Abstract
Background
Half of the global population is at risk for catastrophic health expenditure (CHE) in the event that they require surgery. Universal health coverage fundamentally requires protection from CHE, particularly in low- and middle-income countries (LMICs). Financial risk protection reports in LMICs covering surgical care are limited. We explored the relationship between financial risk protection and hospital admission among injured patients in Cameroon to understand the role of health insurance in addressing unmet need for surgery in LMICs.
Methods
The Cameroon National Trauma Registry, a database of all injured patients presenting to the emergency departments (ED) of three Cameroonian hospitals, was retrospectively reviewed between 2015 and 2017. Multivariate regression analysis identified predictors of hospital admission after injury and of patient report of cost inhibiting their care.
Results
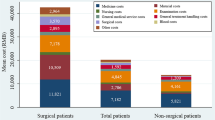
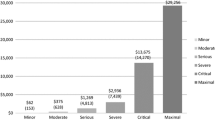
Of the 7603 injured patients, 95.7% paid out-of-pocket to finance ED care. Less than two percent (1.42%) utilized private insurance, and more than half (54.7%) reported that cost inhibited their care. In multivariate analysis, private insurance coverage was a predictor of hospital admission (OR 2.17, 95% CI: 1.26, 3.74) and decreased likelihood of cost inhibiting care (OR 0.34, 95% CI: 0.20, 0.60) when compared to individuals paying out-of-pocket.
Conclusion
The prevalence of out-of-pocket spending among injured patients in Cameroon highlights the need for financial risk protection that encompasses surgical care. Patients with private insurance were more likely to be admitted to the hospital, and less likely to report that cost inhibited care, supporting private health insurance as a potential financing strategy.
Similar content being viewed by others
References
Official Records of the UN General Assembly (2015) The 2030 Agenda for sustainable development, A/RES/70/ vol 16301(October) p 13–4
Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA et al (2015) Global Surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Lancet 386(9993):569–624
Weiser TG, Regenbogen SE, Thompson KD, Haynes AB, Lipsitz SR, Berry WR et al (2008) An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 372(9633):139–144
Debas HT, Gosselin R, McCord C, Thind A (2006) Surgery [Internet]. Disease control priorities in developing countries. The international bank for reconstruction and development/The World Bank; 2006 [cited 2019 May 29]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21250301
Alkire BC, Shrime MG, Dare AJ, Vincent JR, Meara JG, Eye M et al (2016) The global economic consequences of selected surgical disease: a modelling study. Lancet Glob Heal 3(Suppl 2):S21–S27
Grimes CE, Bowman KG, Dodgion CM, Lavy CBD (2011) Systematic Review of barriers to surgical care in low-income and middle-income countries. World J Surg. 35(5):941–950. https://doi.org/10.1007/s00268-011-1010-1
Rajaguru PP, Jusabani MA, Massawe H, Temu R, Sheth NP (2019) Understanding surgical care delivery in Sub-Saharan Africa: a cross-sectional analysis of surgical volume, operations, and financing at a tertiary referral hospital in rural Tanzania. Glob Heal Res 4(1):30
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL (2003) Household catastrophic health expenditure: a multicountry analysis. Lancet 362(9378):111–117
Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara J (2015) catastrophic expenditure to pay for surgery: a global estimate. Lancet Glob Health 3(0 2):38–44
Essue BM, Laba T-L, Knaul F, Chu A, Minh H Van, Nguyen TKP, et al. (2017) Economic burden of chronic Ill health and injuries for households in low- and middle-income countries. In: Disease control priorities, 3rd Edn :improving health and reducing poverty. The World Bank vol 9, p 121–43
Palmer N, Mueller DH, Gilson L, Mills A, Haines A (2004) Health financing to promote access in low income settings—How much do we know? Lancet 364(9442):1365–1370
Aregbeshola BS, Khan SM (2018) Out-of-pocket payments, catastrophic health expenditure and poverty among households in Nigeria 2010. Int J Heal Policy Manag 7(9):798–806
The Sustainable Development Agenda—United Nations sustainable development [Internet]. [cited 2019 Dec 2]. Available from: https://www.un.org/sustainabledevelopment/development-agenda/
Chisholm D, Kutzin J, Russell S et al (2010) Hea6/lth systems financing: the path to universal coverage. World Health Organization. https://www.who.int/whr/2010/en/. Accessed 1 Mar 2020
Saksena P, Hsu J, Evans DB (2014) Financial risk protection and universal health coverage: evidence and measurement challenges. PLoS Med. https://doi.org/10.1371/journal.pmed.1001701
Grogger J, Arnold T, León AS, Ome A (2015) Heterogeneity in the effect of public health insurance on catastrophic out-of-pocket health expenditures: the case of Mexico. Health Policy Plan 30(5):593–599
Nguyen H, Ivers R, Jan S, Pham C (2017) Analysis of out-of-pocket costs associated with hospitalised injuries in Vietnam. BMJ Glob Health. https://doi.org/10.1136/bmjgh-2016-000082
Prinja S, Jagnoor J, Chauhan AS, Aggarwal S, Nguyen H, Ivers R (2016) Article: economic burden of hospitalization due to injuries in North India: a cohort study. Int J Environ Res Public Health 13(7):673
Ekman B (2007) Catastrophic health payments and health insurance: Some counterintuitive evidence from one low-income country. Health Policy (New York) 83(2–3):304–313
Erlangga D, Suhrcke M, Ali S, Bloor K (2019) The impact of public health insurance on health care utilisation, financial protection and health status in low- And middle-income countries: A systematic review. PLoS One. Public Library of Science vol 14
Gosselin R (2009) Injuries: the neglected burden in developing countries. Bull World Health Organ 87(4):246–246
Lopez AD (2006) Disease control priorities project global burden of disease and risk factors. Oxford University Press, Oxford, p 475
Wesson HKH, Boikhutso N, Bachani AM, Hofman KJ, Hyder AA (2013) The cost of injury and trauma care in low-and middle-income countries: a review of economic evidence, health policy and planning. Oxford University Press, Oxford, pp 795–808
The World Bank (2016) Cameroon economic memorandum: markets, public administration, and growth. pp 1–51. http://documents.worldbank.org/curated/en/981281491336365033/Cameroon-economic-memorandum-markets-public-administration-and-growth. Accessed 1 Mar 2020
Ntangsi J (2012) An analysis of health sector expenditures in Cameroon using a national health accounts framework. https://cdn1.sph.harvard.edu/wp-content/uploads/sites/114/2012/10/rp141.pdf. Accessed 1 Mar 2020
(PDF) COUNTRY REPORT: The healthcare system of Cameroon: socio-economic characteristics; historical context; organizational & financial aspects; major public health programs & challenges; strength and weaknesses [Internet]. [cited 2019 Dec 3]. Available from: https://www.researchgate.net/publication/236166490_COUNTRY_REPORT_The_Healthcare_System_of_Cameroon_Socio-Economic_Characteristics_Historical_Context_organizational_Financial_Aspects_Major_Public_Health_Programs_Challenges_Strength_and_Weaknesses
Global health expenditure database [Internet]. [cited 2019 Dec 3]. Available from: https://apps.who.int/nha/database/Select/Indicators/en
Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016 | Institute for Health Metrics and Evaluation [Internet]. [cited 2019 Dec 3]. Available from: https://www.healthdata.org/research-article/global-regional-and-national-disability-adjusted-life-years-dalys-333-diseases-and
Health sector strategy 2016–2027 | MINSANTE [Internet]. [cited 2020 Mar 26]. Available from: https://www.minsante.cm/site/?q=en/content/health-sector-strategy-2016-2027-0
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L et al (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208
Petrucelli E, States JD, Hames LN (1981) The abbreviated injury scale: Evolution, usage and future adaptability. Accid Anal Prev 13(1):29–35
Eyler L, Hubbard A, Juillard C (2019) Optimization and validation of the EconomicClusters model for facilitating global health disparities research: examples from Cameroon and Ghana. PLoS One. https://doi.org/10.1371/journal.pone.0217197
Patton GC, Coffey C, Sawyer SM, Viner RM, Haller DM, Bose K et al (2009) Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 374(9693):881–892
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V et al (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet 380(9859):2095–2128
Sharma D, Prinja S, Aggarwal A, Bahuguna P, Sharma A, Rana S (2017) Out-of-pocket expenditure for hospitalization in Haryana State of India: extent, determinants & financial risk protection. Indian J Med Res 146(6):759
Pettigrew LM, Mathauer I (2016) Voluntary Health Insurance expenditure in low- and middle-income countries: exploring trends during 1995–2012 and policy implications for progress towards universal health coverage. Int J Equity Health 15(1):1–19. https://doi.org/10.1186/s12939-016-0353-5
Umeh CA, Feeley FG (2017) Inequitable access to health care by the poor in community-based health insurance programs: a review of studies from low-and middle-income countries, global health science and practice. Johns Hopkins University Press, Baltimore, pp 299–314
Allcock SH, Young EH, Sandhu MS (2019) Sociodemographic patterns of health insurance coverage in Namibia. Int J Equity Health 18(1):16. https://doi.org/10.1186/s12939-019-0915-4
Dror DM, Soriano ES, Lorenzo ME, Sarol JN, Azcuna RS, Koren R (2005) Field based evidence of enhanced healthcare utilization among persons insured by micro health insurance units in Philippines. Health Policy (New York) 73(3):263–271
Mills A, Ataguba JE, Akazili J, Borghi J, Garshong B, Makawia S et al (2012) Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet 380(9837):126–133
Nguyen H, Ivers R, Jan S, Martiniuk A, Pham C (2013) Catastrophic household costs due to injury in Vietnam. Injury 44(5):684–690
Haghparast-Bidgoli H, Saadat S, Bogg L, Yarmohammadian MH, Hasselberg M (2013) Factors affecting hospital length of stay and hospital charges associated with road traffic-related injuries in Iran. BMC Health Serv Res. https://doi.org/10.1186/1472-6963-13-281
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest related to this submission.
Ethical approval
Ethical approval was obtained from the Institutional Review Boards of UCSF, the Cameroonian National Ethics Committee, and the University of Douala.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shah, P.A., Christie, S.A., Motwani, G. et al. Financial Risk Protection and Hospital Admission for Trauma in Cameroon: An Analysis of the Cameroon National Trauma Registry. World J Surg 44, 3268–3276 (2020). https://doi.org/10.1007/s00268-020-05632-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05632-w