Abstract
Background
To evaluate the outcome of duodenopancreatic reoperations in patients with multiple endocrine neoplasia type 1 (MEN1).
Methods
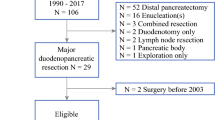
MEN1 patients who underwent reoperations for duodenopancreatic neuroendocrine neoplasms (dpNENs) were retrieved from a prospective database and retrospectively analyzed.
Results
Twelve of 101 MEN1 patients underwent up to three reoperations, resulting in a total of 18 reoperations for dpNEN recurrence. Patients initially underwent either formal pancreatic resections (n = 7), enucleations (n = 3), or duodenotomy with lymphadenectomy for either NF-pNEN (seven patients), Zollinger–Ellison syndrome (ZES, three patients), organic hyperinsulinism (one patient) or VIPoma (one patient). Six patients had malignant dpNENs with lymph node (n = 5) and/or liver metastases (n = 2). The indication of reoperations was NF-pNEN (five patients), ZES (five patients), organic hyperinsulinism (one patient), and recurrent VIPoma (one patient). Median time to first reoperation was 67.5 (range 6–251) months. Five patients required a second duodenopancreatic reoperation for 60–384 months after initial surgery, and one patient underwent a third reoperation after 249 months. The rate of complications (Clavien–Dindo ≥3) was 28%. Four patients required completion pancreatectomy. Six patients developed pancreoprivic diabetes. After a median follow-up of 18 (6–34) years after initial surgery, ten of 12 patients are alive, one died of metastatic pancreatic VIPoma, and one died of metastatic thymic NEN.
Conclusion
Reoperations are frequently necessary for dpNEN in MEN1 patients, but are not associated with an increased perioperative morbidity in specialized centers. Organ-sparing resections should be preferred as initial duodenopancreatic procedures to maintain pancreatic function and avoid completion pancreatectomy.
Similar content being viewed by others
References
Goudet P, Murat A, Binquet C et al (2010) Risk factors and causes of death in MEN1 disease. A GTE (Groupe d’Etude des Tumeurs Endocrines) cohort study among 758 patients. World J Surg 34:249–255
Gibril F, Venzon DJ, Ojeaburu JV et al (2001) Prospective study of the natural history of gastrinoma in patients with MEN1: definition of an aggressive and a nonaggressive form. J Clin Endocrinol Metab 86:5282–5293
Ito T, Igarashi H, Uehara H et al (2013) Causes of death and prognostic factors in multiple endocrine neoplasia type 1: a prospective study: comparison of 106 MEN1/Zollinger–Ellison syndrome patients with 1613 literature MEN1 patients with or without pancreatic endocrine tumors. Medicine (Baltimore) 92:135–181
Lopez CL, Waldmann J, Fendrich V et al (2011) Long-term results of surgery for pancreatic neuroendocrine neoplasms in patients with MEN1. Langenbecks Arch Surg 396:1187–1196
Triponez F, Dosseh D, Goudet P et al (2006) Epidemiology data on 108 MEN 1 patients from the GTE with isolated nonfunctioning tumors of the pancreas. Ann Surg 243:265–272
Triponez F, Goudet P, Dosseh D et al (2006) Is surgery beneficial for MEN1 patients with small (< or = 2 cm), nonfunctioning pancreaticoduodenal endocrine tumor? An analysis of 65 patients from the GTE. World J Surg 30:654–662 discussion 663-664
Anlauf M, Schlenger R, Perren A et al (2006) Microadenomatosis of the endocrine pancreas in patients with and without the multiple endocrine neoplasia type 1 syndrome. Am J Surg Pathol 30:560–574
Thakker RV, Newey PJ, Walls GV et al (2012) Clinical practice guidelines for multiple endocrine neoplasia type 1 (MEN1). J Clin Endocrinol Metab 97:2990–3011
Newey PJ, Jeyabalan J, Walls GV et al (2009) Asymptomatic children with multiple endocrine neoplasia type 1 mutations may harbor nonfunctioning pancreatic neuroendocrine tumors. J Clin Endocrinol Metab 94:3640–3646
Polenta V, Slater EP, Kann PH et al (2018) Preoperative Imaging Overestimates the tumor size in pancreatic neuroendocrine neoplasms associated with multiple endocrine neoplasia type 1. World J Surg 42:1440–1447
Partelli S, Tamburrino D, Lopez C et al (2016) Active surveillance versus surgery of nonfunctioning pancreatic neuroendocrine neoplasms ≤2 cm in MEN1 patients. Neuroendocrinology 103:779–786
Jensen RT, Norton JA (2017) Treatment of pancreatic neuroendocrine tumors in multiple endocrine neoplasia type 1: some clarity but continued controversy. Pancreas 46:589–594
Ito T, Hijioka S, Masui T et al (2017) Advances in the diagnosis and treatment of pancreatic neuroendocrine neoplasms in Japan. J Gastroenterol 52:9–18
Akerstrom G, Hessman O, Skogseid B (2002) Timing and extent of surgery in symptomatic and asymptomatic neuroendocrine tumors of the pancreas in MEN 1. Langenbecks Arch Surg 386:558–569
Adkisson CD, Stauffer JA, Bowers SP et al (2012) What extent of pancreatic resection do patients with MEN-1 require? JOP 13:402–408
Bartsch DK, Albers M, Knoop R et al (2013) Enucleation and limited pancreatic resection provide long-term cure for insulinoma in multiple endocrine neoplasia type 1. Neuroendocrinology 98:290–298
Nell S, Borel Rinkes IHM, Verkooijen HM et al (2018) Early and late complications after surgery for MEN1-related nonfunctioning pancreatic neuroendocrine tumors. Ann Surg 267:352–356
Hausman MS Jr, Thompson NW, Gauger PG et al (2004) The surgical management of MEN-1 pancreatoduodenal neuroendocrine disease. Surgery 136:1205–1211
Gauger PG, Doherty GM, Broome JT et al (2009) Completion pancreatectomy and duodenectomy for recurrent MEN-1 pancreaticoduodenal endocrine neoplasms. Surgery 146:801–806 discussion 807-808
Falconi M, Eriksson B, Kaltsas G et al (2016) ENETS consensus guidelines update for the management of patients with functional pancreatic neuroendocrine tumors and non-functional pancreatic neuroendocrine tumors. Neuroendocrinology 103:153–171
Manoharan J, Albers MB, Bartsch DK (2017) The future: diagnostic and imaging advances in MEN1 therapeutic approaches and management strategies. Endocr Relat Cancer 24:T209–T225
Albers MB, Librizzi D, Lopez CL et al (2017) Limited value of Ga-68-DOTATOC-PET-CT in routine screening of patients with multiple endocrine neoplasia type 1. World J Surg 41:1521–1527
Lopez CL, Falconi M, Waldmann J et al (2013) Partial pancreaticoduodenectomy can provide cure for duodenal gastrinoma associated with multiple endocrine neoplasia type 1. Ann Surg 257:308–314
Bartsch DK, Slater EP, Albers M et al (2014) Higher risk of aggressive pancreatic neuroendocrine tumors in MEN1 patients with MEN1 mutations affecting the CHES1 interacting MENIN domain. J Clin Endocrinol Metab 99:E2387–2391
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13
Panwar R, Pal S (2017) The international study group of pancreatic surgery definition of delayed gastric emptying and the effects of various surgical modifications on the occurrence of delayed gastric emptying after pancreatoduodenectomy. Hepatobiliary Pancreat Dis Int 16:353–363
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Kann PH, Kann B, Fassbender WJ et al (2006) Small neuroendocrine pancreatic tumors in multiple endocrine neoplasia type 1 (MEN1): least significant change of tumor diameter as determined by endoscopic ultrasound (EUS) imaging. Exp Clin Endocrinol Diabetes 114:361–365
Partelli S, Tamburrino D, Lopez C et al (2016) Active surveillance versus surgery of nonfunctioning pancreatic neuroendocrine neoplasms ≤2 cm in MEN1 patients. Neuroendocrinology 103:779–786
Bartsch DK, Albers MB (2015) Controversies in surgery for multiple endocrine neoplasia type 1-related Zollinger–Ellison syndrome. Int J Endocr Oncol 2:71–263
Acknowledgements
We thank all MEN1 patients participating in our controlled screening program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Albers, M.B., Manoharan, J., Bollmann, C. et al. Results of Duodenopancreatic Reoperations in Multiple Endocrine Neoplasia Type 1. World J Surg 43, 552–558 (2019). https://doi.org/10.1007/s00268-018-4809-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4809-1