Abstract
Background
Anastomotic leak is one of the most serious postoperative complications, and intraoperative adequate perfusion plays a key role in preventing its development in gastric cancer surgery. This study aimed to investigate the relationships between anastomotic leak and the parameters defined by an assessment of intraoperative anastomotic perfusion using a near-infrared indocyanine green (ICG) fluorescence system and to evaluate the usefulness of this ICG fluorescence assessment in gastric cancer surgery.
Methods
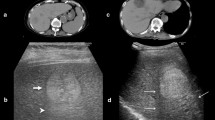
We retrospectively reviewed data of 100 patients who underwent gastric cancer surgery. In a visual assessment based on fluorescence intensity, we classified ICG fluorescence image patterns as homogeneous, heterogeneous, or faint. In a chronological assessment, the first or second time point of ICG fluorescence appearance on one or the other side of the anastomosis was defined as FT or ST, respectively. The time difference in ICG fluorescence appearance between FT and ST was defined as TD. The relationships between anastomotic leak and the evaluated clinical factors, including the parameters identified by the ICG fluorescence assessment, were evaluated using univariate or multivariate analysis.
Results
Although no signs of leak were found by surgeons’ subjective judgments, four patients developed postoperative anastomotic leak of Clavien–Dindo grade III or IV. Multivariate analysis revealed that TD was an independent predictor of anastomotic leak (odds ratio 35.361, 95% confidence interval 1.489–839.923, p = 0.027).
Conclusions
A novel parameter identified using near-infrared ICG fluorescence assessment may be useful to predict anastomotic leak in gastric cancer surgery.
Trial Registration
UMIN Clinical Trials Registry: #UMIN000030747 (https://www.umin.ac.jp/ctr/index.htm).



Similar content being viewed by others
References
Inokuchi M, Otsuki S, Fujimori Y et al (2015) Systematic review of anastomotic complications of esophagojejunostomy after laparoscopic total gastrectomy. World J Gastroenterol 21:9656–9665
Norero E, Vega EA, Diaz C et al (2017) Improvement in postoperative mortality in elective gastrectomy for gastric cancer: analysis of predictive factors in 1066 patients from a single centre. Eur J Surg Oncol 43:1330–1336
Sierzega M, Kolodziejczyk P, Kulig J et al (2010) Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg 97:1035–1042
Andreou A, Biebl M, Dadras M et al (2016) Anastomotic leak predicts diminished long-term survival after resection for gastric and esophageal cancer. Surgery 160:191–203
Li QG, Li P, Tang D et al (2013) Impact of postoperative complications on long-term survival after radical resection for gastric cancer. World J Gastroenterol 19:4060–4065
Powell A, Coxon AH, Patel N et al (2018) Prognostic significance of post-operative morbidity severity score after potentially curative D2 gastrectomy for carcinoma. J Gastrointest Surg 22:1516–1527
Selby LV, Vertosick EA, Sjoberg DD et al (2015) Morbidity after total gastrectomy: analysis of 238 patients. J Am Coll Surg 220:863–871
Martin AN, Das D, Turrentine FE et al (2016) Morbidity and mortality after gastrectomy: identification of modifiable risk factors. J Gastrointest Surg 20:1554–1564
Kingham TP, Pachter HL (2009) Colonic anastomotic leak: risk factors, diagnosis, and treatment. J Am Coll Surg 208:269–278
Kassis ES, Kosinski AS, Ross P Jr et al (2013) Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. Ann Thorac Surg 96:1919–1926
Chadi SA, Fingerhut A, Berho M et al (2016) Emerging trends in the etiology, prevention, and treatment of gastrointestinal anastomotic leakage. J Gastrointest Surg 20:2035–2051
Schaafsma BE, Mieog JS, Hutteman M et al (2011) The clinical use of indocyanine green as a near-infrared fluorescent contrast agent for image-guided oncologic surgery. J Surg Oncol 104:323–332
Zelken JA, Tufaro AP (2015) Current trends and emerging future of indocyanine green usage in surgery and oncology: an update. Ann Surg Oncol 3:S1271–S1283
van Manen L, Handgraaf HJM, Diana M et al (2018) A practical guide for the use of indocyanine green and methylene blue in fluorescence-guided abdominal surgery. J Surg Oncol 118:283–300
Jafari MD, Wexner SD, Martz JE et al (2015) Perfusion assessment in laparoscopic left-sided/anterior resection (PILLAR II): a multi-institutional study. J Am Coll Surg 220:82–92
Ris F, Liot E, Buchs NC et al (2018) Multicentre phase II trial of near-infrared imaging in elective colorectal surgery. Br J Surg 105:1359–1367
Kawada K, Hasegawa S, Wada T et al (2017) Evaluation of intestinal perfusion by ICG fluorescence imaging in laparoscopic colorectal surgery with DST anastomosis. Surg Endosc 31:1061–1069
Boni L, Fingerhut A, Marzorati A et al (2017) Indocyanine green fluorescence angiography during laparoscopic low anterior resection: results of a case-matched study. Surg Endosc 31:1836–1840
Ohi M, Toiyama Y, Mohri Y et al (2017) Prevalence of anastomotic leak and the impact of indocyanine green fluorescein imaging for evaluating blood flow in the gastric conduit following esophageal cancer surgery. Esophagus 14:351–435
Zehetner J, DeMeester SR, Alicuben ET et al (2015) Intraoperative assessment of perfusion of the gastric graft and correlation with anastomotic leaks after esophagectomy. Ann Surg 262:74–78
Kumagai Y, Hatano S, Sobajima J et al (2018) Indocyanine green fluorescence angiography of the reconstructed gastric tube during esophagectomy: efficacy of the 90-second rule. Dis Esophagus. https://doi.org/10.1093/dote/doy052
Koyanagi K, Ozawa S, Oguma J et al (2016) Blood flow speed of the gastric conduit assessed by indocyanine green fluorescence: new predictive evaluation of anastomotic leakage after esophagectomy. Medicine (Baltimore) 95:e4386
Kamiya K, Unno N, Miyazaki S et al (2015) Quantitative assessment of the free jejunal graft perfusion. J Surg Res 194:394–399
Shimada Y, Okumura T, Nagata T et al (2011) Usefulness of blood supply visualization by indocyanine green fluorescence for reconstruction during esophagectomy. Esophagus 8:259–266
Huh YJ, Lee HJ, Kim TH et al (2019) Efficacy of assessing intraoperative bowel perfusion with near-infrared camera in laparoscopic gastric cancer surgery. J Laparoendosc Adv Surg 29:476–483
Ajani JA, In H, Sano T et al (2016) Stomach. In: Amin MB (ed) AJCC cancer staging manual, 8th edn. Springer, New York, pp 203–220
Kanaya S, Gomi T, Momoi H et al (2002) Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg 195:284–287
Kang KC, Cho GS, Han SU et al (2011) Comparison of Billroth I and Billroth II reconstructions after laparoscopy-assisted distal gastrectomy: a retrospective analysis of large-scale multicenter results from Korea. Surg Endosc 25:1953–1961
Kojima K, YamadaInokuchi HM et al (2008) A comparison of Roux-en-Y and Billroth-I reconstruction after laparoscopy-assisted distal gastrectomy. Ann Surg 247:962–967
Hirahara N, Monma H, Shimojo Y et al (2011) Reconstruction of the esophagojejunostomy by double stapling method using EEA™ OrVil™ in laparoscopic total gastrectomy and proximal gastrectomy. World J Surg Oncol 9:55
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Karliczek A, Harlaar NJ, Zeebregts CJ et al (2009) Surgeons lack predictive accuracy for anastomotic leakage in gastrointestinal surgery. Int J Colorectal Dis 24:569–576
Sheridan WG, Lowndes RH, Young HL (1987) Tissue oxygen tension as a predictor of colonic anastomotic healing. Dis Colon Rectum 30:867–871
Jacobi CA, Zieren HU, Zieren J et al (1998) Is tissue oxygen tension during esophagectomy a predictor of esophagogastric anastomotic healing? J Surg Res 74:161–164
Vignali A, Gianotti L, Braga M et al (2000) Altered microperfusion at the rectal stump is predictive for rectal anastomotic leak. Dis Colon Rectum 43:76–82
Seike K, Koda K, Saito N et al (2007) Laser Doppler assessment of the influence of division at the root of the inferior mesenteric artery on anastomotic blood flow in rectosigmoid cancer surgery. Int J Colorectal Dis 22:689–697
Cooperman M, Martin EW Jr, Keith LM et al (1979) Use of Doppler ultrasound in intestinal surgery. Am J Surg 138:856–859
Ambrosetti P, Robert J, Mathey P et al (1994) Left-sided colon and colorectal anastomoses: Doppler ultrasound as an aid to assess bowel vascularization. A prospective evaluation of 200 consecutive elective cases. Int J Colorectal Dis 9:211–214
Urbanavičius L, Pattyn P, de Putte DV et al (2011) How to assess intestinal viability during surgery: a review of techniques. World J Gastrointest Surg 3:59–69
Degett TH, Andersen HS, Gögenur I (2016) Indocyanine green fluorescence angiography for intraoperative assessment of gastrointestinal anastomotic perfusion: a systematic review of clinical trials. Langenbecks Arch Surg 401:767–775
Acknowledgements
We thank Jane Charbonneau, DVM, from Edanz group (https://jp.edanzgroup.com/) for editing a draft of this manuscript.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Human and/or animal rights
This study was approved by the institutional review board of Teikyo University.
Informed consent
Informed consent was obtained from each participant included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mori, M., Shuto, K., Hirano, A. et al. A Novel Parameter Identified Using Indocyanine Green Fluorescence Angiography may Contribute to Predicting Anastomotic Leakage in Gastric Cancer Surgery. World J Surg 44, 2699–2708 (2020). https://doi.org/10.1007/s00268-020-05488-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05488-0