/guidance/ipg562
Papini E, Pacella CM, Solbiati LA et al (2019) Minimally-invasive treatments for benign thyroid nodules: a delphi-based consensus statement from the Italian minimally-invasive treatments of the thyroid (MITT) group. Int J Hyperth Off J Eur Soc Hyperthermic Oncol North Am Hyperth Gr 36:376–382. https://doi.org/10.1080/02656736.2019.1575482
Wang J-F, Wu T, Hu K-P et al (2017) complications following radiofrequency ablation of benign thyroid nodules. Chin Med J (Engl) 130:1361–1370. https://doi.org/10.4103/0366-6999.206347
Cesareo R, Pasqualini V, Simeoni C et al (2015) Prospective study of effectiveness of ultrasound-guided radiofrequency ablation versus control group in patients affected by benign thyroid nodules. J Clin Endocrinol Metab 100:460–466. https://doi.org/10.1210/jc.2014-2186
Chung SR, Suh CH, Baek JH et al (2017) Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analysis. Int J Hyperth 33:920–930. https://doi.org/10.1080/02656736.2017.1337936
Baek JH, Lee JH, Valcavi R et al (2011) Thermal ablation for benign thyroid nodules: radiofrequency and laser. Korean J Radiol 12:525–540
Lee MK, Baek JH, Chung SR et al (2020) Effectiveness of injecting cold 5% dextrose into patients with nerve damage symptoms during thyroid radiofrequency ablation. Endocrinol Metab (Seoul, Korea) 35:407–415. https://doi.org/10.3803/EnM.2020.35.2.407
Chung SR, Baek JH, Choi YJ, Lee JH (2019) Management strategy for nerve damage during radiofrequency ablation of thyroid nodules. Int J Hyperth 36:203–209. https://doi.org/10.1080/02656736.2018.1554826
Fung MMH, Lang BHH (2021) A prospective study evaluating the feasibility and accuracy of very early postoperative translaryngeal ultrasonography in the assessment of vocal cord function after neck surgery. Surg (United States) 169:191–196. https://doi.org/10.1016/j.surg.2020.03.025
Fung MMH, Lang BH-H (2021) A prospective study comparing the midline and lateral trans-laryngeal ultrasonography approaches in vocal cord assessment before and after thyroid and neck surgeries. Am J Surg. https://doi.org/10.1016/j.amjsurg.2021.06.016
Wong KP, Lang BHH, Ng SH et al (2013) A prospective, assessor-blind evaluation of surgeon-performed transcutaneous laryngeal ultrasonography in vocal cord examination before and after thyroidectomy. Surg (United States) 154:1158–1165. https://doi.org/10.1016/j.surg.2013.04.063
Wong KP, Au KP, Lam S, Lang BHH (2017) Lessons learned after 1000 cases of transcutaneous laryngeal ultrasound (TLUSG) with laryngoscopic validation: is there a role of tlusg in patients indicated for laryngoscopic examination before thyroidectomy? in: thyroid. Mary Ann Liebert Inc 27(1): 88–94.
Wong KP, Lang BHH, Lam S et al (2016) Determining the learning curve of transcutaneous laryngeal ultrasound in vocal cord assessment by cusum analysis of eight surgical residents: when to abandon laryngoscopy. World Journal of Surgery. Springer, New York LLC, pp 659–664
Carneiro-Pla D, Miller BS, Wilhelm SM et al (2014) Feasibility of surgeon-performed transcutaneous vocal cord ultrasonography in identifying vocal cord mobility: a multi-institutional experience. Surg (United States) 156:1597–1604. https://doi.org/10.1016/j.surg.2014.08.071
De Miguel M, Peláez EM, Caubet E et al (2017) Accuracy of transcutaneous laryngeal ultrasound for detecting vocal cord paralysis in the immediate postoperative period after total thyroidectomy. Minerva Anestesiol https://doi.org/10.23736/S0375-9393.17.11755-4.
Woo J-W, Suh H, Song R-Y et al (2016) A novel lateral-approach laryngeal ultrasonography for vocal cord evaluation. Surgery 159:52–56. https://doi.org/10.1016/j.surg.2015.07.043
Woo J-W, Park I, Choe JH et al (2017) Comparison of ultrasound frequency in laryngeal ultrasound for vocal cord evaluation. Surgery 161:1108–1112. https://doi.org/10.1016/j.surg.2016.10.013
Dighe M, Barr R, Bojunga J et al (2017) Thyroid ultrasound: State of the art part 1 - Thyroid ultrasound reporting and diffuse thyroid diseases. Med Ultrason 19(1): 79–93 https://doi.org/10.11152/mu-980.
Randolph GW, Kamani D (2006) The importance of preoperative laryngoscopy in patients undergoing thyroidectomy: voice, vocal cord function, and the preoperative detection of invasive thyroid malignancy. Surgery 139:357–362. https://doi.org/10.1016/j.surg.2005.08.009
Farrag TY, Samlan RA, Lin FR, Tufano RP (2006) The utility of evaluating true vocal fold motion before thyroid surgery. Laryngoscope 116(2): 235–238 https://doi.org/10.1097/01.mlg.0000191472.02720.1f.
Wong K-P, Lang BH-H, Chang Y-K et al (2015) Assessing the validity of transcutaneous laryngeal ultrasonography (TLUSG) after thyroidectomy: what factors matter? Ann Surg Oncol 22:1774–1780. https://doi.org/10.1245/s10434-014-4162-z
Wong K-P, Woo J-W, Youn Y-K et al (2014) The importance of sonographic landmarks by transcutaneous laryngeal ultrasonography in post-thyroidectomy vocal cord assessment. Surgery 156:1590–1596. https://doi.org/10.1016/j.surg.2014.08.061
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
MMHF wrote the manuscript, researched the data and performed statistical analyses. BL critically reviewed and edited the manuscript. BL initiated and supervised the study, is the guarantor of this work, has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fung, M.M.H., Lang, B.H.H. Using Intra-Operative Laryngeal Ultrasonography as a Real-Time Tool in Assessing Vocal Cord Function During Radiofrequency Ablation of the Thyroid Gland. World J Surg 46, 2206–2211 (2022). https://doi.org/10.1007/s00268-022-06596-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06596-9