Abstract
Objectives
The primary management of peptic ulcers is medical treatment. Persistent exacerbation of a peptic ulcer may lead to complications (perforation and/or bleeding). There has been a trend toward the use of a less invasive surgical simple suture, simple local suture or non-operative (endoscopic/angiography) hemostasis rather than acid-reducing vagotomy (i.e., vagus nerve severance) for treating complicated peptic ulcers. Other studies have shown the relationship between high vagus nerve activity and survival in cancer patients via reduced levels of inflammation, indicating the essential role of the vagus nerve. We were interested in the role of the vagus nerve and attempted to assess the long-term systemic effects after vagus nerve severance. Complicated peptic ulcer patients who underwent truncal vagotomy may represent an appropriate study population for investigating the association between vagus nerve severance and long-term effects. Therefore, we assessed the risks of subsequent ischemic stroke using different treatment methods in complicated peptic ulcer patients who underwent simple suture/hemostasis or truncal vagotomy/pyloroplasty.
Methods
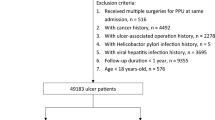
We selected 299,742 peptic ulcer patients without a history of stroke and Helicobacter pylori infection and an additional 299,742 matched controls without ulcer, stroke, and Helicobacter pylori infection from the National Health Insurance database. The controls were frequency matched for age, gender, Charlson comorbidity index (CCI) score, hypertension, hyperlipidemia history, and index year. Then, we measured the incidence of overall ischemic stroke in the two cohorts. The hazard ratio (HR) and the 95% confidence intervals (CIs) were estimated by Cox proportional hazard regression.
Results
Compared to the controls, peptic ulcer patients had a 1.86-fold higher risk of ischemic stroke. There were similar results in gender, age, CCI, hypertension, and hyperlipidemia stratified analyses. In complicated peptic ulcer patients, those who received truncal vagotomy and pyloroplasty had a lower risk of ischemic stroke than patients who received simple suture/hemostasis (HR = 0.70, 95% CI = 0.60–0.81).
Conclusions
Our findings suggest that patients with peptic ulcers have an elevated risk of subsequent ischemic stroke. Moreover, there were associations between vagotomy and a decreased risk of subsequent ischemic stroke in complicated peptic ulcer patients.


Similar content being viewed by others
References
Ramakrishnan K, Salinas RC (2007) Peptic ulcer disease. Am Fam Physician 76:1005–1012
University of Michigan Health System. Peptic ulcer disease. http://www.cme.med.umich.edu/pdf/guideline/PUD05.pdf Accessed 4 May 2007
Treiber G, Wittig J, Ammon S, Walker S, van Doorn L, Klotz U (2002) Clinical outcome and influencing factors of a new short-term quadruple therapy for Helicobacter pylori eradication: a randomized controlled trial (MACLOR study). Arch Intern Med 162:153–160
Kuipers EJ, Thijs JC, Festen HP (1995) The prevalence of Helicobacter pylori in peptic ulcer disease. Aliment Pharmacol Ther 9(Suppl 2):59–69
O’Connor A, Gisbert JP, O’Morain C et al (2015) Treatment of Helicobacter pylori Infection 2015. Helicobacter 20(Suppl 1):54–61
Malfertheiner P, Chan FK, McColl KE (2009) Peptic ulcer disease. Lancet 374(9699):1449–1461
Nyhus LM, Baker RJ, Fischer JE (1997) Mastery of surgery, 3rd edn. Little, Brown, Boston
Søreide K, Thorsen K, Harrison EM et al (2015) Perforated peptic ulcer. Lancet 386(10000):1288–1298
Wong CS, Chia CF, Lee HC et al (2013) Eradication of Helicobacter pylori for prevention of ulcer recurrence after simple closure of perforated peptic ulcer: a meta-analysis of randomized controlled trials. J Surg Res 182:219–226
Lagoo J, Pappas TN, Perez A (2014) A relic or still relevant: the narrowing role for vagotomy in the treatment of peptic ulcer disease. Am J Surg 207:120–126
Levenstein S (2000) The very model of a modern etiology: a biopsychosocial view of peptic ulcer. Psychosom Med 62:176–185
Levenstein S, Rosenstock S, Jacobsen RK et al (2015) Psychological stress increases risk for peptic ulcer, regardless of Helicobacter pylori infection or use of nonsteroidal anti-inflammatory drugs. Clin Gastroenterol Hepatol 13:498-e1–506-e1
Kotlęga D, Gołąb-Janowska M, Masztalewicz M et al (2016) The emotional stress and risk of ischemic stroke. Neurol Neurochir Pol 50:265–270
Cheng TJ, Guo HR, Chang CY et al (2016) The association between peptic ulcer disease and ischemic stroke: a population-based longitudinal study. Medicine (Baltimore) 95(22):e3797
Li C, Engstro¨m G, Hedblad B et al (2005) Risk factors for stroke in subjects with normal blood pressure: a prospective cohort study. Stroke 36:234–238
Steptoe A, Magid K, Edwards S et al (2003) The influence of psychological stress and socioeconomic status on platelet activation in men. Atherosclerosis 168:57–63
Huo Y, Schober A, Forlow SB et al (2003) Circulating activated platelets exacerbate atherosclerosis in mice deficient in apolipoprotein E. Nat Med 9:61–67
Leary MC, Saver JL (2003) Annual incidence of first silent stroke in the United States: a preliminary estimate. Cerebrovasc Dis 16:280–285
De Couck M, Maréchal R, Moorthamers S et al (2016) Vagal nerve activity predicts overall survival in metastatic pancreatic cancer, mediated by inflammation. Cancer Epidemiol 40:47–51
Romano PS, Roos LL, Jollis JG et al (1993) Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol 46(10):1075–1079
Rosenstock S, Jørgensen T, Bonnevie O et al (2003) Risk factors for peptic ulcer disease: a population based prospective cohort study comprising 2416 Danish adults. Gut 52:186–193
Malaty HM, Graham DY, Isaksson I et al (2000) Are genetic influences on peptic ulcer dependent or independent of genetic influences for Helicobacter pylori infection? Arch Intern Med 160:105–109
Malagelada JR, Ahlquist DA, Moore SC (1986) Defects in prostaglandin synthesis and metabolism in ulcer disease. Dig Dis Sci 31(Suppl 2):20S–27S
Wilson DE (1991) Role of prostaglandins in gastroduodenal mucosal protection. J Clin Gastroenterol 13(Suppl 1):S65–S71
Behrman SW (2005) Management of complicated peptic ulcer disease. Arch Surg 140:201–208
Massberg S, Brand K, Gru¨ner S et al (2002) A critical role of platelet adhesion in the initiation of atherosclerotic lesion formation. J Exp Med 196:887–896
Nijm J, Wikby A, Andrea Tompa A et al (2005) Circulating levels of proinflammatory cytokines and neutrophil-platelet aggregates in patients with coronary artery disease. Am J Cardiol 95:452–456
Huang KW, Luo JC, Leu HB et al (2012) Chronic obstructive pulmonary disease: an independent risk factor for peptic ulcer bleeding: a nationwide population-based study. Aliment Pharmacol Ther 35(7):796–802
Tseng CH, Chen JH, Muo CH et al (2015) Increased risk of ischemic stroke among patients with chronic osteomyelitis: a population-based cohort study in Taiwan. Eur J Neurol 22(4):633–639
de Groot L, Posthumus MD, Kallenberg CG et al (2010) Risk factors and early detection of atherosclerosis in rheumatoid arthritis. Eur J Clin Invest 40:835–842
Kramer HR, Giles JT (2011) Cardiovascular disease risk in rheumatoid arthritis: progress, debate, and opportunity. Arthritis Care Res 63:484–499
Patel RV, Shelling ML, Prodanovich S et al (2011) Psoriasis and vascular disease risk factors and outcomes: a systematic review of the literature. J Gen Intern Med 26:1036–1049
Gelfand JM, Dommasch ED, Shin DB et al (2009) The risk of stroke in patients with psoriasis. J Invest Dermatol 129:2411–2418
Tonetti MS (2009) Periodontitis and risk for atherosclerosis: an update on intervention trials. J Clin Periodontol 36(Suppl 10):15–19
Huck O, Saadi-Thiers K, Tenenbaum H et al (2011) Evaluating periodontal risk for patients at risk of or suffering from atherosclerosis: recent biological hypotheses and therapeutic consequences. Arch Cardiovasc Dis 104:352–358
O’Keefe JH, Carter MD, Lavie CJ (2009) Primary and secondary prevention of cardiovascular diseases: a practical evidence-based approach. Mayo Clin Proc 84:741–757
Cho CH, Qui BS, Bruce IC (1996) Vagal hyperactivity in stress induced gastric ulceration in rats. J Gastroenterol Hepatol 11:125–128
Nada T, Nomura M, Iga A et al (2001) Autonomic nervous function in patients with peptic ulcer studied by spectral analysis of heart rate variability. J Med 32(5–6):333–347
Yukinaka M, Nomura M, Saijyo T et al (2000) Evaluation of autonomic nervous function in patients with essential hypertension complicated with peptic ulcer. J Gastroenterol Hepatol 15:40–44
Van Wagoner ZD, Evans DC, Askegard-Giesmann JR et al (2013) Perforated peptic ulcer in a child with a vagus nerve stimulator for seizure control. Brain Stimul 6:972–973
Cho CH, Ogle CW, Dai S (1976) Acute gastric ulcer formation in response to electrical vagal stimulation in rats. Eur J Pharmacol 35:215e9
Kox M, Pompe JC, Pickkers P et al (2008) Increased vagal tone accounts for the observed immune paralysis in patients with traumatic brain injury. Neurology 70:480–485
Matteoli G, Boeckxstaens GE (2013) The vagal innervation of the gut and immune homeostasis. Gut 62:1214–1222
Macrez R, Ali C, Toutirais O et al (2011) Stroke and the immune system: from pathophysiology to new therapeutic strategies. Lancet Neurol 10:471–480
Angus DC, van der Poll T (2013) Severe sepsis and septic shock. N Engl J Med 369:840–851
Pavlov VA, Tracey KJ (2012) The vagus nerve and the inflammatory reflex—linking immunity and metabolism. Nat Rev Endocrinol 8:743–754
Tracey KJ (2002) The inflammatory reflex. Nature 420:853–859
Tracey KJ (2009) Reflex control of immunity. Nat Rev Immunol 9:418–428
Borovikova LV, Ivanova S, Zhang M et al (2000) Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 405:458–462
Linard C, Marquette C, Clarenc D et al (2005) Acute ileal inflammatory cytokine response induced by irradiation is modulated by subdiaphragmatic vagotomy. J Neuroimmunol 168:83–95
Hawkes CH, Del Tredici K, Braak H (2009) Parkinson’s disease: the dual hit theory revisited. Ann NY Acad Sci 1170:615–622
Braak H, Rub U, Gai WP, Del TK (2003) Idiopathic Parkinson’s disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm 110:517–536
Holmqvist S, Chutna O, Bousset L et al (2014) Direct evidence of Parkinson pathology spread from the gastrointestinal tract to the brain in rats. Acta Neuropathol 128:805–820
Phillips RJ, Walter GC, Wilder SL et al (2008) Alpha-synuclein-immunopositive myenteric neurons and vagal preganglionic terminals: autonomic pathway implicated in Parkinson’s disease? Neuroscience 153:733–750
Svensson E, Horváth-Puhó E, Thomsen RW et al (2015) Vagotomy and subsequent risk of Parkinson’s disease. Ann Neurol 78:522–529
Acknowledgements
This study was supported, in part, by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW106-TDU-B-212-113004); the China Medical University Hospital; the Academia Sinica Taiwan Biobank Stroke Biosignature Project (BM10501010037); the NRPB Stroke Clinical Trial Consortium (MOST 105-2325-B-039-003); the Tseng-Lien Lin Foundation, Taichung, Taiwan; the Taiwan Brain Disease Foundation, Taipei, Taiwan; and the Katsuzo and Kiyo Aoshima Memorial Funds, Japan.
Author information
Authors and Affiliations
Contributions
Wu SC, and Fang CW and Tseng CH conceived and designed the study and wrote the initial draft of the manuscript; Chen WT participated in the study design and conception; Muo CH performed the data analysis and interpretation and was involved in writing the initial draft of manuscript; and Wu SC performed the data analysis and interpretation as well as manuscript drafting and revision.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest related to this study.
Disclosure
This study used the National Health Insurance Research Database established by the National Health Research Institutes with the authorization of the Bureau of National Health Insurance, Ministry of Health and Welfare of Taiwan. The interpretations and the conclusions contained herein do not represent the opinion of the aforementioned agencies and institutions.
Additional information
Guarantor of the article: Shih-Chi Wu.
Rights and permissions
About this article
Cite this article
Fang, CW., Tseng, CH., Wu, SC. et al. Association of Vagotomy and Decreased Risk of Subsequent Ischemic Stroke in Complicated Peptic Ulcer Patients: an Asian Population Study. World J Surg 41, 3171–3179 (2017). https://doi.org/10.1007/s00268-017-4127-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-017-4127-z