Abstract
Background
Coagulopathy can delay or complicate surgical diseases that require emergent surgical treatment. Prothrombin complex concentrates (PCC) provide concentrated coagulation factors which may reverse coagulopathy more quickly than plasma (FFP) alone. We aimed to determine the time to operative intervention in coagulopathic emergency general surgery patients receiving either PCC or FFP. We hypothesize that PCC administration more rapidly normalizes coagulopathy and that the time to operation is diminished compared to FFP alone.
Methods
Single institution retrospective review was performed for coagulopathic EGS patients during 2/1/2008 to 8/1/2016. Patients were divided into three groups (1) PCC alone (2) FFP alone and (3) PCC and FFP. The primary outcome was the duration from clinical decision to operate to the time of incision. Summary and univariate analyses were performed.
Results
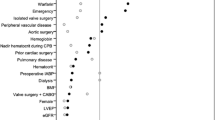
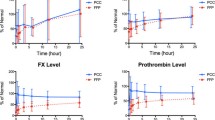
Coagulopathic EGS patients (n = 183) received the following blood products: PCC (n = 20, 11%), FFP alone (n = 119, 65%) and PCC/FFP (n = 44, 24%). The mean (± SD) patient age was 71 ± 13 years; 60% were male. The median (IQR) Charlson comorbidity index was similar in all three groups (PCC = 5(4–6), FFP = 5(4–7), PCC/FFP = 5(4–6), p = 0.33). The mean (± SD) dose of PCC administered was similar in the PCC/FFP group and the PCC alone group (2539 ± 1454 units vs. 3232 ± 1684, p = .09). The mean (±SD) time to incision in the PCC alone group was significantly lower than the FFP alone group (6.0 ± 3.6 vs. 8.8 ± 5.0 h, p = 0.01). The mean time to incision in the PCC + FFP group was also significantly lower than the FFP alone group (7.1 ± 3.6 vs. 8.8 ± 5.0, p = 0.03). The incidence of thromboembolic complications was similar in all three groups.
Conclusions
PCC, alone or in combination with FFP, reduced INR and time to surgery effectively and safely in coagulopathic EGS patients without an apparent increased risk of thromboembolic events, when compared to FFP use alone.
Level of evidence
IV single institutional retrospective review.


Similar content being viewed by others
References
Huhtakangas J, Tetri S, Juvela S, Saloheimo P, Bode MK, Hillbom M (2011) Effect of increased warfarin use on warfarin-related cerebral hemorrhage: a longitudinal population-based study. Stroke 42(9):2431–2435
Wysowski DK, Nourjah P, Swartz L (2007) Bleeding complications with warfarin use: a prevalent adverse effect resulting in regulatory action. Arch Intern Med 167(13):1414–1419
Robert-Ebadi H, Le Gal G, Righini M (2009) Use of anticoagulants in elderly patients: practical recommendations. Clin Interv Aging 4:165–177
Holbrook A, Schulman S, Witt DM, Vandvik PO, Fish J, Kovacs MJ, Svensson PJ, Veenstra DL, Crowther M, Guyatt GH (2012) Evidence-based management of anticoagulant therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest 141(2 Suppl):e152S–e184S
Bruns BR, Tesoriero R, Narayan M, Klyushnenkova EN, Chen H, Scalea TM, Diaz JJ (2015) Emergency general surgery: defining burden of disease in the State of Maryland. Am Surg 81(8):829–834
Gale SC, Shafi S, Dombrovskiy VY, Arumugam D, Crystal JS (2014) The public health burden of emergency general surgery in the United States: a 10-year analysis of the Nationwide Inpatient Sample–2001 to 2010. J Trauma Acute Care Surg 77(2):202–208
Havens JM, Peetz AB, Do WS, Cooper Z, Kelly E, Askari R, Reznor G, Salim A (2015) The excess morbidity and mortality of emergency general surgery. J Trauma Acute Care Surg. 78(2):306–311
Havens JM, Olufajo OA, Cooper ZR, Haider AH, Shah AA, Salim A (2016) Defining rates and risk factors for readmissions following emergency general surgery. JAMA Surg 151(4):330–336
Patel SS, Patel MS, Goldfarb M, Ortega A, Ault GT, Kaiser AM, Senagore AJ (2013) Elective versus emergency surgery for ulcerative colitis: a national surgical quality improvement program analysis. Am J Surg 205(3):333–337 discussion 7-8
Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, Sadiraj V, Sweeney JF (2012) Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg 215(3):322–330
Stewart B, Khanduri P, McCord C, Ohene-Yeboah M, Uranues S, Vega Rivera F, Mock C (2014) Global disease burden of conditions requiring emergency surgery. Br J Surg 101(1):e9–e22
Schreiber MA (2004) Damage control surgery. Crit Care Clin 20(1):101–118
Howard JL 2nd, Cipolle MD, Horvat SA, Sabella VM, Reed JF 3rd, Fulda G, Tinkoff G, Pasquale MD (2009) Preinjury warfarin worsens outcome in elderly patients who fall from standing. J Trauma 66(6):1518–1522 discussion 23-4
Chapman SA, Irwin ED, Beal AL, Kulinski NM, Hutson KE, Thorson MA (2011) Prothrombin complex concentrate versus standard therapies for INR reversal in trauma patients receiving warfarin. Ann Pharmacother 45(7–8):869–875
Baxter Healthcare Corporation (2006) Bebulin VH (Factor IX Complex) vapor heated [package insert]. Westlake Village, CA
Grifols Biologicals Inc. Profilnine SD (Factor IX Complex) [package insert]. Los Angeles, CA. 2003
Food and Drug Administration. Bebulin (Factor IX Complex), Nanofiltered and Vapor Heated. 2011
Kozek-Langenecker SA, Afshari A, Albaladejo P, Santullano CA, De Robertis E, Filipescu DC, Fries D, Gorlinger K, Haas T, Imberger G et al (2013) Management of severe perioperative bleeding: guidelines from the European society of anaesthesiology. Eur J Anaesthesiol 30(6):270–382
National Advisory Committee on Blood and Blood products. Recommendations for use of Prothrombin Complex Concentrates in Canada; May 16th, 2014
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40(5):373–383
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996 Jul;22(7):707-10. PMID 8844239
Tominaga GT, Staudenmayer KL, Shafi S, Schuster KM, Savage SA, Ross S, Muskat P, Mowery NT, Miller P, Inaba K et al (2016) The American Association for the Surgery of Trauma grading scale for 16 emergency general surgery conditions: Disease-specific criteria characterizing anatomic severity grading. J Trauma Acute Care Surg. 81(3):593–602
Belli S, Aytac HO, Yabanoglu H, Karagulle E, Parlakgumus A, Nursal TZ, Yildirim S (2015) Results of surgery in general surgical patients receiving warfarin: retrospective analysis of 61 patients. Int Surg 100(2):225–232
Ong M, Guang TY, Yang TK (2015) Impact of surgical delay on outcomes in elderly patients undergoing emergency surgery: A single center experience. World J Gastrointest Surg. 7(9):208–213
Ferreira J, DeLosSantos M (2013) The clinical use of prothrombin complex concentrate. J Emerg Med 44(6):1201–1210
Chai-Adisaksopha C, Hillis C, Siegal DM, Movilla R, Heddle N, Iorio A, Crowther M (2016) Prothrombin complex concentrates versus fresh frozen plasma for warfarin reversal. A systematic review and meta-analysis. Thromb Haemost 116(5):879–890
Rowe AS, Mahbubani PS, Bucklin MH, Clark CT, Hamilton LA (2016) Activated Prothrombin Complex Concentrate versus Plasma for Reversal of Warfarin-Associated Hemorrhage. Pharmacotherapy. 36(11):1132–1137
Kalina M, Tinkoff G, Gbadebo A, Veneri P, Fulda G (2008) A protocol for the rapid normalization of INR in trauma patients with intracranial hemorrhage on prescribed warfarin therapy. Am Surg 74(9):858–861
Leissinger CA, Blatt PM, Hoots WK, Ewenstein B (2008) Role of prothrombin complex concentrates in reversing warfarin anticoagulation: a review of the literature. Am J Hematol 83(2):137–143
Desserud KF, Veen T, Soreide K (2016) Emergency general surgery in the geriatric patient. Br J Surg 103(2):e52–e61
Perioperative management of antithrombotic therapy (2012) Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, Dunn AS, Kunz R, American College of Chest Physicians Chest. 141(2 Suppl):e326S
Author information
Authors and Affiliations
Contributions
MY wrote the first draft of the manuscript. Study design was developed by MY, KW, MR-Z, NHH, MH and MZ. Data generation was performed by Moustafa Younis, Mohamed Ray-Zack, and Nadeem H. Haddad. Data analysis and interpretation was performed by Moustafa Younis, Mohamed Ray-Zack, Matthew Hernandez and Martin Zielinski. Manuscript writing was performed by Moustafa Younis, Matthew Hernandez, Nadeem H. Haddad, Mohamed Ray-Zack and Martin Zielinski.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any potential conflicts of interest and no funding was utilized for the generation of this work. The authors do not have any honoraria, grants, or other form of payment was given to anyone to produce the manuscript.
Rights and permissions
About this article
Cite this article
Younis, M., Ray-Zack, M., Haddad, N.N. et al. Prothrombin Complex Concentrate Reversal of Coagulopathy in Emergency General Surgery Patients. World J Surg 42, 2383–2391 (2018). https://doi.org/10.1007/s00268-018-4520-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4520-2