Abstract
Background
Postoperative delirium after liver transplantation is relatively common, especially due to preexisting conditions such as hepatic encephalopathy. Most studies of delirium after liver transplantation were based on ICU practices using deep hypnosedation. Therefore, risk factors and consequences of postoperative delirium after liver transplantation were evaluated in the light sedation era.
Methods
A total of 253 liver transplantation patients were evaluated for postoperative delirium. Clinical outcomes including mortality were compared between patients who suffered delirium and those who did not. Risk factors for postoperative delirium were analyzed with subgroup analysis depending on MELD scores and type of liver transplantation.
Results
Post-liver transplant delirium developed in 17% of the patients, 88% of which occurred within the first postoperative day. Alcoholic liver cirrhosis, class C Child–Pugh score, higher MELD scores, higher proportion of deceased donor liver transplantation, and reintubation were more frequent in patients who developed delirium, but there was no difference in mortality. Higher preoperative MELD group (15–24 vs. <15; OR 4.10, 95% Cl [1.67–10.09], P = 0.002, ≥25 vs. <15; OR 5.59, 95% CI [2.06–15.19], P < 0.01), higher APACHE II scores (OR 5.59, 95% CI [2.06–15.19], P < 0.01), and reintubation (OR 6.46, 95% CI [2.10–19.88], P < 0.01) were identified as significant risk factors for postoperative delirium.
Conclusion
Postoperative delirium after liver transplantation was associated with worse clinical outcomes. MELD scores greater than 15 were predictive of postoperative delirium in both living and deceased donor liver transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In critically ill patients, delirium is a relatively common complication with ramifications such as prolonged ICU length of stay [1] and prolonged mechanical ventilation [2], as well as increased mortality [1,2,3]. It has also been associated with long-term neurologic deterioration such as cognitive impairment [4] and dementia [5].
Due to impaired liver function, patients undergoing liver transplantation (LT) frequently present with some degree of encephalopathy. In addition, a significant proportion of LT patients has a history of alcoholism. Therefore, liver transplant recipients may be at a higher risk for developing postoperative delirium in the ICU with a reported incidence between 10.3 and 26.7% [6, 7]. However, most studies of postoperative delirium after LT were reported before the paradigm shift to light ICU sedation with priority to analgesia.
The approach toward sedation and delirium in ICU patients has changed with more emphasis on light sedation and early rehabilitation as highlighted in the 2013 pain, agitation, and delirium guidelines [8]. The aim of our study was to investigate associated risk factors and the incidence of postoperative delirium in LT patients who were managed in accordance with the updated guidelines.
Methods
This retrospective study was approved by the institutional review board of the Seoul National University hospital (1506-099-681). Informed consent was waived by the institutional review board.
Anesthesia and liver transplantation
All LTs were performed by one surgical team who collectively perform more than 150 liver transplants per year. Anesthesia was induced with propofol, rocuronium, and sevoflurane and maintained with sevoflurane and cis-atracurium under standard monitoring from a dedicated anesthesia team. Portal and hepatic veins were anastomosed without venovenous bypass or portocaval shunt and anastomosis of the hepatic artery and bile duct were performed after graft reperfusion. Intraoperatively, serum electrolytes and arterial blood gas were checked and managed accordingly. Patients were transferred to the surgical intensive care unit without extubation for postoperative care. When required, dexmedetomidine was considered for sedation with a target of 0 to −2 on the Richmond Agitation Sedations scale after appropriate treatment for pain. All patients received intravenous patient-controlled analgesia (PCA) with morphine and fentanyl for postoperative analgesia. The PCA consisted of 0.6 mg of morphine and 15 mcg of fentanyl per ml in a total volume of 100 ml with a basal rate of 1 ml/h, bolus dose of 0.5 ml, and a lock out time of 15 min.
Immunosuppression after LT was based on triple immunosuppressive regimen with calcineurin inhibitor, mycophenolate mofetil, and steroids. Doses of tacrolimus or cyclosporine were adjusted depending on each patient’s clinical condition, and mycophenolate mofetil was adjusted according to the associated side effects. Intravenous methylprednisolone 500 mg was given intraoperatively before portal perfusion and tapered from 200 to 20 mg within 6 days, and oral prednisolone was continued at 20 mg daily thereafter. It was tapered to 0–5 mg/day until 6 months post-LT.
Study protocol and data collection
Patients admitted to the surgical intensive care unit after LT operation from November 2012 to December 2014 were included in this study. Pediatric patients (<18 years of age), co-transplant patients, and patients with a Glasgow Coma Scale (GCS) <13 or inability to follow command on postoperative day 0 were excluded. We conducted an analysis of information based on electronic medical records for included patients. Perioperative factors potentially associated with delirium were evaluated, which includes age, sex, donor status, operation type, initial diagnoses, coexisting diseases, hepatic encephalopathy grade, Model for End-Stage Liver Disease (MELD) score, and preoperative GCS score. Patients were also grouped according to their MELD scores (<15, 15–24, and ≥25), which largely correlate with previous United Network for Organ Sharing statuses 3, 2B, and sick 2B and 2A, respectively [9]. Intraoperative RBC transfusion and duration of surgery were evaluated as perioperative factors. Collected postoperative factors were the Acute Physiologic and Chronic Health Evaluation (APACHE) II score, use of opioid/sedatives/inotropics, postoperative RBC transfusion, reoperation, reintubation, mechanical ventilation duration, postoperative ICU stay, postoperative hospital stay, in-hospital mortality, and 1-year mortality. Postoperative acute kidney injury according to the risk, injury, failure, loss, and end-stage kidney disease (RIFLE) criteria [10], postoperative renal replacement therapy, vascular and biliary complications requiring intervention, and surgical site infection were collected. Patient characteristics and outcomes between living donor LT and deceased LT were also compared.
Delirium assessment
The incidence of postoperative delirium was assessed using the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) [11]. Each ICU nurse was trained for CAM-ICU using educational materials (relevant literature, handouts, CAM-ICU tools, and a video about detailed application of CAM-ICU) and subsequent bedside training. CAM-ICU was performed by the ICU nurse once per each 8-h shift, or three times a day. Patients with three or more missing CAM-ICU data were excluded from the study. For patients with 1 or 2 missing CAM-ICU data, the immediately preceding CAM-ICU data were carried over.
Statistical analysis
Statistical analyses were performed by using SPSS version 22 (SPSS Inc., Chicago, Illinois, USA) and SAS statistical software (SAS system for Windows, version 9.2; SAS institute, Cary, NC). Patient data were expressed as median [range] and number (percentage). Continuous variables were analyzed with Student`s t test or Mann–Whitney U test after assessing normality with the Kolmogorov–Smirnov test. Categorical variables were analyzed with Chi-square test or Fisher exact test. To identify significant risk factors of delirium, significant variables yielding P < 0.1 by univariate analysis were included in the multivariate analysis with forward selection. We added hypertension and alcoholics which widely have known as delirium risk factors to multivariate logistic regression analysis. Collinearity between variables was assessed before modeling, and if present (Pearson`s correlation coefficient > 0.7), only one variable was included into the statistical analysis. Calibration was assessed using the Hosmer–Lemeshow goodness-of-fit test, with a P value > 0.05 indicating adequate model fit of the data. Statistical significance was defined as P < 0.05 (two-tailed). The Kaplan–Meier method using the log rank test was used to compare ICU and hospital length of stay and in-hospital and 1-year mortality between no-delirium group and delirium group. Cox proportional hazard models were used to assess the association between delirium after liver transplant in ICU and outcomes including length of ICU and hospital stay, in-hospital mortality and 1-year mortality.
Results
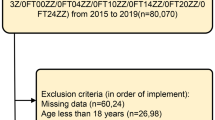
After excluding 27 pediatric patients (<18 years) and 1 simultaneous kidney liver transplant patient, 253 patients were included and analyzed (Fig. 1). Additionally, 14 patients who were unable to cooperate on postoperative day 0 were excluded.
Of the 253 patients, 43 (17.0%) developed delirium during ICU stay after LT. Approximately, 88% (38/43) of delirium occurred on the day of transplantation or the first postoperative day (Fig. 2). The duration of delirium was 1.9 [0.3–5.0] days. Patients with delirium showed higher rate of alcoholic liver cirrhosis (27.9 vs. 12.4%, P = 0.02), higher rate of C class of Child–Pugh score (CPS) (65.1 vs. 24.8%, P < 0.01), higher median MELD score (22 [7–53] vs. 13 [6–51], P < 0.01)), higher proportion of deceased donor liver transplant (55.8 vs. 22.9%, P < 0.01), and reintubation (23.3 vs. 4.3%, P < 0.01) (Table 1).
Impact of delirium
Patients with delirium showed longer duration of mechanical ventilation (5 [1–114] vs. 10 [3–369] h, P = 0.04) and longer ICU (4.1 [2.1–14.9] vs. 5.8 [2.4–39.9] days, P < 0.01) and hospital length of stay (21 [4–305] vs. 38 [12–268] days, P < 0.01) compared to patients without delirium (Table 2). There was no difference in mortality between the two groups. After adjusting for APACHE II scores, delirium was associated with longer ICU length of stay (hazard ratio (HR) 2.21, 95% CI [1.53–3.19], P < 0.001) and postoperative hospital length of stay (HR 1.92, 95% CI [1.35–2.74], P < 0.001), but not with in-hospital or 1-year mortality.
Postoperative acute kidney injury and renal replacement therapy and vascular interventions of hepatic artery, portal vein, and hepatic veins were not significant different between patients with and without delirium (supplementary table 1).
Risk factors of delirium
Higher preoperative MELD group (15–24 vs. <15; OR 4.10, 95% Cl [1.67–10.09], P = 0.002, ≥25 vs. <15; OR 5.59, 95% CI [2.06–15.19], P < 0.01), higher APACHE II scores (OR 5.59, 95% CI [2.06–15.19], P < 0.01), and reintubation (OR 6.46, 95% CI [2.10–19.88], P < 0.01) were identified as significant risk factors for postoperative delirium after adjusting for donor type, alcoholic liver cirrhosis, preoperative sodium level, and inotropic support during ICU stay (Table 3). Higher preoperative MELD group was also the only common risk factor of postoperative delirium in living donor LT (15–24 vs. <15; OR 3.94, 95% Cl [1.19–13.18], P = 0.03, ≥25 vs. <15; OR 7.21, 95% CI [1.59–32.73], P = 0.01) and deceased donor LT (15–24 vs. <15; OR 24.42, 95% Cl [1.44–413.22], P = 0.03, ≥25 vs. <15, OR 19.29, 95% CI [1.31–273.31], P = 0.03) (Table 3). Diabetes mellitus (OR 3.73, 95% CI [1.18–11.76], P = 0.03) and reintubation (OR 6.46, 95% CI [2.10–19.88], P < 0.01) were also associated with postoperative delirium in living donor LT after adjusting for age, alcoholic liver cirrhosis, preoperative ammonia level, intraoperative RBC transfusion, and postoperative dexmedetomidine use. Additional risk factors of delirium in deceased donor LT was higher APACHE II scores (OR 1.26, 95% CI [1.08–1.46], P < 0.01) after adjusting for preoperative ammonia and reintubation (Table 3).
Effect of donor type
Nineteen patients (10.5%) developed delirium after living donor LT compared to 24 patients (33%) after deceased donor LT. Postoperative delirium after living donor LT was associated with higher MELD scores (15 [7–37] vs. 11 [6–51], P = 0.02), lower median sodium levels (137 [119–141] vs. 139 [120–148], P = 0.01), more intraoperative RBC transfusion (2 [0–6] vs. 0 [0–17], P = 0.01), and more postoperative midazolam (3 (15.8), vs. 2 (1.2), P = 0.01). Postoperative delirium after deceased donor LT was associated with higher preoperative MELD scores (24 [13–53] vs. 18 [6–49], P < 0.01), higher preoperative ammonia levels (115 [40–306] vs. 90 [0–229], P < 0.01), and higher APACHE II scores (27 [15–34] vs. 22 [4–39], P < 0.01). Patients with delirium also showed longer ICU and hospital length of stay after both living and deceased donor LT (supplemental table 2).
Discussion
The main findings of our study are (1) the incidence of delirium after LT was 17% with over 2/3 of delirium presenting within the first postoperative day, (2) delirium was more frequent in deceased donor LT compared to living donor LT, and (3) higher MELD score group was a common risk factor both in living donor and deceased donor LT.
The incidence of delirium after LT in our study (17%) is comparable with other studies (10.3–26.7%) [6, 7, 12]. A recent study reported a significantly higher incidence of delirium after living donor LT of about 50% [13]. The discrepancy of delirium incidence might be attributed to the different proportion of patients with alcoholic liver cirrhosis and preoperative hepatic encephalopathy. In contrast to the 5.5% (14/253) incidence of preoperative hepatic encephalopathy and 15% (38/253) incidence of alcoholic liver cirrhosis in our study, 42.3% (33/78) of patients had preoperative hepatic encephalopathy and 42.3% (33/78) of patients had alcoholic liver disease [13].
More than 80% (38/43) of delirium episodes in our study occurred on either postoperative day 0 or 1. This was consistent with results in surgical ICU patients who did not require MV [14], as well as mechanically ventilated medical ICU patients [15]. Only one study evaluated the onset of delirium after LT, which reported about 50% of delirium developed delirium within 5.5 days of transplantation [13]. The plausible explanation would be that the transplanted liver starts to clear metabolites in the first few days.
In accordance with previous studies, patients with delirium after LT had longer mechanical ventilation duration [12, 13] and stayed longer in the ICU [12, 16] and the hospital [6, 12, 13, 16]. In contrast to previous studies [6], there was no difference in in-hospital mortality and 1-year mortality most likely due to the relatively low in-hospital (2.3%) and 1-year (7.0%) mortality in our patients with delirium.
Patients who undergo LT tend to have underlying conditions associated with the development of delirium. Liver cirrhosis contributes to predisposing factors of delirium such as frequent electrolyte imbalance and kidney injury [17], infection [18], and hepatic encephalopathy [12, 13, 19]. In addition, extensive intraoperative blood loss and transfusion [6] and postoperative calcineurin inhibitors for immunosuppression [20] may contribute to postoperative delirium after LT.
Preoperative hepatic encephalopathy has been reported as a predictor of delirium in post-liver transplant patients [12, 13]. In our study, only 1.2% (3/253) of patients showed overt hepatic encephalopathy (West Haven grade 2 or greater) [21], whereas the prevalence of hepatic encephalopathy ranged from 21 to 42.3% in studies that reported hepatic encephalopathy as a risk factor of delirium [12, 13]. The Confusion Assessment Method (CAM) was suggested as a screening tool for delirium in patients with suspected hepatic encephalopathy [22]. CAM-ICU has been used in critically ill patient with cirrhosis [23] and LT patients [13, 24], successfully diagnosing delirium, even in patients with hepatic encephalopathy [13, 24].
In accordance with the recent guidelines [8], dexmedetomidine has been used in our ICU for patients as the primary sedative for agitation with a target Richmond Agitation Sedation Scale of 0 to −2. Midazolam infusion was used in four patients (of which one patient developed delirium) for sedation because of extracorporeal membrane oxygenation support and acute respiratory distress syndrome. Due to limited use, midazolam was not identified as a risk factor of delirium both in univariable and multivariable regression analyses.
In our study, identified risk factors of delirium included preoperative MELD group and APACHE II scores in deceased donor LT, and reintubation and diabetes in living donor LT. MELD scores have been used to represent severity of liver disease, prioritize liver allocation, and predict mortality of patients awaiting LT [25]. In our study, MELD scores >15 were associated with delirium after living donor and deceased donor LT. In accordance with the recent guidelines and previous studies of delirium after LT [6, 24], APACHE II scores were also found to be associated with delirium after deceased donor LT [8]. LT patients with high MELD or APACHE II scores may benefit from interventions such as early mobilization and physical therapy, which have been shown to prevent delirium in other critically ill patients [26].
Our study found that patients requiring reintubation during ICU stay were more likely to develop delirium. Reintubation was performed in patients with severe bleeding requiring reoperation, desaturation due to pulmonary edema or pneumonia, CO2 retention, or severe metabolic acidosis due to hepatic dysfunction. Thus, reintubation is likely to be an index of severity of illness during ICU stay. Disease severity as MELD score preoperatively, APACHE II score at ICU admission, and reintubation during ICU stay were associated with delirium after LT. However, it is still unclear whether delirium is the cause of the disease severity or one of the consequences.
Our study is the first study to compare the two types of LT and show that patients undergoing deceased donor LT were more likely to develop delirium compared to patients undergoing living donor LT (33 vs. 10.5%). Deceased donor LT patients had higher MELD scores (20 [6–53]) vs. 11 [6–51]), higher APACHE II scores, longer preoperative hospital length of stay (17 [0–76] vs. 3 [2–53]), more intraoperative and postoperative RBC transfusion, and required more inotropic support during the ICU stay compared to living donor LT patients. However, donor type itself was not associated with post-transplant delirium after adjusting for relevant factors.
Our study has several limitations. First, due to the retrospective nature of the analysis, some variables potentially associated with delirium after LT may not have been adjusted for in the analysis. The results may have been affected by confounders or systematic bias and the predominant proportion of living donor LT. Negative results should be interpreted with caution due to the possibility of insufficient sample size. Second, our study was conducted in a single center with a high proportion of hepatitis B patients and few alcoholic liver cirrhosis patients. Identified risk factors of delirium such as MELD group in deceased donor LT showed relatively wide confidence intervals, which may be due to the small number of deceased donor LT number. Therefore, application of these risk factors to different patient mix should be done with caution. Third, although CAM-ICU was routinely used for more than 6 years, the experience level of bedside nurses might affect the results. Also, pretest bias may have affected the diagnosis of delirium, as CAM-ICU was performed by bedside nurses who were aware of the patient’s condition and past medical history. Lastly, midazolam was used only in 4.7% patients with delirium. Although the target RASS for sedation was 0 to −2, the use of sedatives may have confounded the results of CAM-ICU in light of recent studies [27, 28]. However, serial CAM-ICU was performed in patients for sufficient periods after complete cessation of sedation. Also, multivariable analysis did not identify the use of midazolam as a risk factor of delirium.
In conclusion, high preoperative MELD score (≥15) seems to be an independent risk factor of delirium after living donor and deceased donor LT. Further study is required to identify modifiable preoperative or postoperative risk factors of delirium after LT.
References
Thomason JW, Shintani A, Peterson JF et al (2005) Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care 9:R375–R381
Lin SM, Huang CD, Liu CY et al (2008) Risk factors for the development of early-onset delirium and the subsequent clinical outcome in mechanically ventilated patients. J Crit Care 23:372–379
Pisani MA, Kong SY, Kasl SV et al (2009) Days of delirium are associated with 1-year mortality in an older intensive care unit population. Am J Respir Crit Care Med 180:1092–1097
Norman BC, Jackson JC, Graves JA et al (2016) Employment outcomes after critical illness: an analysis of the bringing to light the risk factors and incidence of neuropsychological dysfunction in ICU survivors cohort. Crit Care Med 44:2003–2009
Pandharipande PP, Girard TD, Jackson JC et al (2013) Long-term cognitive impairment after critical illness. N Engl J Med 369:1306–1316
Lescot T, Karvellas CJ, Chaudhury P et al (2013) Postoperative delirium in the intensive care unit predicts worse outcomes in liver transplant recipients. Can J Gastroenterol 27:207–212
Chiu NM, Chen CL, Cheng AT (2009) Psychiatric consultation for post-liver-transplantation patients. Psychiatry Clin Neurosci 63:471–477
Barr J, Fraser GL, Puntillo K et al (2013) Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 41:263–306
Onaca NN, Levy MF, Sanchez EQ et al (2003) A correlation between the pretransplantation MELD score and mortality in the first two years after liver transplantation. Liver Transpl 9:117–123
Bellomo R, Ronco C, Kellum JA et al (2004) Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the acute dialysis quality initiative (ADQI) group. Crit Care 8:R204–R212
Ely EW, Margolin R, Francis J et al (2001) Evaluation of delirium in critically ill patients: validation of the confusion assessment method for the intensive care unit (CAM-ICU). Crit Care Med 29:1370–1379
Oliver N, Bohorquez H, Anders S et al (2017) Post-liver transplant delirium increases mortality and length of stay. Ochsner J 17:25–30
Wang SH, Wang JY, Lin PY et al (2014) Predisposing risk factors for delirium in living donor liver transplantation patients in intensive care units. PLoS ONE 9:e96676
Serafim RB, Dutra MF, Saddy F et al (2012) Delirium in postoperative nonventilated intensive care patients: risk factors and outcomes. Ann Intensive Care 2:51
Ely EW, Shintani A, Truman B et al (2004) Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA 291:1753–1762
Bhattacharya B, Maung A, Barre K et al (2017) Postoperative delirium is associated with increased intensive care unit and hospital length of stays after liver transplantation. J Surg Res 207:223–228
Belcher JM, Garcia-Tsao G, Sanyal AJ et al (2013) Association of AKI with mortality and complications in hospitalized patients with cirrhosis. Hepatology 57:753–762
Merli M, Lucidi C, Giannelli V et al (2010) Cirrhotic patients are at risk for health care-associated bacterial infections. Clin Gastroenterol Hepatol 8:979–985
Jepsen P, Ott P, Andersen PK et al (2010) Clinical course of alcoholic liver cirrhosis: a Danish population-based cohort study. Hepatology 51:1675–1682
Beresford TP (2001) Neuropsychiatric complications of liver and other solid organ transplantation. Liver Transpl 7:S36–S45
Ferenci P, Lockwood A, Mullen K et al (2002) Hepatic encephalopathy–definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th world congresses of gastroenterology, Vienna, 1998. Hepatology 35:716–721
Cordoba J (2011) New assessment of hepatic encephalopathy. J Hepatol 54:1030–1040
Orman ES, Perkins A, Ghabril M et al (2015) The confusion assessment method for the intensive care unit in patients with cirrhosis. Metab Brain Dis 30:1063–1071
Binda F, Galazzi A, Brambilla A et al (2017) Risk factors for delirium in intensive care unit <BR> in liver transplant patients. Assist Inferm Ric 36:90–97
Wiesner R, Edwards E, Freeman R et al (2003) Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology 124:91–96
Schweickert WD, Pohlman MC, Pohlman AS et al (2009) Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet 373:1874–1882
Haenggi M, Blum S, Brechbuehl R et al (2013) Effect of sedation level on the prevalence of delirium when assessed with CAM-ICU and ICDSC. Intensive Care Med 39:2171–2179
Patel SB, Poston JT, Pohlman A et al (2014) Rapidly reversible, sedation-related delirium versus persistent delirium in the intensive care unit. Am J Respir Crit Care Med 189:658–665
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflict of interest to disclose as described by the World Journal of Surgery.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lee, H., Oh, SY., Yu, J.H. et al. Risk Factors of Postoperative Delirium in the Intensive Care Unit After Liver Transplantation. World J Surg 42, 2992–2999 (2018). https://doi.org/10.1007/s00268-018-4563-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4563-4