Abstract
Background
The Enhanced Recovery After Surgery (ERAS) society published new recommendations for hepatectomy in 2016. Few studies have assessed their clinical impact. The aim of this monocentric study was to assess the impact of those guidelines on outcomes after liver surgery with a special focus on cirrhotic patients.
Method
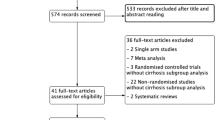
Postoperative outcomes of patients undergoing hepatectomy 30 months before and after ERAS implementation according to the 2016 ERAS guidelines were compared after inverse probability of treatment weighting (IPTW). Primary endpoint was 90-day morbidity.
Results
From 2015 to 2020, 430 patients underwent hepatectomy including 226 procedures performed before and 204 after ERAS implementation. After IPTW, overall morbidity (42.5% vs. 64.7%, p < 0.001), Comprehensive Complication Index (CCI) score (14.3 vs. 20.8, p = 0.004), length of stay (10.4 vs. 13.7 days, p = 0.001) and textbook outcome (50% vs. 40.2%, p = 0.022) were significantly improved in the ERAS group, while mortality and severe complications were similar in both groups. In the non-cirrhosis subgroup (n = 321), these results were confirmed. However, in the cirrhosis subgroup (n = 105), no difference appeared on outcomes after hepatectomy with an overall morbidity (47.5% vs. 65.2%, p = 0.069) and a length of stay (8 vs. 9 days, p = 0.310) which were not significantly different. The compliance rate to ERAS guidelines was 60% in both cirrhotic and non-cirrhotic subgroups.
Conclusion
Perioperative ERAS program for hepatectomy results in improved outcomes with decreased rate of non-severe morbidity. Although those guidelines are not deleterious for cirrhotic patients, they probably require revisions to be more effective in this patient population.


Similar content being viewed by others
References
Karanjia ND, Lordan JT, Fawcett WJ et al (2009) Survival and recurrence after neo-adjuvant chemotherapy and liver resection for colorectal metastases – A ten year study. Eur J Surg Oncol 35:838–843
Benzoni E, Molaro R, Cedolini C et al (2007) Liver resection for HCC: analysis of causes and risk factors linked to postoperative complications. Hepatogastroenterology 54:186–189
Liang X, Ying H, Wang H et al (2016) Enhanced recovery program versus traditional care in laparoscopic hepatectomy. Medicine 95:2835
Song W, Wang K, Zhang R, et al (2016) The enhanced recovery after surgery (ERAS) program in liver surgery: a meta-analysis of randomized controlled trials. SpringerPlus 5
Hashizume M, Takenaka K, Yanaga K et al (1995) Laparoscopic hepatic resection for hepatocellular carcinoma. Surg Endosc 9:1289–1291
Kasai M, Cipriani F, Gayet B et al (2018) Laparoscopic versus open major hepatectomy: a systematic review and meta-analysis of individual patient data. Surgery 163:985–995
Xiangfei M, Yinzhe X, Yingwei P et al (2019) Open versus laparoscopic hepatic resection for hepatocellular carcinoma: a systematic review and meta-analysis. Surg Endosc 33:2396–2418
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78:606–617
Labgaa I, Jarrar G, Joliat G-R et al (2016) Implementation of Enhanced Recovery (ERAS) in colorectal surgery has a positive impact on non-ERAS liver surgery patients. World J Surg 40:1082–1091
Jones C, Kelliher L, Dickinson M et al (2013) Randomized clinical trial on enhanced recovery versus standard care following open liver resection: enhanced recovery following open liver resection. Br J Surg 100:1015–1024
Melloul E, Hübner M, Scott M et al (2016) Guidelines for perioperative care for liver surgery: Enhanced Recovery After Surgery (ERAS) society recommendations. World J Surg 40:2425–2440
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Slankamenac K, Graf R, Barkun J et al (2013) The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 258:1–7
Tsilimigras DI, Mehta R, Merath K et al (2020) Hospital variation in textbook outcomes following curative-intent resection of hepatocellular carcinoma: an international multi-institutional analysis. HPB 22:1305–1313
Mullen JT, Ribero D, Reddy SK et al (2007) Hepatic insufficiency and mortality in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll Surg 204:854–862
Joliat G-R, Labgaa I, Hübner M et al (2016) Cost-benefit analysis of the implementation of an enhanced recovery program in liver surgery. World J Surg 40:2441–2450
Zheng Y, Wang L, Wu F et al (2020) Enhanced recovery after surgery strategy for cirrhosis patients undergoing hepatectomy: experience in a single research center. Ann Surg Treat Res 98:224
Ni CY, Yang Y, Chang YQ et al (2013) Fast-track surgery improves postoperative recovery in patients undergoing partial hepatectomy for primary liver cancer: A prospective randomized controlled trial. Eur J Surg Oncol (EJSO) 39:542–547
He F, Lin X, Xie F et al (2015) The effect of enhanced recovery program for patients undergoing partial laparoscopic hepatectomy of liver cancer. Clin Transl Oncol 17:694–701
Agarwal V, Divatia JV (2019) Enhanced recovery after surgery in liver resection: current concepts and controversies. Korean J Anesthesiol 72(2):119–129
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Philippe Merle has served on the advisory board of Roche, AstraZeneca, Ipsen, MSD, Eisai, Bayer, and Lilly. He has also served as a consultant for Ipsen, Eisai, and Onxeo and received grants from Ipsen and Onxeo. The other authors declare that they have no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was supported by Antonin Poncet grant from the University of LYON 1 dedicated to Paul-Noël Dumont.
Rights and permissions
About this article
Cite this article
Lunel, T., Mohkam, K., Merle, P. et al. Impact of 2016 Enhanced Recovery After Surgery (ERAS) Recommendations on Outcomes after Hepatectomy in Cirrhotic and Non-Cirrhotic Patients. World J Surg 45, 2964–2974 (2021). https://doi.org/10.1007/s00268-021-06229-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-021-06229-7