Abstract
Background
The incidence of spontaneous rupture of hepatocellular carcinoma (HCC) is low in Europe, at less than 3%. HCC rupture remains a life-threatening complication, with mortality reported between 16 and 30%. The risk of bleeding recurrence has never been clearly evaluated in such clinical situation. The objectives of this study were to evaluate the current risk of mortality related to HCC rupture and to focus on the risk of bleeding recurrence following interventional management.
Methods
All patients admitted to 14 French–Italian surgical centers for spontaneous rupture of HCC between May 2000 and May 2012 were retrospectively included. Clinical data, imaging features, relevant laboratory data, treatment strategies, and prognoses were analyzed.
Results
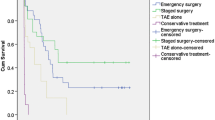
Overall, 58 of the 138 included patients (42%) had cirrhosis. Thirty-five patients (25%) presented with hemorrhagic shock, and 19% with organ(s) dysfunction. Bleeding control was obtained by interventional hemostasis, emergency liver resection, and conservative medical management in 86 (62%), 24 (18%), and 21 (15%) patients, respectively. Best supportive care was chosen for 7 (5%) patients. The mortality rate following rupture was 24%. The bleeding recurrence rate was 22% with related mortality of 52%. In multivariate analysis, a bilirubin level >17 micromol/L (HR 3.768; p = 0.006), bleeding recurrence (HR 5.400; p < 0.0001), and ICU admission after initial management (HR 8.199; p < 0.0001) were associated with in-hospital mortality.
Conclusion
This European, multicenter, large-cohort study confirmed that the prognosis of ruptured HCC is poor with an overall mortality rate of 24%, despite important advances in endovascular techniques. Overall, the rate of bleeding recurrence was more than 20%, with a related high risk of mortality.

Similar content being viewed by others
References
El-Serag HB (2007) Rudolph KL Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 132(2557–257):6
Cancer I-IAfRo GLOBOCAN (2012) estimated Cancer Incidence. Mortality and Prevalence Worldwide in 2012:2012
Vergara V, Muratore A, Bouzari H et al (2000) Spontaneous rupture of hepatocellular carcinoma: surgical resection and long-term survival. Eur J Surg Oncol 26(770–77):2
Vivarelli M, Cavallari A, Bellusci R et al (1995) Ruptured hepatocellular carcinoma: an important cause of spontaneous haemoperitoneum in Italy The European journal of surgery =. Acta chirurgica 161:881–886
Castells L, Moreiras M, Quiroga S et al (2001) Hemoperitoneum as a first manifestation of hepatocellular carcinoma in western patients with liver cirrhosis: effectiveness of emergency treatment with transcatheter arterial embolization. Dig Dis Sci 46(555–56):2
Liu CL, Fan ST, Lo CM et al (2001) Management of spontaneous rupture of hepatocellular carcinoma: single-center experience. J Clin Oncol 19(3725–373):2
Zhu LX, Liu Y (2002) Fan ST Ultrastructural study of the vascular endothelium of patients with spontaneous rupture of hepatocellular carcinoma Asian journal of surgery/Asian Surgical Association 25(157–16):2
Bassi N, Caratozzolo E, Bonariol L et al (2010) Management of ruptured hepatocellular carcinoma: implications for therapy. World journal of gastroenterology: WJG 16(1221–122):5
Battula N, Madanur M, Priest O et al (2009) Spontaneous rupture of hepatocellular carcinoma: a Western experience. Am J Surg 197(164–16):7
Kung CT, Liu BM, Ng SH et al (2008) Transcatheter arterial embolization in the emergency department for hemodynamic instability due to ruptured hepatocellular carcinoma: analysis of 167 cases AJR. Am J Roentgenol 191:W231–W239
Li WH, Cheuk EC, Kowk PC et al (2009) Survival after transarterial embolization for spontaneous ruptured hepatocellular carcinoma Journal of hepato-biliary-pancreatic surgery 16(508–51):2
Lai EC (2006) Lau WY Spontaneous rupture of hepatocellular carcinoma: a systematic review Archives of surgery 141(191–19):8
Okazaki M, Higashihara H, Ono H et al (1991) Percutaneous embolization of ruptured splanchnic artery pseudoaneurysms. Acta Radiol 32(349–35):4
Leung CS, Tang CN, Fung KH et al (2002) A retrospective review of transcatheter hepatic arterial embolisation for ruptured hepatocellular carcinoma. J R Coll Surg Edinb 47(685–68):8
Corr P, Chan M, Lau WY et al (1993) The role of hepatic arterial embolization in the management of ruptured hepatocellular carcinoma. Clin Radiol 48(163–16):5
Ngan H, Tso WK, Lai CL et al (1998) The role of hepatic arterial embolization in the treatment of spontaneous rupture of hepatocellular carcinoma. Clin Radiol 53(338–34):1
Kim GM, Yoon CJ, Seong NJ et al (2013) Postpartum haemorrhage from ruptured pseudoaneurysm: efficacy of transcatheter arterial embolisation using N-butyl-2-cyanoacrylate. Eur Radiol 23:2344–2349
Jae HJ, Chung JW, Jung AY et al (2007) Transcatheter arterial embolization of nonvariceal upper gastrointestinal bleeding with N-butyl cyanoacrylate Korean journal of radiology: official journal of the Korean Radiological Society 8(48–5):6
Dave BR, Sharma A, Kalva SP et al (2011) Nine-year single-center experience with transcatheter arterial embolization for hemoptysis: medium-term outcomes. Vascular and endovascular surgery 45(258–26):8
Srivastava DN, Sharma S, Pal S et al (2006) Transcatheter arterial embolization in the management of hemobilia. Abdom Imaging 31(439–44):8
Zhu LX, Geng XP (2001) Fan ST Spontaneous rupture of hepatocellular carcinoma and vascular injury Archives of surgery 136(682–68):7
Miyayama S, Yamashiro M, Okuda M et al (2009) Anastomosis between the hepatic artery and the extrahepatic collateral or between extrahepatic collaterals: observation on angiography. Journal of medical imaging and radiation oncology 53(271–28):2
Mine T, Murata S, Ueda T et al (2014) Contribution of extrahepatic collaterals to liver parenchymal circulation after proper hepatic artery embolization. J Gastroenterol Hepatol 29(7):1515–1521
Bilbao JI, Garrastachu P, Herraiz MJ et al (2010) Safety and efficacy assessment of flow redistribution by occlusion of intrahepatic vessels prior to radioembolization in the treatment of liver tumors. Cardiovasc Intervent Radiol 33(523–53):1
Schwarz L, Huet E, Yzet T et al (2014) An extremely uncommon variant of left hepatic artery arising from the superior mesenteric artery Surgical and radiologic anatomy: SRA 36(91–9):4
Gando S, Saitoh D, Ogura H et al (2008) Natural history of disseminated intravascular coagulation diagnosed based on the newly established diagnostic criteria for critically ill patients: results of a multicenter, prospective survey. Crit Care Med 36:145–150
Bellomo R, Kellum JA (2012) Ronco C Acute kidney injury Lancet 380(756–76):6
Sallah S, Wan JY, Nguyen NP et al (2001) Disseminated intravascular coagulation in solid tumors: clinical and pathologic study. Thromb Haemost 86(828–83):3
Acknowledgements
We are grateful to Nikki Sabourin-Gibbs, Rouen University Hospital, for writing assistance and review of the manuscript in English.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
LS, MB, JZ, AH, FM, AA, RR, CD, JMR, HT, EL, GP, AS, AD, LC, YPLT, and JJT have no conflict of interest.
Rights and permissions
About this article
Cite this article
Schwarz, L., Bubenheim, M., Zemour, J. et al. Bleeding Recurrence and Mortality Following Interventional Management of Spontaneous HCC Rupture: Results of a Multicenter European Study. World J Surg 42, 225–232 (2018). https://doi.org/10.1007/s00268-017-4163-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4163-8