Abstract
Introduction
Negative pressure wound therapy (NPWT) may prevent subcutaneous fluid accumulation in a closed wound and subsequently reduce surgical site infections (SSI). This meta-analysis aimed to determine the effect of prophylactic NPWT on SSI incidence following abdominal surgery.
Methods
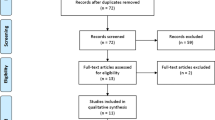
A systematic search of MEDLINE and EMBASE databases was performed using PRISMA methodology. All randomised trials reporting the use of NPWT in closed abdominal incisions were included, regardless of the type of operation. The primary outcome measure was the incidence of SSI, stratified by superficial and deep and organ/space infections. Secondary outcomes were wound dehiscence and length of hospital stay.
Results
Ten randomised trials met the inclusion criteria (five Caesarean, five midline laparotomy). The use of NPWT reduced overall SSI (11.6% vs. 16.7%, RR 0.67, 95% CI 0.48–0.95, p = 0.02). The rate of superficial SSI rate was also reduced (6.3% vs. 11.3%, RR 0.57, 95% CI 0.35–0.94, p = 0.03). There was no effect on deep or organ/space SSI (3.2% vs. 4.2%, RR 0.77, 95% CI 0.51–1.18, p = 0.23), wound dehiscence (9.7% vs. 10.9%, RR 0.92, 95% CI 0.69–1.21, p = 0.54), or length of hospital stay (MD 0.06 days, 95% CI–0.11 to 0.23, p = 0.51).
Conclusions
Prophylactic use of NPWT may reduce the incidence of superficial SSI in closed abdominal incisions but has no effect on deep or organ space SSI.



Similar content being viewed by others

References
Tanner J, Padley W, Assadian O et al (2015) Do surgical care bundles reduce the risk of surgical site infections in patients undergoing colorectal surgery? A systematic review and cohort meta-analysis of 8515 patients. Surgery 158:66–77
Venkat R, Edil BH, Schulick RD et al (2012) Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 255:1048–1059
Kobayashi M, Mohri Y, Inoue Y et al (2008) Continuous follow-up of surgical site infections for 30 days after colorectal surgery. World J Surg 32:1142–1146. https://doi.org/10.1007/s00268-008-9536-6
Badia JM, Casey AL, Petrosillo N et al (2017) Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect 96:1–15
Tevis SE, Kohlnhofer BM, Stringfield S et al (2013) Postoperative complications in patients with rectal cancer are associated with delays in chemotherapy that lead to worse disease-free and overall survival. Dis Colon Rectum 56:1339–1348
de Lissovoy G, Fraeman K, Hutchins V et al (2009) Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control 37:387–397
Keenan JE, Speicher PJ, Thacker JKM et al (2014) The preventive surgical site infection bundle in colorectal surgery: an effective approach to surgical site infection reduction and health care cost savings. JAMA Surg 149:1045–1052
Anderson DJ, Podgorny K, Berríos-Torres SI et al (2014) Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 35:605–627
Atema JJ, Gans SL, Boermeester MA (2015) Systematic review and meta-analysis of the open abdomen and temporary abdominal closure techniques in non-trauma patients. World J Surg 39:912–925. https://doi.org/10.1007/s00268-014-2883-6
Ubbink DT, Westerbos SJ, Nelson EA, Vermeulen H (2008) A systematic review of topical negative pressure therapy for acute and chronic wounds. Br J Surg 95:685–692
Suissa D, Danino A, Nikolis A (2011) Negative-pressure therapy versus standard wound care: a meta-analysis of randomized trials. Plast Reconstr Surg 128:498e–503e
Stannard JP, Volgas DA, McGwin G III et al (2012) Incisional negative pressure wound therapy after high-risk lower extremity fractures. J Orthop Trauma 26:37–42
Ingargiola MJ, Daniali LN, Lee ES (2013) Does the application of incisional negative pressure therapy to high-risk wounds prevent surgical site complications? A systematic review. Eplasty 13:e49
Scalise A, Calamita R, Tartaglione C et al (2016) Improving wound healing and preventing surgical site complications of closed surgical incisions: a possible role of incisional negative pressure wound therapy. A systematic review of the literature. Int Wound J 13:1260–1281
Javed AA, Teinor J, Wright M et al (2018) Negative pressure wound therapy for surgical-site infections: a randomized trial. Ann Surg 10:10
Suh H, Lee A-Y, Park EJ, Hong JP (2016) Negative pressure wound therapy on closed surgical wounds with dead space: animal study using a swine model. Ann Plast Surg 76:717–722
Malmsjö M, Huddleston E, Martin R (2014) Biological effects of a disposable, canisterless negative pressure wound therapy system. Eplasty 14:e15
Wilkes RP, Kilpad DV, Zhao Y et al (2012) Closed incision management with negative pressure wound therapy (CIM): biomechanics. Surg Innov 19:67–75
Kilpadi DV, Cunningham MR (2011) Evaluation of closed incision management with negative pressure wound therapy (CIM): hematoma/seroma and involvement of the lymphatic system. Wound Repair Regen 19:588–596
Allegranzi B, Zayed B, Bischoff P et al (2016) New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 16:e288–e303
Witt-Majchrzak A, Żelazny P, Snarska J (2015) Preliminary outcome of treatment of postoperative primarily closed sternotomy wounds treated using negative pressure wound therapy. Pol Przegl Chir 86:456–465
Karlakki SL, Hamad AK, Whittall C et al (2016) Incisional negative pressure wound therapy dressings (iNPWTd) in routine primary hip and knee arthroplasties: a randomised controlled trial. Bone Joint Res 5:328–337
Svensson-Björk R, Zarrouk M, Asciutto G et al (2019) Meta-analysis of negative pressure wound therapy of closed groin incisions in arterial surgery. Br J Surg 13:e20
Sahebally SM, McKevitt K, Stephens I et al (2018) Negative pressure wound therapy for closed laparotomy incisions in general and colorectal surgery: a systematic review and meta-analysis. JAMA Surg 153:e183467
Ge D (2018) The safety of negative-pressure wound therapy on surgical wounds: an updated meta-analysis of 17 randomized controlled trials. Adv Skin Wound Care 31:421–428
Hyldig N, Birke-Sorensen H, Kruse M et al (2016) Meta-analysis of negative-pressure wound therapy for closed surgical incisions. Br J Surg 103:477–486
De Vries FEE, Wallert ED, Solomkin JS et al (2016) A systematic review and meta-analysis including GRADE qualification of the risk of surgical site infections after prophylactic negative pressure wound therapy compared with conventional dressings in clean and contaminated surgery. Medicine 95:e4673
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–34
Higgins JPT, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Schwarzer G (2007) Meta: an R package for meta-analysis. R news 7:40–45
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634
Chaboyer W, Anderson V, Webster J et al (2014) Negative Pressure wound therapy on surgical site infections in women undergoing elective caesarean sections: a pilot RCT. Healthcare (Basel) 2:417–428
Gunatilake RP, Swamy GK, Brancazio LR et al (2017) Closed-incision negative-pressure therapy in obese patients undergoing cesarean delivery: a randomized controlled trial. AJP Rep 7:e151–e157
Hyldig N, Vinter CA, Kruse M et al (2018) Prophylactic incisional negative pressure wound therapy reduces the risk of surgical site infection after caesarean section in obese women: a pragmatic randomised clinical trial. BJOG 01:01
Ruhstaller K, Downes KL, Chandrasekaran S et al (2017) Prophylactic wound vacuum therapy after cesarean section to prevent wound complications in the obese population: a randomized controlled trial (the ProVac study). Am J Perinatol 34:1125–1130
Wihbey KA, Joyce EM, Spalding ZT et al (2018) Prophylactic negative pressure wound therapy and wound complication after cesarean delivery in women with class II or III obesity: a randomized controlled trial. Obstet Gynecol 132:377–384
Li P-Y, Yang D, Liu D et al (2017) Reducing surgical site infection with negative-pressure wound therapy after open abdominal surgery: a prospective randomized controlled study. Scand J Surg 106:189–195
Murphy PB, Knowles S, Chadi SA et al (2018) Negative pressure wound therapy use to decrease surgical nosocomial events in colorectal resections (NEPTUNE): a randomized controlled trial. Ann Surg 29:29
O’Leary DP, Peirce C, Anglim B et al (2017) Prophylactic negative pressure dressing use in closed laparotomy wounds following abdominal operations: a randomized, controlled, open-label trial: the P.I.C.O Trial. Ann Surg 265:1082–1086
Shen P, Blackham AU, Lewis S et al (2017) Phase II randomized trial of negative-pressure wound therapy to decrease surgical site infection in patients undergoing laparotomy for gastrointestinal, pancreatic, and peritoneal surface malignancies. J Am Coll Surg 224:726–737
Mangram AJ, Horan TC, Pearson ML et al (1999) Guideline for prevention of surgical site infection. Centers for disease control and prevention (CDC) hospital infection control practices advisory committee. Am J Infect Control 27(2):97–132
Uchino M, Hirose K, Bando T et al (2016) randomized controlled trial of prophylactic negative-pressure wound therapy at ostomy closure for the prevention of delayed wound healing and surgical site infection in patients with ulcerative colitis. Dig Surg 33:449–454
Willy C, Agarwal A, Andersen CA et al (2017) Closed incision negative pressure therapy: international multidisciplinary consensus recommendations. Int Wound J 14:385–398
Willy C, Engelhardt M, Stichling M, Grauhan O (2016) The impact of surgical site occurrences and the role of closed incision negative pressure therapy. Int Wound J 13(Suppl 3):35–46
Pellino G, Sciaudone G, Selvaggi F, Canonico S (2015) Prophylactic negative pressure wound therapy in colorectal surgery. Effects on surgical site events: current status and call to action. Updates Surg 67:235–245
Imamura K, Adachi K, Sasaki R et al (2016) randomized comparison of subcuticular sutures versus staples for skin closure after open abdominal surgery: a multicenter open-label randomized controlled trial. J Gastrointest Surg 20:2083–2092
Okubo S, Gotohda N, Sugimoto M et al (2018) Abdominal skin closure using subcuticular sutures prevents incisional surgical site infection in hepatopancreatobiliary surgery. Surgery 164:251–256
de Jonge SW, Gans SL, Atema JJ et al (2017) Timing of preoperative antibiotic prophylaxis in 54,552 patients and the risk of surgical site infection: a systematic review and meta-analysis. Medicine 96:e6903
Toh JWT, Phan K, Hitos K et al (2018) Association of mechanical bowel preparation and oral antibiotics before elective colorectal surgery with surgical site infection: a network meta-analysis. JAMA Netw Open 1:e183226
Kang SI, Oh H-K, Kim MH et al (2018) Systematic review and meta-analysis of randomized controlled trials of the clinical effectiveness of impervious plastic wound protectors in reducing surgical site infections in patients undergoing abdominal surgery. Surgery 164:939–945
Howell RD, Hadley S, Strauss E, Pelham FR (2011) Blister formation with negative pressure dressings after total knee arthroplasty. Curr Orthop Pract 22:176
Karlakki S, Brem M, Giannini S et al (2013) Negative pressure wound therapy for management of the surgical incision in orthopaedic surgery: a review of evidence and mechanisms for an emerging indication. Bone Joint Res 2:276–284
Peinemann F, McGauran N, Sauerland S, Lange S (2008) Negative pressure wound therapy: potential publication bias caused by lack of access to unpublished study results data. BMC Med Res Methodol 8:4
Peinemann F, Labeit A (2018) Negative pressure wound therapy: a systematic review of randomized controlled trials from 2000 to 2017. J Evid Based Med 20:20
Alexander HC, Bartlett AS, Wells CI et al (2018) Reporting of complications after laparoscopic cholecystectomy: a systematic review. HPB 20:786–794
Bruce J, Russell EM, Mollison J, Krukowski ZH (2001) The quality of measurement of surgical wound infection as the basis for monitoring: a systematic review. J Hosp Infect 49:99–108
Hyldig N, Joergensen JS, Wu C et al (2018) Cost-effectiveness of incisional negative pressure wound therapy compared with standard care after caesarean section in obese women: a trial-based economic evaluation. BJOG 03:03
Heard C, Chaboyer W, Anderson V et al (2017) Cost-effectiveness analysis alongside a pilot study of prophylactic negative pressure wound therapy. J Tissue Viability 26:79–84
Schulz KF, Altman DG, Moher D, CONSORT Group (2011) CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg 9:672–677
Brölmann FE, Eskes AM, Sumpio BE et al (2013) Fundamentals of randomized clinical trials in wound care: reporting standards. Wound Repair Regen 21:641–647
Gillespie BM, Webster J, Ellwood D et al (2016) ADding negative pRESSure to improve healING (the DRESSING trial): a RCT protocol. BMJ Open 6:e010287
Mihaljevic AL, Schirren R, Müller TC et al (2015) Postoperative negative-pressure incision therapy following open colorectal surgery (Poniy): study protocol for a randomized controlled trial. Trials 16:471
Sandy-Hodgetts K, Leslie GD, Parsons R et al (2017) Prevention of postsurgical wound dehiscence after abdominal surgery with NPWT: a multicentre randomised controlled trial protocol. J Wound Care 26:S23–S26
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wells, C.I., Ratnayake, C.B.B., Perrin, J. et al. Prophylactic Negative Pressure Wound Therapy in Closed Abdominal Incisions: A Meta-analysis of Randomised Controlled Trials. World J Surg 43, 2779–2788 (2019). https://doi.org/10.1007/s00268-019-05116-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-019-05116-6